Journal scan
A review of 15 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Francis C. The more you know your patient, the better care you can give. 2022.
In my 40-plus years as a clinician, I have found that a strong, empathic physician-patient relationship builds the trust that is fundamental to successful patient care. The best way to achieve that trust is by taking the time to get to know a little more about my patients. Showing that I was interested in them as individuals made our bond stronger, and I am convinced that this resulted in better outcomes.
When we review patient satisfaction surveys, we find that there is always room for improvement. It is convenient to blame low scores on survey sample size and other factors, but the results tend to be consistent and are unlikely to change unless we make a fundamental change.
Patients give us good reviews if we provide an expected level of service: minimizing wait times, treating them with dignity and respect, and providing appropriate therapies. These fall under the heading of customer service and are essential but recognizing patients as individuals and showing interest in their lives beyond their disease exceeds expectations and promotes the excellence we strive for.
Instead, we create faceless “avatars” of patients in the EMR, eg, “Jane Doe is a 63-year-old Black woman with atrial fibrillation.” With copy and paste, this avatar represents the patient in all future encounters and changes only with a birthday or additional diagnoses.
We were taught the importance of the “patient’s story” in medical school, but we seldom use it now. There are many 63-year-old women with atrial fibrillation, but only one who has a granddaughter named Amie who is about to graduate from nursing school. Knowing this not only builds rapport and trust but can also lead to a more personalized treatment plan with better results.
A personal connection with the patient is an important principle in the “art of medicine” and fundamental to the clinician-patient relationship. It establishes the foundation for much of what follows. Engaging in these conversations shows the patient that we see them as more than their diagnosis and contributes to a different level of respect as patients navigate through our impersonal, fast-paced, EMR-driven system.
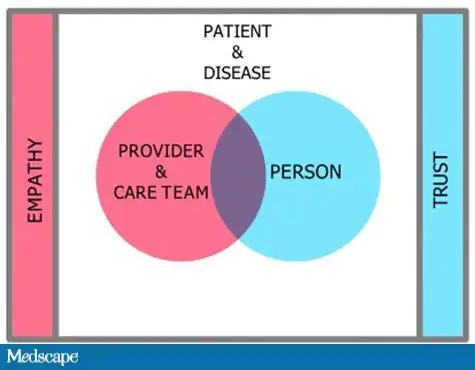
Medical encounters are dynamic and have several players: the care team and clinician; the individual with a disease; and the ever-present computer that takes away essential eye contact. An individual with a disease becomes a patient once there is an association with the caregiver. But association alone is not enough; there must be a connection. Then, and only then, can empathy from the caregiver and trust on the part of the patient develop. The connection may not be complete after the first encounter, and more information may be collected over several encounters
Connection Pause
I recognize that time is an issue, but the following will add very little time to patient encounters.
For new patients, I suggest that we take what I call a “connection pause” before getting into the specifics of their condition. Take 2-4 minutes to sit at the same level as the patient, look them in the eye and talk about things that have little to do with what brought them in to see you: family and living arrangements; occupation; education; and if possible, a little about exercise and hobbies: Do they follow a sports team? Have they ever served in the military?
This will present a clearer picture of the patient and can be included in the visit summary so it’s available to other members of the care team.
The initial conversation should not be forced. An informal give and take may not come naturally to some of us, but it can be learned. Investing in clinical empathy training is money well spent.
Even if you are aware of the pervasiveness and insidiousness of implicit bias, it is still easy to fall into the trap of making assumptions about someone on the basis of their appearance. Personal information about patients can help counter this bias. An added benefit is that knowing our patients on a more human level enriches our lives as well.
It is challenging to empirically evaluate improvement in outcomes through a more personalized approach. My institution is developing plans to gather data to test the hypothesis that time spent on learning more about patients as individuals will lead to greater patient satisfaction and improved patient experience. (I will report on the results in a future blog.)
I decided many years ago that wearing less armor and being more vulnerable would help me take better care of my patients. This meant getting to know more about them; in turn, I allowed them to know more about me. I have never regretted that decision. Less armor and more vulnerability might put the fun back into seeing patients and help counteract burnout.
(2). Sze May Ng. Managing the psychosocial impact of type 1 diabetes in young people. BMJ 2022;377:e070530
https://www.bmj.com/content/377/bmj-2022-070530
What you need to know
Adolescent and young people with type 1 diabetes (T1D) experience higher rates of psychological distress, periods of burnout, and feelings of being unable to cope with the daily burden of living with diabetes, compared with those who are diagnosed as adults
Family, peer, and psychological support and education on living with diabetes can help to reduce distress and improve management of diabetes and wellbeing
Consider using psychological screening assessment tools at diagnosis and annually, and developing appropriate local referral pathways to ensure adequate mental health support
Psychological and behavioural interventions, such as solution focused therapy, coping skills training, motivational interviewing, cognitive behavioural therapy, or family centred interventions aimed at supporting the emotional wellbeing and mental health of people with T1D have shown significant improvements in quality of life and overall management of diabetes
(3). Stuart CG Rison, et al. Investigating hypertension in younger patients. BMJ 2022;376:e067924.
https://www.bmj.com/content/376/bmj-2021-067924
What you need to know
Secondary hypertension may account for up to 30% of diagnoses of young-onset hypertension
Thyroid dysfunction, renal parenchymal disease, and renal artery stenosis secondary to fibromuscular dysplasia are the most common causes of secondary hypertension in younger patients
Testing for 24-hour urinary metanephrines should be carried out only if the patient has phaeochromocytoma symptoms, clinical signs, or relevant family history
Random (spot) serum cortisol tests are usually uninformative. Consider late evening salivary cortisol if available
If treating patients with young onset hypertension empirically, revisit a diagnosis of secondary hypertension following post-treatment blood tests, or if blood pressure control is not achieved or deteriorates
Hypertension is often thought of as a disease of older age, but it occurs across all adult ages, including in younger patients. In the US, 22.4% of people aged 18-39 are estimated to have a blood pressure of above 130/80 mmHg. The 2018 Health Survey for Health for England found that 2.6% of people aged 16-24 and 12.2% of those aged 35-44 had hypertension (on antihypertensive medication and/or blood pressure over 140/90 mmHg). Various guidelines define young onset differently. This article uses the definition in guidelines from the UK’s National Institute for Health and Care Excellence (NICE), which is hypertension in patients under the age of 40.
Essential hypertension remains the most common cause of hypertension, even in young onset hypertension, but secondary hypertension-which has an underlying pathological cause-accounts for 5% to 30% of cases of young onset hypertension. Secondary hypertension is not a diagnosis in itself, but rather a collective term.
(4). Jureidini J. The illusion of evidence-based medicine. BMJ 2022;376:o702.
https://www.bmj.com/content/376/bmj-2021-067924
Evidence based medicine has been corrupted by corporate interests, failed regulation, and commercialisation of academia, argue these authors
The advent of evidence-based medicine was a paradigm shift intended to provide a solid scientific foundation for medicine. The validity of this new paradigm, however, depends on reliable data from clinical trials, most of which are conducted by the pharmaceutical industry and reported in the names of senior academics. The release into the public domain of previously confidential pharmaceutical industry documents has given the medical community valuable insight into the degree to which industry sponsored clinical trials are misrepresented. Until this problem is corrected, evidence-based medicine will remain an illusion.
The philosophy of critical rationalism, advanced by the philosopher Karl Popper, famously advocated for the integrity of science and its role in an open, democratic society. A science of real integrity would be one in which practitioners are careful not to cling to cherished hypotheses and take seriously the outcome of the most stringent experiments. This ideal is, however, threatened by corporations, in which financial interests trump the common good. Medicine is largely dominated by a small number of very large pharmaceutical companies that compete for market share, but are effectively united in their efforts to expanding that market. The short-term stimulus to biomedical research because of privatisation has been celebrated by free market champions, but the unintended, long term consequences for medicine have been severe. Scientific progress is thwarted by the ownership of data and knowledge because industry suppresses negative trial results, fails to report adverse events, and does not share raw data with the academic research community. Patients die because of the adverse impact of commercial interests on the research agenda, universities, and regulators.
The pharmaceutical industry’s responsibility to its shareholders means that priority must be given to their hierarchical power structures, product loyalty, and public relations propaganda over scientific integrity. Although universities have always been elite institutions prone to influence through endowments, they have long laid claim to being guardians of truth and the moral conscience of society. But in the face of inadequate government funding, they have adopted a neo-liberal market approach, actively seeking pharmaceutical funding on commercial terms. As a result, university departments become instruments of industry: through company control of the research agenda and ghostwriting of medical journal articles and continuing medical education, academics become agents for the promotion of commercial products. When scandals involving industry-academe partnership are exposed in the mainstream media, trust in academic institutions is weakened and the vision of an open society is betrayed.
The corporate university also compromises the concept of academic leadership. Deans who reached their leadership positions by virtue of distinguished contributions to their disciplines have in places been replaced with fundraisers and academic managers, who are forced to demonstrate their profitability or show how they can attract corporate sponsors. In medicine, those who succeed in academia are likely to be key opinion leaders (KOLs in marketing parlance), whose careers can be advanced through the opportunities provided by industry. Potential KOLs are selected based on a complex array of profiling activities carried out by companies, for example, physicians are selected based on their influence on prescribing habits of other physicians. KOLs are sought out by industry for this influence and for the prestige that their university affiliation brings to the branding of the company’s products. As well-paid members of pharmaceutical advisory boards and speakers’ bureaus, KOLs present results of industry trials at medical conferences and in continuing medical education. Instead of acting as independent, disinterested scientists and critically evaluating a drug’s performance, they become what marketing executives refer to as “product champions.”
Ironically, industry sponsored KOLs appear to enjoy many of the advantages of academic freedom, supported as they are by their universities, the industry, and journal editors for expressing their views, even when those views are incongruent with the real evidence. While universities fail to correct misrepresentations of the science from such collaborations, critics of industry face rejections from journals, legal threats, and the potential destruction of their careers. This uneven playing field is exactly what concerned Popper when he wrote about suppression and control of the means of science communication. The preservation of institutions designed to further scientific objectivity and impartiality (i.e., public laboratories, independent scientific periodicals and congresses) is entirely at the mercy of political and commercial power; vested interest will always override the rationality of evidence.
Regulators receive funding from industry and use industry funded and performed trials to approve drugs, without in most cases seeing the raw data. What confidence do we have in a system in which drug companies are permitted to “mark their own homework” rather than having their products tested by independent experts as part of a public regulatory system? Unconcerned governments and captured regulators are unlikely to initiate necessary change to remove research from industry altogether and clean up publishing models that depend on reprint revenue, advertising, and sponsorship revenue.
Our proposals for reforms include: liberation of regulators from drug company funding; taxation imposed on pharmaceutical companies to allow public funding of independent trials; and, perhaps most importantly, anonymised individual patient level trial data posted, along with study protocols, on suitably accessible websites so that third parties, self-nominated or commissioned by health technology agencies, could rigorously evaluate the methodology and trial results. With the necessary changes to trial consent forms, participants could require trialists to make the data freely available. The open and transparent publication of data are in keeping with our moral obligation to trial participants-real people who have been involved in risky treatment and have a right to expect that the results of their participation will be used in keeping with principles of scientific rigour. Industry concerns about privacy and intellectual property rights should not hold sway.
(5). Anne-Sophie Claes. Intravascular tumour embolism from chondrosarcoma. Lancet 2022;399(10332):E29.
https://doi.org/10.1016/S0140-6736(16)30382-8
A 48-year-old woman with a history of sternal chondrosarcoma that had been completely resected 3 years previously presented with a 7-month history of cough and progressive dyspnoea. On admission she had blood oxygen saturation of 88%.
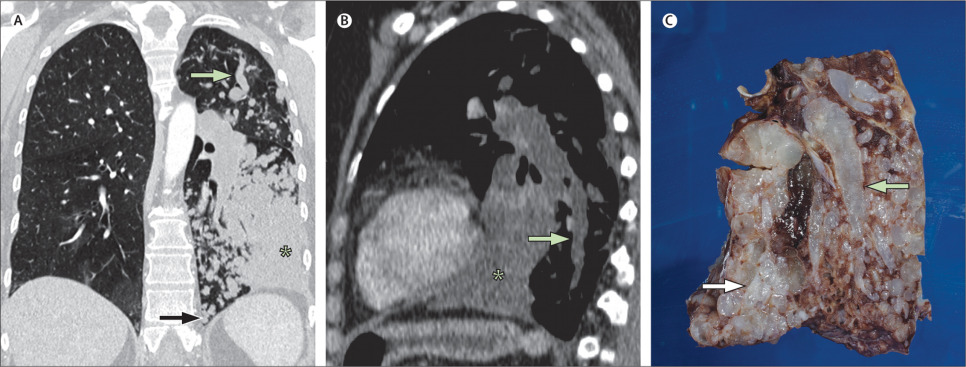
Pulmonary CT angiography showed a large tumour embolus in the main pulmonary artery bifurcation that extended into the left pulmonary artery and all the left lobar and segmental arterial branches and caused a large left lower lobe parenchymal consolidation (figure). Percutaneous transthoracic biopsy of the consolidation showed metastatic chondrosarcoma. She underwent a left pneumonectomy. Macroscopic examination of the resected lung (figure) showed a translucent myxoid tissue filling the pulmonary arteries in an arboreous pattern. Microscopic analysis confirmed that the metastatic chondrosarcoma was confined to the vasculature, even inside the parenchymal consolidation. The patient died 4 months later from respiratory insufficiency from right-sided pleural and pulmonary infection associated with rapid metastatic spread to the right lung.
Pulmonary intravascular tumour embolism is often underdiagnosed at imaging; it is reported in 4-30% of all patients with malignancy on post-mortem examination. It is most common in cancers of the kidney, liver, breast, and lung. Chondrosarcomas are the third most common primary bone malignancy. They often metastasise to the lung parenchyma, but intravascular pulmonary tumour embolism has rarely been reported in chondrosarcoma. Distribution depends on the size of the initial tumour embolus. Small tumour emboli initially lodge distally and propagate towards the centre, gradually affecting larger pulmonary vessels, whereas larger tumour aggregates that embolise in more proximal vessels spread both centrally and peripherally. The clinical signs of pulmonary tumour embolism are variable, and often mimic those of acute or chronic pulmonary thromboembolism; unlike thromboemboli, tumour emboli typically continue to grow despite anticoagulation.
Pulmonary tumour embolism can show various patterns on chest CT (figure). It can present with a tree-in-bud pattern-a pattern that is more commonly seen in other diseases such as bronchiolar inflammation or infection-when small tumour emboli cause filling and dilatation of the small peripheral centrilobular pulmonary arteries, occasionally leading to a pulmonary infarct. The most characteristic appearance of tumour embolism is enlargement of more central beaded pulmonary arteries, caused by larger tumour emboli. Extensive dissemination can also result in parenchymal consolidation, a cause that should be considered in a patient with a known malignancy.
(6). Yoshimura S. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 2022;386:1303-13.
https://www.nejm.org/doi/full/10.1056/NEJMoa2118191
Background
Endovascular therapy for acute ischemic stroke is generally avoided when the infarction is large, but the effect of endovascular therapy with medical care as compared with medical care alone for large strokes has not been well studied.
Methods
We conducted a multicenter, open-label, randomized clinical trial in Japan involving patients with occlusion of large cerebral vessels and sizable strokes on imaging, as indicated by an Alberta Stroke Program Early Computed Tomographic Score (ASPECTS) value of 3 to 5 (on a scale from 0 to 10, with lower values indicating larger infarction). Patients were randomly assigned in a 1:1 ratio to receive endovascular therapy with medical care or medical care alone within 6 hours after they were last known to be well or within 24 h if there was no early change on fluid-attenuated inversion recovery images. Alteplase (0.6 mg per kilogram of body weight) was used when appropriate in both groups. The primary outcome was a modified Rankin scale score of 0 to 3 (on a scale from 0 to 6, with higher scores indicating greater disability) at 90 days. Secondary outcomes included a shift across the range of modified Rankin scale scores toward a better outcome at 90 days and an improvement of at least 8 points in the National Institutes of Health Stroke Scale (NIHSS) score (range, 0 to 42, with higher scores indicating greater deficit) at 48 h.
Results
A total of 203 patients underwent randomization; 101 patients were assigned to the endovascular-therapy group and 102 to the medical-care group. Approximately 27% of patients in each group received alteplase. The percentage of patients with a modified Rankin scale score of 0 to 3 at 90 days was 31.0% in the endovascular-therapy group and 12.7% in the medical-care group (relative risk, 2.43; 95% confidence interval [CI], 1.35 to 4.37; P = 0.002). The ordinal shift across the range of modified Rankin scale scores generally favored endovascular therapy. An improvement of at least 8 points on the NIHSS score at 48 h was observed in 31.0% of the patients in the endovascular-therapy group and 8.8% of those in the medical-care group (relative risk, 3.51; 95% CI, 1.76 to 7.00), and any intracranial hemorrhage occurred in 58.0% and 31.4%, respectively (P < 0.001).
Conclusions
In a trial conducted in Japan, patients with large cerebral infarctions had better functional outcomes with endovascular therapy than with medical care alone but had more intracranial hemorrhages
(7). Raja-Elie EA. Deliberate practice at the virtual bedside to improve clinical reasoning. 2022.
https://www.nejm.org/doi/full/10.1056/NEJMe2204540
A concert pianist plays Chopin’s Nocturne, op. 9, no. 1, for an audience in awe. A trial attorney breaks down the defendant’s arguments without once pausing to consult her bench. A gymnast rips through the air and lands an impossible double-twisting double somersault. An expert clinician makes the elusive diagnosis seconds after listening to a case presentation. Despite performing in very different fields, these professionals followed the same path to expertise: deliberate practice.
The Path to Expertise in Clinical Reasoning.
The acquisition of expertise requires highly motivated, focused repetition combined with specific and timely feedback to hone and perfect performance. Studies have shown that time spent on this particular type of practice, called deliberate practice is a stronger predictor of clinical performance than either academic aptitude or experience.
The pianist and the gymnast can get deliberate practice in an empty hall or gymnasium. The lawyer can do this in her office, with colleagues providing coaching and critique. How and where do clinicians perform deliberate practice to hone the art and science of their own clinical reasoning? The basis for outstanding performance during one’s professional life is built during medical school and residency, but that foundation is not enough to achieve the highest level of performance. A learner requires an average of 10,000 hours of deliberate practice to achieve expert performance. However, the average U.S. residency graduate is likely to complete only 2500 to 3000 hours of deliberate practice in clinical reasoning during the clinical years of medical school and residency. The opportunities for deliberate practice after residency can be even more limited; clinicians seldom have the time to reflect on their clinical reasoning and rarely receive high-quality feedback on their performance.
To build a solid base, students and residents must obtain high-quality and timely feedback as they learn the science and art of clinical reasoning. We all know that assessing trainees and delivering such feedback is challenging when there is a ward full of patients to see. As a result, medical schools and training programs typically rely on end-of-rotation evaluations, objective structured clinical examinations (OSCEs), and multiple-choice examinations of medical knowledge. The feedback provided from end-of-rotation assessments may lack specificity (“great job, read more”), timeliness, and an action plan for improvement. OSCEs can provide specific and timely feedback but are limited in scope and are resource-intensive. Multiple-choice examinations are efficient but account for only a small part of the variance in performance of clinical reasoning. Many medical schools and residency programs lack valid, reliable, and feasible ways to frequently assess performance and to provide high-quality feedback on learners’ clinical reasoning abilities in order to improve their performance. Consequently, the assessment and deliberate practice of clinical reasoning might be viewed as the holy grail of medical education.
In response to these challenges, we have developed a solution to provide learners with deliberate practice of their clinical reasoning skills. NEJM Healer (https://healer.nejm.org. opens in new tab) provides screen-based, interactive patient encounters that expose learners to various clinical problems and disease presentations. During a virtual encounter, learners engage in each step of the clinical reasoning process. Of note, the program assesses the learner’s prioritized differential diagnosis and illness script accuracy (i.e., the similarity between a learner’s valuation of clinical findings that define an illness and that of an expert). The application also offers detailed feedback on problem representations, diagnostic probabilities, and management plans. These features allow trainees to obtain deliberate practice. Detailed, longitudinal, and real-time assessments of clinical reasoning and applied medical knowledge enable the objective measurement of a learner’s areas of strength and the identification of opportunities for growth. Medical schools and postgraduate programs can then provide targeted coaching and remediation with additional NEJM Healer cases or other resources.
A passenger boarding a plane has complete confidence in the flight crew’s skills, thanks to the aviation industry’s culture of lifelong practice and rigorous assessment standards, which rely heavily on simulation. Do our patients share that same confidence during a clinical encounter? Unfortunately, diagnostic errors due to faulty clinical reasoning are all too common, and they cause patient suffering and preventable deaths. 2,4-8 The National Academy of Medicine suggests a multipronged approach to improve diagnosis in medicine, including formal education, training, and assessment of diagnostic reasoning for both trainees and practicing clinicians. High-stakes industries, such as aviation, have used screen-based, simulated deliberate practice for decades. The medical community must follow their lead to enhance the path to expertise in clinical reasoning.
(8). Katsoularis I. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ 2022;377.
https://www.bmj.com/content/377/bmj-2021-069590
What is already known on this topic
It is well known that covid-19 increases the risk of venous thromboembolism
Less evidence exists on the length of time this risk is increased, if risk changed during the pandemic waves, and whether covid-19 also increases the risk of bleeding
What this study adds
The findings of this study suggest that covid-19 is an independent risk factor for deep vein thrombosis, pulmonary embolism, and bleeding, and that the risk of these outcomes is increased for three, six, and two months after covid-19, respectively
This study also found a higher risk of events in patients with comorbidities, patients with more severe covid-19, and during the first pandemic wave compared with the second and third waves
Editorial
Risks are increased even after mild infections
It is now clear from meta-analyses of case series, cohort studies, and self-controlled case series that the risk of venous thromboembolism is increased after SARS-CoV-2 infection. However, two important questions remain: for how long post-infection is the risk increased, and does mild infection also increase risk? In a linked paper, Katsoularis and colleagues (doi:10.1136/bmj-2021-069590) address these questions by applying two complementary study designs to data from several Swedish registries.
The authors identified more than one million people with laboratory confirmed SARS-CoV-2 infection from the start of the pandemic to mid-2021, matched on age, sex, and county of residence to more than four million people who had not had a positive SARS-CoV-2 test result. After adjustment for a wide range of potential confounders, the authors reported a fivefold increase in risk of deep vein thrombosis (relative incidence 4.98, 95% confidence interval 4.96 to 5.01), 33-fold increase in risk of pulmonary embolism (33.05, 32.8 to 33.3), and an almost twofold increase in risk of bleeding (1.88, 1.71 to 2.07) in the 30 days after infection.
The results were largely consistent in alternative analyses using a self-controlled case series approach comparing risk 1-30 days after the infection with a control period. The advantage of this approach is that comparing two periods in the same individual eliminates confounding by factors that are stable over time, such as genetics.
The large study population enabled novel, granular analyses. Previous studies have already shown that the association between SARS-CoV2-2 and thromboembolic events is much stronger for pulmonary embolism than for deep vein thrombosis. Katsoularis and colleagues were able to show that the increased risk of thromboembolism also lasts longer for pulmonary embolism than for deep vein thrombosis; six and three months, respectively.
These authors also report an increased risk of bleeding after SARS-CoV-2 infection that is consistent with previous studies. Use of thromboprophylaxis after SARS-CoV-2 infection clearly carries a risk of bleeding. However, covid-19 has also been associated with coagulopathy and disseminated intravascular coagulation. Although unable to identify the underlying mechanism, the authors show that the association with bleeding is independent of anticoagulation before SARS-CoV-2 infection and lasts for two months after infection.
Since risks of thromboembolism and bleeding were highest among participants with more severe covid-19, vaccination could reduce the overall risk both by preventing infection and by reducing its severity when it does occur. While risk of thromboembolic events is increased after vaccination, the magnitude of risk remains smaller and persists for a shorter period that that associated with infection.
Are the new study findings still relevant now that nearly 65% of the world’s population has received at least one vaccine dose? Yes-current vaccines are highly effective against severe covid-19 but confer only moderate protection against infection with the omicron variant. Breakthrough infections are common, even after a third dose, and effectiveness against symptomatic disease appears to decrease to less than 50% 10 weeks after vaccination.
Although many infections with the omicron variant are mild, the new study confirms an increased risk of venous thromboembolism even among those with milder infections who do not require admission to hospital.
The association was much weaker (relative incidence 5.87, 95% confidence interval 4.88 to 7.05 for pulmonary embolism) than that among patients admitted to hospital (64.49, 53.91 to 77.15) and those admitted to intensive care (196.98, 128.71 to 301.46), but mild disease accounts for a much larger proportion of infections (94.5% in this study). This patient group may therefore contribute a substantial number of thromboembolic events.
A study from England reported a doubling in the incidence of, and mortality from, thromboembolism since the start of the pandemic in 2020 compared with the same periods in 2018 and 2019. The same study reported comparable increases among individuals without positive SARS-CoV-2 test results. Some of those without a positive test result will have been infected before widespread testing was available, but others will have had mild or asymptomatic infections.
Despite the potential for new variants of concern, most governments are removing restrictions and shifting their focus to determining how best to “live with covid.”
Katsoularis and colleagues’ study reminds us of the need to remain vigilant to the complications associated with even mild SARS-CoV-2 infection, including thromboembolism
(9). Ghosh P. Rejuvenation of woman’s skin could tackle diseases of ageing. 2022.
https://www.bbc.com/news/science-environment-60991675
Researchers have rejuvenated a 53-year-old woman’s skin cells so they are the equivalent of a 23-year-old’s.
The scientists in Cambridge believe that they can do the same thing with other tissues in the body.
The eventual aim is to develop treatments for age-related diseases such as diabetes, heart disease and neurological disorders.
The technology is built on the techniques used to create Dolly the cloned sheep more than 25 years ago.
The head of the team, Prof Wolf Reik, of the Babraham Institute in Cambridge, told BBC News that he hoped that the technique could eventually be used to keep people healthier for longer as they grow older.
“We have been dreaming about this kind of thing. Many common diseases get worse with age and to think about helping people in this way is super exciting,” he said.
Prof Reich stressed though that the work, which has been published in the journal eLife, was at a very early stage. He said that there were several scientific issues to overcome before it could move out of his lab and into the clinic. But he said that demonstrating for the first time that cell rejuvenation is possible was a critical step forward.
The origins of the technique stem from the 1990s, when researchers at the Roslin Institute just outside Edinburgh developed a method of turning an adult mammary gland cell taken from a sheep into an embryo. It led to the creation of Dolly the cloned sheep.
The Roslin team’s aim was not to create clones of sheep or indeed humans, but to use the technique to create so-called human embryonic stem cells. These, they hoped, could be grown into specific tissues, such as muscle, cartilage, and nerve cells to replace worn-out body parts.
The Dolly technique was made simpler in 2006 by Prof Shinya Yamanaka, then at Kyoto University. The new method, called IPS, involved adding chemicals to adult cells for around 50 days. This resulted in genetic changes that turned the adult cells into stem cells.
In both the Dolly and IPS techniques, the stem cells created need to be regrown into the cells and tissues the patient requires. This has proved difficult and despite decades of effort, the use of stem cells to treat diseases is currently extremely limited.
Prof Reik’s team used the IPS technique on 53-year-old skin cells. But they cut short the chemical bath from 50 days to around 12. Dr. Dilgeet Gill was astonished to find that the cells had not turned into embryonic stem cells – but had rejuvenated into skin cells that looked and behaved as if they came from a 23-year old.
He said: “I remember the day I got the results back and I didn’t quite believe that some of the cells were 30 years younger than they were supposed to be. It was a very exciting day!”
The technique cannot immediately be translated to the clinic because the IPS method increases the risk of cancers. But Prof Reik was confident that now it was known that it is possible to rejuvenate cells, his team could find an alternative, safer method.
“The long-term aim is to extend the human health span, rather than the lifespan, so that people can get older in a healthier way,” he said.
Prof Reik says some of the first applications could be to develop medicines to rejuvenate skin in older people in parts of the body where they have been cut or burned – as a way to speed up healing. The researchers have demonstrated that this is possible in principle by showing that their rejuvenated skin cells move more quickly in experiments simulating a wound.
The next step is to see if the technology will work on other tissues such as muscle, liver and blood cells.
Prof Melanie Welham, who is the executive chairman of the Biotechnology and Biological Sciences Research Council, which part-funded the research that led to Dolly the sheep, told BBC News that the long-stalled clinical benefits of the technology may not be that far away.
If similar approaches or new therapies could rejuvenate immune cells, which we know become less responsive as we age, then in the future it might be possible to boost people’s response to vaccination as well as their ability to fight infections.”
The big question is whether research efforts in this area would lead to a method of whole-body regeneration, an elixir of youth or an anti-ageing pill. Prof Reik said this idea was not completely far-fetched.
“The technique has been applied to genetically modified mice and there are some signs of rejuvenation. One study showed signs of a rejuvenated pancreas, which is interesting for its potential to tackle diabetes.”
But Prof Robin Lovell-Badge, of the Crick Institute in London, believes that the scientific hurdles between Prof Reik’s result in the lab and even the simplest clinical applications are considerable. Nor does he think it will be a trivial process to translate the rejuvenation process to other types of tissue or indeed an anti-ageing pill.
If you find other chemicals to do the same thing, then that would be good, but they may be just as bad. So, it is ambitious to think you are going to find these chemicals easily and that they are going to be safer.
“It is also quite possible that other types of cells would require different conditions that may be hard to control. And whether you could do it with the whole body safely would be such a long way off, that I would think it would be pure speculation.”
(10). Roxby P. Keep your waist to less than half your height, guidance says. 2022.
https://www.bbc.com/news/health-61021823
An adult’s waist should be less than half their height in order to reduce health risks, the guidance says
People should be encouraged to measure their waist to check they don’t have too much dangerous fat around their middle, updated guidelines say.
An adult’s waist should be less than half their height to reduce health risks, health body NICE recommends.
Measuring body mass index (BMI) is also useful – but doesn’t take into account excess weight around the abdomen.
This increases the risk of conditions such as type 2 diabetes, high blood pressure, heart disease and stroke.
New draft guidance from the National Institute for Health and Care Excellence (NICE) says people from some Asian and black ethnic groups are more prone to this type of fat build-up around the waist, which is called “central adiposity”.
They should use lower BMI thresholds for obesity to help predict their specific health risks.
But NICE warns that even those in a healthy BMI weight category could be carrying too much weight around the waist
If you’re 175 cm (5 ft 9 inches) tall, for example, then your waist measurement should be less than 87.5 cm (34 inches) – or half your height.
Measuring waist-to-height ratio can be used for both sexes and all ethnic groups, as well as highly muscular adults, it adds.
But waist circumference measurements are not accurate in people with a BMI over 35, pregnant women or children under two.
Disease risk
The latest estimates for England suggest that 28% of adults are obese and a further 36% are overweight – a problem that is costing the NHS more than £6bn.
Professor Naveed Sattar, professor of metabolic medicine at the University of Glasgow, said whether this new message gets taken up is “uncertain” but he said it never harms to try “new ways” to get people to think about their health.
Other experts say measuring the waistline doesn’t work for people who are very short or older people over 60 who may have lost height with ageing.
But Professor Rachel Batterham, consultant in obesity, diabetes and endocrinology, who is on the guidelines committee, said: “Increased fat in the abdomen increases a person’s risk of developing several life-limiting diseases including type 2 diabetes and heart disease.
“Waist-to-height ratio is a simple, easy-to-use measure that identifies people who are at increased health risk and would benefit from weight management support to improve their health.”
‘Be sensitive’
In the guidance, GPs and nurses are advised to ask someone’s permission before talking about their weight, and also to “discuss it in a sensitive manner”.
Advice on managing weight is usually tailored to the individual and focuses on improving their diet and getting them to exercise more, in addition to potential treatments and surgery.
Dr Paul Chrisp, director of the centre for guidelines at NICE, said the updated draft guidelines help people understand what factors affect their health and how to address them.
Healthcare professionals and the public can comment on the proposed recommendations in the guidelines before they are published in May.
The updated guidelines say doctors should also consider using waist-to-height ratio in children and young people aged over five to assess and predict health risks.
During the pandemic, there was a substantial rise in obesity in children in England with 25% classed as obese by the time they leave primary school, according to recent NHS data.
Dr Nivedita Aswani, consultant paediatrician specialising in diabetes and weight management at Sheffield Children’s Hospital, said even young children were at risk of the effects of fat in the abdomen.
What is a healthy body mass index (BMI)?
healthy weight: BMI 18.5 to 24.9 kg/m2
overweight: BMI 25 to 29.9 kg/m2
obesity class 1: BMI 30 to 34.9 kg/m2
obesity class 2: BMI 35 to 39.9 kg/m2
obesity class 3: BMI 40 kg/m2 or more
(11). Squair JW. Implanted system for orthostatic hypotension in multiple-system atrophy. N Engl J Med. 2022;386:1339-44.
Orthostatic hypotension is a cardinal feature of multiple-system atrophy. The upright posture provokes syncopal episodes that prevent patients from standing and walking for more than brief periods. We implanted a system to restore regulation of blood pressure and enable a patient with multiple-system atrophy to stand and walk after having lost these abilities because of orthostatic hypotension. This system involved epidural electrical stimulation delivered over the thoracic spinal cord with accelerometers that detected changes in body position.
(12). Aikawa E. The Developmental Origin of Calcific Aortic Stenosis. N Engl J Med. 2022;386:1372-1374.
https://www.nejm.org/doi/full/10.1056/NEJMcibr2200439
Mechanisms of heart-valve disease often mimic processes observed in embryonic and early childhood development, including activation of valvular interstitial cell (VIC) phenotypes and remodeling of extracellular matrix.1 This developmental reprogramming in the mature aortic valve is probably an attempt to repair damaged tissue and restore normal function; however, remodeling responses are notoriously poor in more quiescent adult tissues. The persistence of pathologic stimuli results in accumulation of fibrotic collagen and development of calcific nodules, which compromise the biomechanical integrity of the cusps of the aortic valve and lead to stenosis.
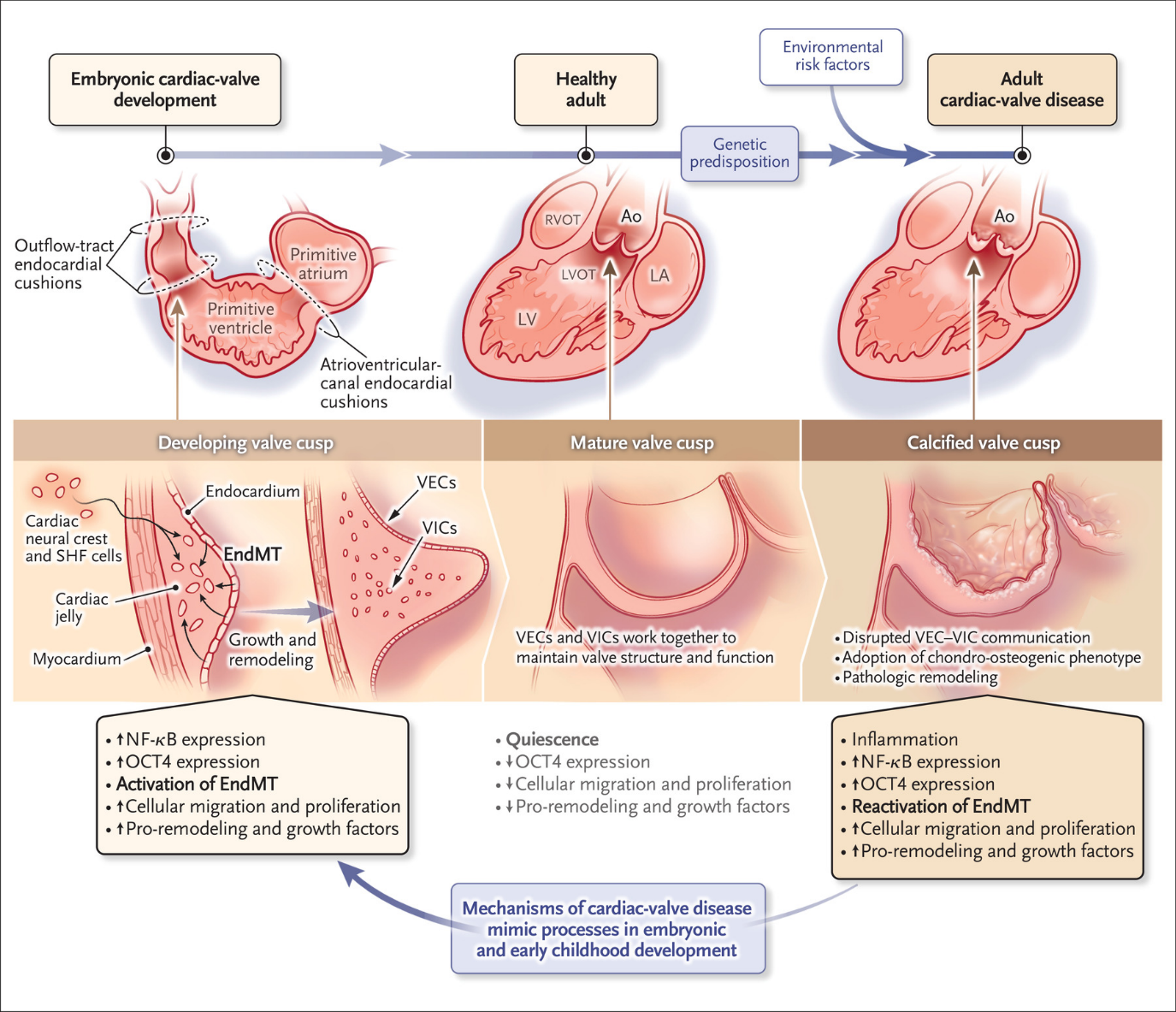
Fig. 1. Potential role of developmental mechanisms in calcific aortic stenosis.
Reactivation of developmental mechanisms may play a critical role in valve-tissue remodeling that leads to aortic stenosis. Genetic risk factors may predispose a person to the development of calcific cardiac-valve disease later in life, and modifiable environmental risk factors may contribute to disease onset and severity. Ao denotes aorta, EndMT endothelial-to-mesenchymal transition, LA left atrium, LV left ventricle, LVOT left ventricular outflow tract, NF-κB nuclear factor κB, OCT4 octamer-binding transcription factor 4, RVOT right ventricular outflow tract, SHF second heart field, VEC valve endothelial cell, and VIC valve interstitial cell.
Potential Role of Developmental Mechanisms in Calcific Aortic Stenosis.
A recent study by Farrar et al.2 showed the relevance of one particular developmental process, endothelial-to-mesenchymal transition, in pathologic aortic-valve remodeling (Figure 1). This process is key during heart-valve development when the endocardial cells that line the outflow tract and cardiac cushions migrate into the underlying tissue and populate aortic-valve cusps with VICs. The cells that remain on the surface and line the mature aortic-valve cusps are known as valve endothelial cells (VECs). VECs and VICs work in concert to maintain aortic-valve structure and function. In response to disrupted communication between VICs and VECs, activation of endothelial-to-mesenchymal transition leads VECs to adopt a chondro-osteogenic phenotype associated with aortic-valve calcification. Farrar et al. show that the chondro-osteogenic VECs that undergo endothelial-to-mesenchymal transition derive from a specific genetic lineage that expresses octamer-binding transcription factor 4 (OCT4, also known as POU5F1), which promotes a progenitor-cell phenotype. OCT4-positive cells are associated with calcification in diseased human aortic valves, and increased OCT4 expression leads to elaboration of proinflammatory cytokines that promote endothelial-to-mesenchymal transition. Once OCT4-lineage cells migrate into the cusps, they express procalcific genes, which suggests an active participation in calcification. Genetic deletion of OCT4 reduced calcification and prevented aortic stenosis in hypercholesterolemic mice, showing a causal relationship between these endothelial-to-mesenchymal transition mechanisms and pathologic remodeling. Beyond implying potential therapeutic benefit in targeting OCT4-associated signaling, these observations may suggest the need to take a new look at developmental pathways in the onset and progression of calcific aortic stenosis.
Several developmental lineages contribute to aortic-valve development, leading to a unique, complex, and underappreciated cellular heterogeneity. In addition to endothelial-to-mesenchymal transition, cells from the neural crest and second heart field populate the developing valve cusps. Alterations in the relative contributions of these developmental lineages during fetal development can change valve structure and lead to malformations such as bicuspid aortic valves.3 Stratification of distinct gene and protein expression patterns in mature cusps – and altered patterns in diseased leaflets – suggests that specific populations of cells maintain the extracellular microarchitecture that dictates valve function.4 However, the exact contribution of each of the three previously described and distinct embryonic lineages to cell phenotypes and extracellular matrix patterning in the mature aortic-valve cusps and associated remodeling in disease remains unclear. Similar to the approaches used by Farrar et al., temporal lineage tracing and single-cell-based analyses from embryonic to adult-onset disease are needed to map developmental contributions to aortic-valve homeostasis and remodeling.
In valve research, developmental and disease studies have most often existed as separate disciplines, but holistic analyses that unify valve development, maturation, and disease could lead to new approaches to the management and treatment of aortic stenosis in patients. The clinical realization of noninvasive therapeutics will require identification of patients before gross remodeling occurs, and valve-replacement procedures are being tested in ongoing studies to determine whether they may provide greater benefit if performed earlier in the course of disease, before cardiac function becomes irreversibly compromised. In many patients, symptom manifestation occurs only in severe stenosis, which limits clinical options that could preserve cardiac function and reduce future complications. Socioeconomic and racial disparities in the reporting of symptoms such as fatigue and dyspnea may also contribute to widening gaps in outcomes for patients with aortic stenosis as new guidelines and interventions require earlier identification of disease. The recognition that developmental factors and reactivation of developmental pathways can contribute to aortic stenosis may provide new insight into individual risks of valve remodeling. Familial analyses suggest a strong genetic contribution to the risk of aortic stenosis.5 Persons with at least one sibling who has aortic stenosis have been found to be at significantly higher risk for the development of aortic-valve disease than those who do not (hazard ratio, 3.4; 95% confidence interval [CI], 2.2 to 5.2). The associated risk was found to increase further when two or more siblings had aortic stenosis (hazard ratio, 32.8; 95% CI, 20.5 to 65.2), whereas the risk associated with a spousal diagnosis of stenosis was modest (hazard ratio, 1.2; 95% CI, 1.1 to 1.3). In some persons, reemergence of developmental mechanisms in disease may reflect a genetic predisposition to aortic-valve remodeling in adulthood. New mechanistic insight into the connections between aortic-valve development and disease could lead to a reevaluation of individual risk assessment and subsequent management of aortic stenosis, which may have its origins at birth.
Potential Role of Developmental Mechanisms in Calcific Aortic Stenosis.
A recent study by Farrar et al.2 showed the relevance of one particular developmental process, endothelial-to-mesenchymal transition, in pathologic aortic-valve remodeling (Figure 1). This process is key during heart-valve development when the endocardial cells that line the outflow tract and cardiac cushions migrate into the underlying tissue and populate aortic-valve cusps with VICs. The cells that remain on the surface and line the mature aortic-valve cusps are known as valve endothelial cells (VECs). VECs and VICs work in concert to maintain aortic-valve structure and function. In response to disrupted communication between VICs and VECs, activation of endothelial-to-mesenchymal transition leads VECs to adopt a chondro-osteogenic phenotype associated with aortic-valve calcification. Farrar et al. show that the chondro-osteogenic VECs that undergo endothelial-to-mesenchymal transition derive from a specific genetic lineage that expresses octamer-binding transcription factor 4 (OCT4, also known as POU5F1), which promotes a progenitor-cell phenotype. OCT4-positive cells are associated with calcification in diseased human aortic valves, and increased OCT4 expression leads to elaboration of proinflammatory cytokines that promote endothelial-to-mesenchymal transition. Once OCT4-lineage cells migrate into the cusps, they express procalcific genes, which suggests an active participation in calcification. Genetic deletion of OCT4 reduced calcification and prevented aortic stenosis in hypercholesterolemic mice, showing a causal relationship between these endothelial-to-mesenchymal transition mechanisms and pathologic remodeling. Beyond implying potential therapeutic benefit in targeting OCT4-associated signaling, these observations may suggest the need to take a new look at developmental pathways in the onset and progression of calcific aortic stenosis.
Several developmental lineages contribute to aortic-valve development, leading to a unique, complex, and underappreciated cellular heterogeneity. In addition to endothelial-to-mesenchymal transition, cells from the neural crest and second heart field populate the developing valve cusps. Alterations in the relative contributions of these developmental lineages during fetal development can change valve structure and lead to malformations such as bicuspid aortic valves.3 Stratification of distinct gene and protein expression patterns in mature cusps – and altered patterns in diseased leaflets – suggests that specific populations of cells maintain the extracellular microarchitecture that dictates valve function.4 However, the exact contribution of each of the three previously described and distinct embryonic lineages to cell phenotypes and extracellular matrix patterning in the mature aortic-valve cusps and associated remodeling in disease remains unclear. Similar to the approaches used by Farrar et al., temporal lineage tracing and single-cell-based analyses from embryonic to adult-onset disease are needed to map developmental contributions to aortic-valve homeostasis and remodeling.
In valve research, developmental and disease studies have most often existed as separate disciplines, but holistic analyses that unify valve development, maturation, and disease could lead to new approaches to the management and treatment of aortic stenosis in patients. The clinical realization of noninvasive therapeutics will require identification of patients before gross remodeling occurs, and valve-replacement procedures are being tested in ongoing studies to determine whether they may provide greater benefit if performed earlier in the course of disease, before cardiac function becomes irreversibly compromised. In many patients, symptom manifestation occurs only in severe stenosis, which limits clinical options that could preserve cardiac function and reduce future complications. Socioeconomic and racial disparities in the reporting of symptoms such as fatigue and dyspnea may also contribute to widening gaps in outcomes for patients with aortic stenosis as new guidelines and interventions require earlier identification of disease. The recognition that developmental factors and reactivation of developmental pathways can contribute to aortic stenosis may provide new insight into individual risks of valve remodeling. Familial analyses suggest a strong genetic contribution to the risk of aortic stenosis.5 Persons with at least one sibling who has aortic stenosis have been found to be at significantly higher risk for the development of aortic-valve disease than those who do not (hazard ratio, 3.4; 95% confidence interval [CI], 2.2 to 5.2). The associated risk was found to increase further when two or more siblings had aortic stenosis (hazard ratio, 32.8; 95% CI, 20.5 to 65.2), whereas the risk associated with a spousal diagnosis of stenosis was modest (hazard ratio, 1.2; 95% CI, 1.1 to 1.3). In some persons, reemergence of developmental mechanisms in disease may reflect a genetic predisposition to aortic-valve remodeling in adulthood. New mechanistic insight into the connections between aortic-valve development and disease could lead to a reevaluation of individual risk assessment and subsequent management of aortic stenosis, which may have its origins at birth.
(13). Sadnicka A, et al. Dystonia. BMJ 2022;377:e062659
https://www.bmj.com/content/377/bmj-2020-062659
What you need to know
Dystonia is a neurological condition characterised by abnormal postures and movements resulting from abnormal neural control of muscles
The most common forms of isolated dystonia in adults are focal, affecting the neck (cervical dystonia), eyes (blepharospasm), or associated with a task (eg, writer’s cramp)
Acute and tardive dystonia can occur as complications of medications such as dopamine receptor blockers.
Neurophysiotherapy, botulinum toxin injections, and deep brain stimulation are effective treatments.
Management of non-motor symptoms such as depression, anxiety, and associated pain are also important.
Dystonia is an abnormality of movement and posture caused by the abnormal neural control of muscle contractions. It is a highly stigmatising long term condition associated with a reduced quality of life. Management is a multidisciplinary partnership between general practitioners, specialists, therapists, and patients and seeks to alleviate motor and non-motor symptoms and the wider psychosocial repercussions of dystonia. This practice pointer highlights the common forms of dystonia, flags rarer causes which can have significant repercussions if not recognised, and offers a clinical roadmap for patient management.
What is dystonia?
Dystonia is defined as “a movement disorder characterised by sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures, or both. Dystonic movements are typically patterned, twisting, and may be tremulous. Dystonia is often initiated or worsened by voluntary action and associated with overflow muscle activation.” A dystonic body part usually remains mobile and movements are often slow and effortful, with a reduced range. The most common forms of dystonia in adults are focal, affecting the neck (cervical dystonia), eyes (blepharospasm), or associated with a task (eg, writer’s cramp). However, dystonia can also present with a generalised pattern, which is more common with childhood onset forms. Dystonia is a subcategory of the hyperkinetic movement disorders in which too much or disordered movement is seen.
(14). Meyerowitz-Katz G, et al. Unethical studies of ivermectin for covid-19. BMJ 2022;377:o917.
Flawed research means we still do not know if the drug is safe or effective
During disease outbreaks, it can be tempting to sacrifice the scientific rigour of research in favour of speed, given the urgency to develop new treatments. After the 2014-16 Ebola outbreak in west Africa, however, a report on the ethics of research from the US National Academy of Medicine stated clearly that “research during an epidemic is still subject to the same core scientific and ethical requirements that govern all research on human subjects.” Early in the covid-19 pandemic ethicists warned researchers against “pandemic research exceptionalism”-lowering ethical standards because of the urgency of the crisis. Despite these warnings, there have been many examples of researchers treating covid-19 as exactly that: an exception to the rigorous standards to which we should hold medical research. There is no better example of such exceptionalism than the research into ivermectin for covid-19.
Ivermectin is used to treat a range of parasitic diseases, including onchocerciasis and helminthiases. On the basis of in vitro activity against SARS-CoV-2,4 the drug was tested as a possible treatment and prevention for covid-19. Initial randomised trials and systematic reviews suggested large benefits from the drug, including reduced hospital admissions and improved survival rates. It turns out that many of the results were-literally-too good to be true.
An analysis of 26 major trials of ivermectin for covid-19 found that over one third had “serious errors or signs of potential fraud.” One prominent meta-analysis that suggested a large survival benefit from the drug was retracted.6 The authors did a re-analysis and found that the effect of ivermectin on survival that they had shown in their retracted study “was dependent on the inclusion of studies with a high risk of bias or potential medical fraud.” The editor of the American Journal of Therapeutics published an expression of concern about another high profile meta-analysis, noting suspicious data in several of the included studies and concluding that “exclusion of the suspicious data appears to invalidate the findings regarding ivermectin’s potential to decrease the mortality of covid-19 infection.”
Ethics scandals
Two recent ethics scandals have cast a further shadow over ivermectin research. First, a report of an experimental study in Mexico City that gave almost 200 000 ivermectin based medical kits to residents with covid-19 was retracted from the preprint server SocArXiv.10 The report was retracted, says SocArXiv’s director, because the experiment was conducted “without proper consent or appropriate ethical protections.”Second, in an experiment in a jail in Arkansas, USA, four incarcerated men developed severe side effects after a physician gave them high dose ivermectin as a supposed covid-19 treatment without their knowledge.The four men are suing the jail.
Lack of consent was not the only ethical violation in these two scandals. The research participants were exposed to a risk of drug side effects without knowing they had been given ivermectin. In Mexico, the failure to give information to the participants infringed on a human right established in Mexico’s constitution: the right to access information. The Arkansas case raises additional concerns as it involved incarcerated people, who risk coercion and exploitation when they are enrolled in clinical research.
It is also arguably unethical and a waste of resources to conduct drug research in an emergency that is of such low quality that no conclusions can be drawn about the drug’s efficacy. That is the situation we find ourselves in today-it is still unclear whether ivermectin is safe or has any benefit in the treatment or prevention of covid-19. The flawed and potentially fraudulent research represents a huge missed opportunity to answer an important research question.
Abandoning research exceptionalism
The pressure to act quickly and do something instead of nothing in a global health emergency can lead researchers to cause harm or add to already existing injustices. But the answer is not to abandon research during crises, which could itself lead to “inadequate, ineffective, or even harmful care.” The answer is to abandon research exceptionalism.
Such exceptionalism is not needed to run fast, informative trials during a pandemic. The Recovery trial, for example, was a collaborative triumph that allowed clinicians quickly and efficiently to discard ineffective treatments such as lopinavir-ritonavir while adopting effective ones such as dexamethasone. The trial started in March 2020 and released its first results in June 2020, finding an effective treatment for covid-19 just 10 weeks after enrolling the first participant while maintaining high ethical standards.
The Nuffield Council on Bioethics has recommended several ways to conduct ethical research even under crisis conditions. These include research teams developing study protocols with input from the local community to ensure that a trial is acceptable. Research funders should require inclusive community engagement plans in all proposals and should collaborate with governments, national research institutions, and multilateral agencies at the start of an emergency to agree research priorities. Research ethics committees must consider “whether the proposed consent processes are the most appropriate and sensitive that they can be in the circumstances.” The urgency of a pandemic is never an excuse for poorly designed studies, ethical misconduct, or the violation of human rights.
(15). Liu D. Calorie restriction with or without time-restricted eating in weight loss. N Engl J Med. 2022;386:1495-1504.
Background
The long-term efficacy and safety of time-restricted eating for weight loss are not clear.
Methods
We randomly assigned 139 patients with obesity to time-restricted eating (eating only between 8:00 a.m. and 4:00 p.m.) with calorie restriction or daily calorie restriction alone. For 12 months, all the participants were instructed to follow a calorie-restricted diet that consisted of 1500 to 1800 kcal per day for men and 1200 to 1500 kcal per day for women. The primary outcome was the difference between the two groups in the change from baseline in body weight; secondary outcomes included changes in waist circumference, body-mass index (BMI), amount of body fat, and measures of metabolic risk factors.
Results
Of the total 139 participants who underwent randomization, 118 (84.9%) completed the 12-month follow-up visit. The mean weight loss from baseline at 12 months was -8.0 kg (95% confidence interval [CI], -9.6 to -6.4) in the time-restriction group and -6.3 kg (95% CI, -7.8 to -4.7) in the daily-calorie-restriction group. Changes in weight were not significantly different in the two groups at the 12-month assessment (net difference, -1.8 kg; 95% CI, -4.0 to 0.4; P=0.11). Results of analyses of waist circumferences, BMI, body fat, body lean mass, blood pressure, and metabolic risk factors were consistent with the results of the primary outcome. In addition, there were no substantial differences between the groups in the numbers of adverse events.
Conclusions
Among patients with obesity, a regimen of time-restricted eating was not more beneficial with regard to reduction in body weight, body fat, or metabolic risk factors than daily calorie restriction.
