A guideline for patients with diabetes mellitus, towards self-assessment of their feet, during the COVID-19 pandemic times – a modified VBNM TTSSSS classification.
VB. Narayana Murthy*, Sathish Manivel, Arul Mozhi Mangai, Kalpana
Department of Plastic and Reconstructive Surgery, Kauvery Hospital, Chennai, India
*Correspondence: vbnmurthy@gmail.com
Background
The advent in India, in 2020, of the calamitous and catastrophic pandemic of COVID-19 called for compulsive changes to be considered in the careful management of the diabetic foot.
Diabetic limb salvage goals of prevention, preservation and protection of the foot from amputation (PPPA) were violently disrupted by the pandemic. The need for reviewing practice guidelines for managing diabetic foot in Indian subjects during the COVID-19 Pandemic became a compelling issue in the context of many challenges that were posed in providing continuity for these vulnerable patients.
With the second wave of the pandemic now in full swing in India in 2021, we have to rethink about how to plan again. What we had planned in 2020 seemed to be the right thing, but never got around to implementing it on a large scale. It is time to rethink.
COVID-19 pandemic, which led to long periods of lock downs, affected delivery of care for non-COVID-19 problems, causing deterioration in status of health of patients and leading to critical states which demanded attention as an emergency. Providing initial advice at home through teleconsultations may help to prevent such an evolution and help to decide who would need a hospital visit, which would not only ease the burden of the doctor at the hospital but also can free the beds.
VBNM TTSSSS [1] classification system has been used to grade the severity of the disease and planning management. This was modified by simplifying the classification to make it easy for the patients to do a self-evaluation. Teleconsultation was arranged after orienting the patient and their care- givers to the tables.
A welcome change observed was acceptance by relatives of tele-diagnosis and tele consent for treatment which led to keeping less serious patients away from hospital, thus avoiding hospital admissions and visits by a specialist to the bed side.
This approach needs to be carefully evaluated to see whether it can possibly be used beyond the lock-down period. Such a totally different approach, with patient-centered technology guiding telemedicine service for appropriate patients, will increase teleconsultations, decrease visits to the out-patient consultations and allow better hospital bed utilization,
Diabetic foot in India amid COVID-19
India is home to about 72.9 million diabetes patients, a number that will rise to about 134 million by 2045, and will make India the second largest contributor to the world’s diabetic load after China [2]. The complications from diabetic foot affects >30% of the diabetic population over 40 years of age. Frequent visits to a diabetic foot center is essential to prevent further complications which may lead to amputations [3]. Healthcare expenditure on diabetic foot care adds up to one-third of total expenditure on diabetes care [3]. Foot complications which may be limb and/or life-threatening need to be promptly recognized, and hospital care needs to be instituted.
COVID-19 pandemic has thrown at us a whole range of hitherto unknown logistical, administrative, social, medical and surgical management issues. Many are related to the lockdown but also to the shift in the priorities in the delivery of service to non-COVID-19 emergency and critical problems. Surgeons dealing with these patients had to rethink the way these patients have to be managed. Modifications to treatment logistics in such demanding times has been a challenge. Home care and tele consultations means the possibility of providing not only care at home and decongesting the much-needed beds for the treatment of COVID-19 patients, but to reassure and provide a sense of confidence to the patient at home.
VBNM TTSSSS (Copyright Office Government of India 24/09/2014) presented in Table 1 stands for Venue time Based Notion in Management of DF, records the status of the foot and all other parameters related to the foot, diabetic status and also the status of the general organ systems of the patient. Points can be added to arrive at a score ranging from 0 to 10 as Grade 0, 11 to 20 as Grade 1, 21 to 25 as Grade 2a and 26 to 30 as Grade 2b [1–6].
Table 1. Venue time-based notion management in diabetic foot
| TTSSSS CLASSIFICATION | ||||||
| (TIP) TIME AT PRESENTATION | TIP 1 Non Acute |
TIP 2 Recurrent (Recurrence after complete healing) |
TIP 3 Persistent (Healing wound) |
TIP 4 Chronic More than 3 months |
TIP 5 Sub Acute 3 weeks – 3months |
TIP 6 Acute, Acute on chronic (acute exacerbation of chronic ulcer) |
| (TYP) TYPE AT PRESENTATION | TYP 1 The normal foot Foot at Risk |
TYP 2 Multiple Sites same foot Bilateral |
TYP 3 Wound Allowed to heal regardless of time (by choice) Inoperable |
TYP 4 Precipitating factors present ill Fitting Shoes |
TYP 5 Infected Tendon Osteomyelitis |
TYP 6 Toe Limb Life threatening Necrotising Fasciits |
| (SSU) STATUS OF THE SKIN, ULCER | SSU 1 Pinkish white (Normal Pinkish white Scar |
SSU 2 Pink Epithelising) Callosity |
SSU 3 White (fungal) White Acute on chronic |
SSU 4 Yellow (Slough) Non infected Non healing ulcer, |
SSU 5 Black (Ischemic) Red Granulating wound |
SSU 6 Pus / Abscess Infected Callus, Burns, footwear/ Shoe bite, acute injury |
| (SF) STATUS OF THE FOOT | SF 1 Normal |
SF 2 Osteoarthropathy Arch collapse |
SF 3 Neuropathy Neuropathy reversed |
SF 4 ischaemia Ischaemia reversed |
SF 5 Neuroischemia Generally non reversible |
SF 6 Severe Charcot Mixed status Critical Limb Ischemia |
| (SDM) STATUS OF DM | SDM 1 Not Known DM |
SDM 2 Pre-diabetes/IGT |
SDM 3 Newly Diagnosed |
SDM 4 Well ControlledHbA1 < 7 |
SDM 5 Poorly controlled HbAiC > 9 |
SDM 6 Ketoacidosis Hyponatremia |
| (SOS) STATUS OF THE ORGAN | SOS 1 Not affected |
SOS 2 HAEMOPOITIC SYSTEM |
SOS 3 HEART |
SOS 4 LUNGS Lung injury ARDS |
SOS 5 KIDNEY Kidney Failure Acute Kidney Failure Chronic |
SOS 6 Multiple Organ system FAILURE |
Illustrative example of a foot with an ulcer. Derivation of a score and a grade.
Diagnosis
The table is populated with the clinical findings. Points are added to get a score and finally a grade for the foot. This patient is diagnosed as – Non-acute foot at risk with ulcer in a toe, multiple callosities bilaterally with arch collapse, poorly controlled DM with no organ system involved- Grade 1. This patient requires elective evaluation in the OP Department at a later time with prior appointment. The patient reassured for footwear; foot care advice also given.
90 % of DM patients belong to this category. These patients are worried and want to be cautious.
A telephonic video conference may or may not be necessary depending on whether it is a new or an old patient. Both feet need to be examined or a photo with proper lighting can be taken and sent for view. They need reassurance and advice on red flags to be looked for. Injuries in any form or perceived wounds need urgent telephonic consultation. These are usually our known patients. DM WITH NO WOUNDS

9Healed wounds mean that the foot is at risk and susceptible for recurrence. The precipitating factors may not be completely absent. Footwear may have to be thought of as well. Worn out footwear and inability to buy new ones during shutdown has to be borne in mind. Teleconsultation should include checking the foot pulses, skin, and a close look into the footwear. Regular foot and nail care has to be done either by the patient or by a health care worker sometime during this period of lockdown. They are also usually our old and known patients. DHEALED WOUNDS
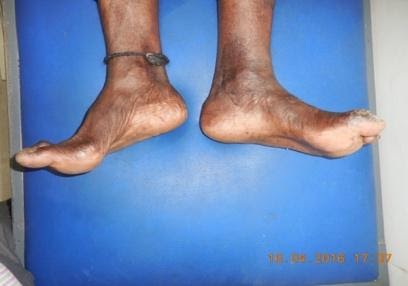
This patient is under treatment for an ulcer. The progress of the wound towards healing is not upto the mark and there are concerns of any deterioration. An initial telephonic consultation and sharing of photos can be done as a preliminary evaluation. These generally may require a visit to the out-patient clinic for further clinical diagnosis and further treatment. Changes to treatment, medications, dressing and any laboratory or imaging may have to be done. Further follow up can be done by health care worker under the supervision of the doctor can be done. The HCW shares photos of the patients. These are usually existing patients on treatment. EXISTING WOUNDS

Rapid worsening of a wound, due to spreading infection. Ischaemia may be there. Redness and discharge from the wounds become more noticeable along with the development of fever and in the presence of other co morbid conditions involvement of other organ systems. Symptoms of COVID-19 infection have to be kept in mind too. Hospital evaluation for foot ulcer and COVID-19 have to be undertaken. These are usually patients seeking new treatment. EMERGENCY WOUNDS

This patient is a classic example of how and why we get these late presentations unfortunately during the COVID-19 pandemic. Severe foot infection precipitated due to delay in seeking medical care. Neuropathy has blunted the pain response and ischaemia has worsened the moderate infection which now has become significant locally and also spread systemically. Renal impairment with early ARDS has been noted in this patient. He needs priority 1 to be managed in an ICU. Difficulty breathing and rapid worsening has to be differentiated from COVID-19 pneumonia and ARDS. CRITICAL LIMB AND LIFE

The recognition of the possibility of this deadly combination has to be kept in mind of the emergency doctor too. Early detection of COVID-19 alerts us to the use of all the necessary steps including isolation, personal protection with adequate protection equipment. Surgical debridement has to be kept to the most radical and just one definitive procedure rather than multiple trips to the operation theater.
Ned for a paradigm shift in treating diabetic foot patients
During a period of containment, as it happened at Wuhan where the pandemic began, many patients would be unable to get admitted to hospitals and diabetic foot clinics and most clinicians would not be organized to provide care at patients’ homes.
Diabetic patients represent a fragile population, a group at increased risk of mortality from COVID-19 [6]. It will be wise to avoid unnecessary diabetes-related hospital admissions to reduce the risk of COVID-19 exposure in the hospitals.
Diabetic foot diseases form a huge spectrum of disorders. Patient centered guidelines have emerged so that these patients are not left behind. Telemedicine can help the patients to get in touch with their regular physician from the comfort of their home, and away from hospitals which could possibly expose them to coronavirus infection. Photos can be shared through mobile phone or email or videos. Need for modification is explained below.
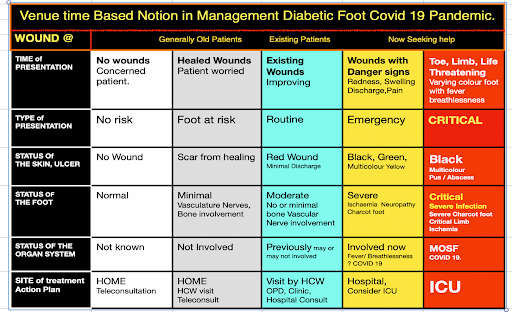
Need for modification of the VBNM classification table for COVID-19 emergency
Patients have to clearly know where do they stand and how to interpret their health concerns during a lockdown. This modification to VBNM, TTSSSS classification has been used to educate the patients to self-interpret looking at their feet at regular or at specific time advised by the health care worker (HCW) or the doctor taking care of the patient.
This modified table is patient centric and relies only on what the patient knows about himself regarding his ulcer, state of foot, diabetic and organ systems. New patients seek advice due to non-availability of their own doctor or for second and tertiary opinion. This table is sent to the patients by WhatsApp and the secretary follows up with instructions on how to interpret the table.
Kindly find below the modified VBNM Classification. The patient looks at the wound at the time of his inspection and interprets the other variables which a doctor normally evaluates in his clinic. We have actually tried to educate the patient, and in a simple way, during this time of crisis. He selects his foot as to which group, he belongs to at the time of presentation. He and the doctor would know if he is an old patient or if he is an existing patient under treatment. We have also had new patients for general or secondary or advanced care of the foot. Patient or his immediate relatives or care givers can see the significant changes to the wound, and his general condition can be derived if they go through the subsequent headings. Status of the foot will be known to our old and existing patients. Changes can be assessed over teleconsultation. They can check each square and if they tend to move towards the right, they are in trouble (Table 2).
Table 2. Venue time-based notion in management diabetic foot COVID-19 pandemic.
Discussion
Existing wounds
Regular photos sent by WhatsApp; progress appraised, home dressings and occasional HCW visit arranged. Progress seen over 22 days. Healing wound, well on the way to healing. Patients and relatives well aware of the classification and signs and symptoms to be observed. A pink and a red wound is now well known as a good sign. Following the color code for observing the nature of the wound and plotting by selecting the boxes in the VBNM table guides them to see if they are moving left or to the right. A move to the right raises red flags to seek help soon.

Critical limb and life threatening
Probably the best example of teleconsultation during the pandemic. An 80-years old man presented with gangrene of toe. Peripheral angiogram showed poor possibility of preserving limb.
Patient at each dressing change desaturated and was in sepsis. All preop checks, investigations, fitness for surgery, organizing the operating schedule and planning for minimal personnel during surgery were done using teleconsultation and teleconference only. Below knee amputation was done. At 48 h patient developed mild fever and hypotension. Photo and teleconsultation reassured that the wound stump was healing well. Movement of specialists and surgeons was avoided during a pandemic and surveillance could be done very effectively remotely. Use of modified table meant what was happening was known to everybody including the relatives. who understood the need for restricted movement of the medical personnel. In normal times, patient’s expectation to be seen by a specialist would be high and often demanding. This was yet important behavior change seen among the relatives.


There are several other excellent examples of such cases managed in a novel, innovative, safe and positive way guided by modified VBNM principles of recording the clinical findings, so that all personnel in the team are on the same page, starting from the patient.
We believe in this mantra that the patient is the most important person in the team. Nowhere is it more important than in these pandemic times. It should be so in the future too. This modified classification puts the patient first. A lot needs to be done to educate him further. This pandemic has given us this opportunity to rethink how we can undertake clinical work in the future. The principle being -prevent, preserve and protect the diabetic feet from amputation, with less travel and visits, keeping patients off hospitals, yet facilitating them to reach hospitals early and seek ICU help at the appropriate time.
Conclusion
This classification formulated by Prof V.B. Narayanamurthy (VBNM) records not only the condition of the foot but also the status of the different types of ulcers among our existing patients, and condition of all the organ systems. This color code Chart is given to all the health care workers and patients who come for evaluation and diagnosis in our center and both the patients and care taker are also trained to complete it. A modification has been done keeping in view the present COVID-19 pandemic situation by recognizing the no risk and at-risk patients. This is a simple table which a patient can use to self-evaluate and present his foot and health status. A preliminary impression of the clinical status of the patient is derived based on a holistic evaluation of the patient. It needs to be seen if this can be used effectively in times after this pandemic.
References
- Narayanamurthy VB. Diabetic Foot Classification – copyright software work. Copyright Office Government of India 24/09/2014
- IDF Diabetes atlas 8th Ed, International Diabetes Federation. 2017. www.diabetesatlas.org
- Rastogi A, Bhansali A. Diabetic foot infection: An Indian scenario. J Foot Ankle Surg. 2016;3:71–79.
- Armstrong DG, Kanda VA, Lavery LA, Marston W, Mills JLS,Boulton AJM. Mind the gap: disparity between research funding and costs of care for diabetic foot ulcers. Diabetes Care. 2013;36:1825–1827.
- Narayanamurthy VB. Sushrutha Professorship Lecture in Plastic Surgery, Royal College of Surgeons of Edinburgh. Lecture – International Confederation of Plastic Surgeons (ICOPLAST 2019) meeting at American Society of Plastic Surgeons (ASPS) Meeting San Diago. CA USA. Sept 2019.
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARSCoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;S2213-2600(20):30079–30075.
