Journal Scan
A review of 20 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Elisabeth Mahase. Study questions relationship between statins and cardiovascular outcomes. BMJ 2022;376:o712
The relationship between the amount that statins reduce low density lipoprotein cholesterol (LDL-C) levels and the risk of death, heart attack, and stroke is “weak or inconsistent,” a review has suggested.
A team of researchers from Australia, Denmark, Ireland, and the US carried out a meta-analysis of 21 randomised clinical trials undertaken between 1987 and 2021 that examined the efficacy of statins for both primary and secondary prevention. The studies were all partially or wholly funded by the pharmaceutical industry.
They reported that their unadjusted analysis “showed only a weak or inconsistent association!”
(2). Emmanuelle AD, et al. Recent advances in the diagnosis and management of cluster headache. BMJ 2022;376:e059577
Cluster headache, a primary headache disorder, consists of short (15-180 minutes), frequent (up to eight a day), unilateral attacks of facial pain with associated ipsilateral autonomic features and restlessness. The attacks are one of the most painful human experiences, and the disorder is associated with a high rate of suicidal ideation. Proper diagnosis is key, as some of the most effective treatments, such as high flow oxygen gas, are rarely used in other headache disorders. Yet diagnostic delay is typically years for this disorder, as it is often confused with migraine and trigeminal neuralgia, and secondary causes may be overlooked. This review covers the clinical, pathophysiologic, and therapeutic features of cluster headache. Recent updates in diagnosis include the redefinition of chronic cluster headache (remission periods lasting less than three months instead of the previous one month), and recent advances in management include new treatments for episodic cluster headache (galcanezumab and non-invasive vagus nerve stimulation).
(3). Partha Kar. To improve clinical leadership in health services, we need a dose of realism. BMJ 2022;376:o651.
One key weakness of Health Services ( HS) is that it may lack strong clinical leadership.
Some may be some good speakers and good motivators, but leaders have to be able to deliver outcomes that matter to patients.
As a leader you should always be judged on the basis of delivery-of outcomes that matter to the people you serve.
Consider the basic question of what draws people to leadership roles. In general, rightly or wrongly, a few factors draw clinicians towards these roles.
Money often isn’t much of a driver towards leadership roles, mainly because the financial rewards are pretty average.
Power and position can be a huge draw. This doesn’t diminish what they can offer: their passion is worth emulating, and there are examples of great care driven by these individuals. Time teaches you that a career position also leads to influence, thereby widening the scope of what one can change or affect.
Which brings us to altruism. For some people it will always play a significant part in attracting them to leadership roles. The problem with altruism as motivation is that it’s not necessarily sustainable. The HS is astounding in its ability to ask those who do a bit more to do a bit more, one more time, and again one more time, for the patients. But every one of us has a limit-and an outside life. At some point the rubber band snaps, and you lose not just the power of that altruism but perhaps also those leaders from the workforce.
But the HS needs clinical leaders.
Leaders may spend too much time describing a shiny new world. That optimism needs balance. It needs realism. It needs stories of leaders failing, of how the first hurdle was the toughest, of how adversity is a part of life in the HS, and of how a lack of resources impedes progress. Otherwise, in the face of the challenges of the real world, disenchantment quickly sets in, and you lose the people who have been inspired to take on leadership roles. Leadership is rewarding, and it can be fun, but it’s also tough and spiked with failure.
The basic fundamental of leadership is: are you representing the needs of the patients and your staff to the higher echelons of power)-or is it the other way around?
The answer should be simple, but in many cases it’s not. And therein sits the basis of leadership success. Or failure.
(4). Yakovenko V, et al. Infective endocarditis and thromboses due to antiphospholipid syndrome following acute Q fever. Lancet 2022;399(10330):p1154.
5 months earlier, the patient had a fever, dyspnoea, and chest pain; he had been seen in the community and a chest CT had shown bilateral dense sub-pleural infiltrates in both lower lobes of the lungs-more on the left. Investigations had found a raised C-reactive protein (CRP) concentration of 18.8 mg/dL (normal 0-0.5). The patient was initially diagnosed and treated for a community acquired pneumonia with oral cefuroxime and roxithromycin with limited clinical response; he was swapped on to oral levofloxacin for a further 14 days. The patient recovered and a CT scan, 1 months later showed almost complete disappearance of the infiltrates.
5 months earlier, the patient had a fever, dyspnoea, and chest pain; he had been seen in the community and a chest CT had shown bilateral dense sub-pleural infiltrates in both lower lobes of the lungs-more on the left. Investigations had found a raised C-reactive protein (CRP) concentration of 18.8 mg/dL (normal 0-0.5). The patient was initially diagnosed and treated for a community acquired pneumonia with oral cefuroxime and roxithromycin with limited clinical response; he was swapped on to oral levofloxacin for a further 14 days. The patient recovered and a CT scan, 1 months later showed almost complete disappearance of the infiltrates.
His medical history was unremarkable, he had no history of travelling abroad, no contact with animals, and he was employed in home renovation.
On examination, we found cyanosis in toes 1 and 5 of his left foot; arterial pulses were detected in the groin but they were absent in the popliteal fossae of both legs. He was afebrile.
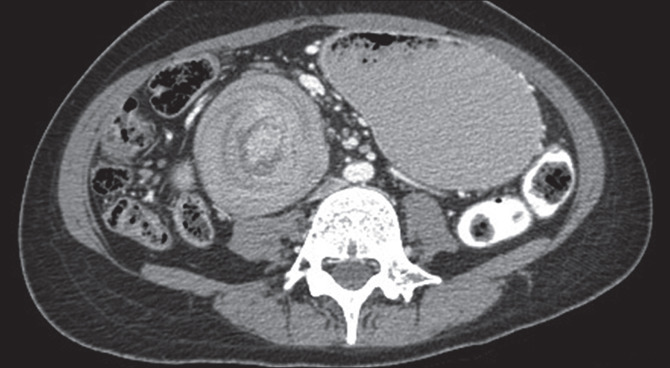
CT-angiography showed filling defects the right kidney and spleen suggesting infarcts and obstructions of the left femoral artery and right popliteal artery (figure). We started low-molecular-weight heparin.
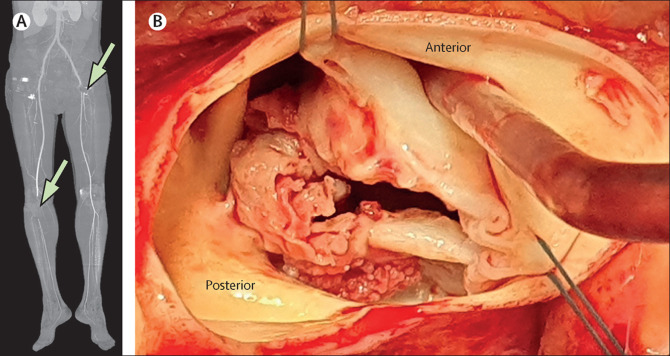
Thrombi were extracted from the left iliac, common femoral and superficial femoral, and the right deep and superficial femoral arteries resulting in the restoration of blood flow to both legs.
Chest CT with angiography also showed large masses on the cusps of the aortic valve and trans-oesophageal echocardiography found a bicuspid aortic valve with masses attached to the aortic and ventricular surfaces of the valve.
Significant laboratory abnormalities included a raised CRP concentration 15.1 mg/dL. Tests for anticardiolipin and anti-β2 glycoprotein 1 antibodies were both strongly positive. Tests for anti-double-stranded DNA and anti-Sm antibodies were negative; blood cultures were also negative.
At operation to replace the aortic valve, large vegetations were found over the left anterior-posterior commissure with destruction of the left aspect of both leaflets (figure). Cultures of samples of the values did not grow organisms but were positive on PCR for Coxiella burnetii; Q fever serology was also positive. We therefore made a diagnosis of antiphospholipid syndrome following Q fever. The patient was treated with doxycycline and hydroxychloroquine; he was allowed home after 8 days. 3 months later, both IgG anticardiolipin antibodies and anti-β2 glycoprotein 1 IgG antibodies remained high. The patient completed an 18-month course of the antibiotics without any further problems.
The diagnosis of antiphospholipid syndrome depends upon the detection of a lupus anticoagulant, or anticardiolipin or anti-β2-glycoprotein 1 antibodies. Acute Q fever can be complicated by antiphospholipid syndrome leading to infective endocarditis with large vegetations and multiple emboli. Thromboembolic events following a pneumonia should prompt investigations for antiphospholipid syndrome; a finding which mandates testing for C burnetii and undertaking echocardiographic studies
(5). Ozelo MC. Valoctocogene Roxaparvovec Gene Therapy for Hemophilia A. N Engl J Med. 2022;386:1013-1025.
Valoctocogene roxaparvovec (AAV5-hFVIII-SQ) is an adeno-associated virus 5 (AAV5)-based gene-therapy vector containing a coagulation factor VIII complementary DNA driven by a liver-selective promoter. The efficacy and safety of the therapy were previously evaluated in men with severe hemophilia A in a phase 1-2 dose-escalation study.
We conducted an open-label, single-group, multicenter, phase 3 study to evaluate the efficacy and safety of valoctocogene roxaparvovec in men with severe hemophilia A, defined as a factor VIII level of 1 IU per deciliter or lower. Participants who were at least 18 years of age and did not have preexisting anti-AAV5 antibodies or a history of development of factor VIII inhibitors and who had been receiving prophylaxis with factor VIII concentrate received a single infusion of 6×1013 vector genomes of valoctocogene roxaparvovec per kilogram of body weight. The primary end point was the change from baseline in factor VIII activity (measured with a chromogenic substrate assay) during weeks 49 through 52 after infusion. Secondary end points included the change in annualized factor VIII concentrate use and bleeding rates. Safety was assessed as adverse events and laboratory test results.
Overall, 134 participants received an infusion and completed more than 51 weeks of follow-up. Among the 132 human immunodeficiency virus-negative participants, the mean factor VIII activity level at weeks 49 through 52 had increased by 41.9 IU per deciliter (95% confidence interval [CI], 34.1 to 49.7; P < 0.001; median change, 22.9 IU per deciliter; interquartile range, 10.9 to 61.3). Among the 112 participants enrolled from a prospective noninterventional study, the mean annualized rates of factor VIII concentrate use and treated bleeding after week 4 had decreased after infusion by 98.6% and 83.8%, respectively (P<0.001 for both comparisons). All the participants had at least one adverse event; 22 of 134 (16.4%) reported serious adverse events. Elevations in alanine aminotransferase levels occurred in 115 of 134 participants (85.8%) and were managed with immune suppressants. The other most common adverse events were headache (38.1%), nausea (37.3%), and elevations in aspartate aminotransferase levels (35.1%). No development of factor VIII inhibitors or thrombosis occurred in any of the participants.
In patients with severe hemophilia A, valoctocogene roxaparvovec treatment provided endogenous factor VIII production and significantly reduced bleeding and factor VIII concentrate use relative to factor VIII prophylaxis.
(6). What Long Covid Shows Us About the Limits of Medicine.
https://www.nytimes.com/2022/03/17/opinion/long-covid.html, March 17, 2022
Long Covid symptoms, such as fatigue, shortness of breath, cognitive difficulties, erratic heart rate, headache and dizziness, can be debilitating and wide-ranging. There is uncertainty about what ultimately causes long Covid and how to adequately respond to it.
In conventional medicine, illnesses without definitive markers of disease are often described as “medically unexplained.” As a medical anthropologist who has studied the controversy over whether treated Lyme disease can become chronic, I’ve been struck by the similarities between long Covid and other contested illnesses like chronic Lyme disease and myalgic encephalomyelitis, more familiarly known as chronic fatigue syndrome.
In conventional medicine, illnesses without definitive markers of disease are often described as “medically unexplained.” As a medical anthropologist who has studied the controversy over whether treated Lyme disease can become chronic, I’ve been struck by the similarities between long Covid and other contested illnesses like chronic Lyme disease and myalgic encephalomyelitis, more familiarly known as chronic fatigue syndrome.
Long Covid has a bigger spotlight than other contested illnesses and was recognized much faster. Post-Covid clinics have been established in nearly every state, the National Institutes of Health have invested $1.15 billion to study it, and it’s now included in the Americans With Disabilities Act. Long Covid has brought increased attention to other marginalized illnesses, along with hope that the needle might finally be moved on overdue research and funding.
At the heart of conventional medicine is a foundational distinction between symptoms and signs. Symptoms like fatigue and joint pain are subjective markers of disease, while signs like fever and arthritis are considered objective markers. Unlike symptoms, signs can be observed and measured by a practitioner, often with the aid of technologies such as blood tests and radiologic imaging.
When it comes to making a diagnosis, signs trump symptoms. This enduring hierarchy can be traced to the late 18th and early 19th centuries in the United States and Europe, when physicians who had relied on external symptoms for diagnosis shifted to a focus on internal anatomy and pathology by using technologies like microscopes. The French philosopher Michel Foucault observed that during that time, medicine transitioned from a practice in which the physician asked, “What’s the matter with you?” to a practice in which the physician asked, “Where does it hurt?” The first question invites a patient’s description of symptoms; the second question leads to a location on the patient’s body that can be observed and measured by the physician.
The diagnostic importance of signs over symptoms was further cemented in the late 1980s and early 1990s with the establishment of evidence-based medicine. It aims to standardize clinical care through guidelines and a pecking order of scientific evidence, with objective evidence of randomized controlled trials at the top and subjective evidence of expert opinion at the bottom. The shift to evidence-based medicine solidified objective evidence as the strongest and most legitimate basis for the diagnosis of disease and reinforced contested illnesses as “medically unexplained,” a term that has often been used to describe physical distress caused by mental illness.
In the same way that conventional medicine prioritizes signs over symptoms, it often prioritizes mortality (risk of death) over morbidity (a diminished quality of life). During interviews, mainstream Lyme disease physicians and scientists often told me that “no one dies from Lyme.” Because Lyme disease is rarely fatal, the thinking goes, there are doubts about the extent to which it compromises the quality of life of those who suffer from it.
The death toll from Covid-19 has been staggering and disproportionate. But medicine’s emphasis on mortality over morbidity has consequences for how suffering is measured as well as the efforts undertaken to prevent disease transmission and the thresholds used for determining when the pandemic is over. If we expand suffering’s metric to include long Covid morbidity, then individual and collective decision making would not only take into account the risk of hospitalization and death but would also include the risk of long Covid.
When patients with contested illnesses don’t find answers in conventional medicine, they often seek out the symptom-centered practices of complementary and alternative medicine. One mainstream Lyme physician I interviewed surmised that although he did not “believe in alternative medicine,” patients’ gravitation toward it was a result of conventional medicine’s “failure to treat the symptoms that they have.” Validating patients’ symptomatic experience, even if the cause is unknown, is one possible remedy.
Patients with contested and chronic illnesses also tend to have long medical histories. These patients need longer than 15 minutes to tell their story, and providers need more than 15 minutes to listen to them. A broad-scale investment in primary care that would allow providers to offer longer appointments that are fully covered by insurance would help to address this need. Additionally, medical schools should introduce a social science-informed understanding of contested illnesses. Despite seeming marginal, “medically unexplained” illnesses are actually some of the most frequently seen conditions in primary care. The more familiar physicians are with these illnesses, the fewer opportunities there will be for misunderstanding.
“Acknowledging uncertainty” – what long Covid patients have called for – is a fitting refrain for our times. As much as they wanted answers, the Lyme patients I interviewed also wanted physicians who could admit what they didn’t know. Starting with what we don’t know – and leading with humility and empathy – seems like a good place to begin.
(7). Warnock S, et al. Inpatient Management of Type 2 Diabetes. JAMA Intern Med. 2022.
A middle-aged man with a history of decompensated cirrhosis with ascites and non-insulin-dependent type 2 diabetes with a hemoglobin A1c level of 6.9% (to convert to the proportion of total hemoglobin, multiply by 0.01) 2 months prior was admitted to the hospital for altered mental status and hyponatremia. On admission, his home metformin use was temporarily halted and sliding scale insulin (SSI) was ordered, with finger stick blood glucose (FSBG) checks at breakfast, lunch, dinner, and bedtime (QACHS). The patient’s mental status improved with treatment with lactulose, and he was eating full meals by hospital day 2. During these 2 days, he was found to have an FSBG level of greater than 180 mg/dL (to convert to mmol/L, multiply by 0.0555) only once. However, while the hyponatremia improved and the patient awaited acceptance to the rehabilitation department, his SSI order was maintained for an 8-day hospitalization, resulting in 30 FSBG checks that ranged from 100 mg/dL to 180 mg/dL without the need for treatment with insulin to maintain a target of 140 mg/dL to 180 mg/dL. Because many patients are treated without insulin, this raised the question: could we spare these patients from frequent FSBG checks?
Teachable Moment
Various observational studies have demonstrated an association between hyperglycemia and poor clinical outcomes. However, to our knowledge, randomized clinical trials have not demonstrated a benefit from intensive vs conservative glycemic control, but have shown increases in mortality and severe hypoglycemia with more aggressive therapy. This has led to the American Diabetes Association (ADA) recommendation for a conservative approach to inpatient glycemic treatment.
The ADA guidelines for inpatient diabetes treatment state that “insulin therapy should be initiated for treatment of persistent hyperglycemia starting at a threshold ≥180 mg/dL (10.0 mmol/L). Once insulin therapy is started, a target glucose range of 140-180 mg/dL (7.8-10.0 mmol/L) is recommended for the majority of critically ill and noncritically ill patients.” When initiating treatment with insulin, long-acting basal insulin plus SSI should be ordered, while standing mealtime short-acting insulin can be added for patients with reliable oral intake. Although the ADA provides clear recommendations on when and how to administer treatment with insulin, to our knowledge there is no standard approach to FSBG monitoring for patients with non-insulin-dependent diabetes who do not meet the persistent hyperglycemia threshold for insulin administration. With 10% of the US population with a diagnosis of type 2 diabetes, eliminating unnecessary FSBG monitoring is not only patient centered and can improve the patient experience, but also has the potential to prevent a waste of medical resources, nursing, and staff time.
One approach to high-value FSBG monitoring is highlighted in a quality improvement project at New York Methodist Hospital (Brooklyn, New York) in which the Yale Diabetic Center recommendations for inpatient diabetic management were used to reduce unnecessary FSBG checks. First, an order set rule was placed that required all patients not in the intensive care unit in the main medical segments of the hospital to receive a definitive diagnosis of diabetes for QACHS finger sticks to be ordered. Daily education was then provided to reduce the frequency of finger sticks to twice daily if the patient was stable with well-controlled blood glucose levels without SSI requirements after 48 hours. The number of finger sticks decreased from nearly 275 000 per year to 238 187 during the year after intervention. Additionally, a study at Mount Sinai Medical Center (Chicago, Illinois) on FSBG monitoring found that an estimated 4 to 10 minutes of staff time was required to go to a patient’s room and complete a single FSBG.5 Taken together, these projects highlight the potential of improving patient care by reducing the frequency of an uncomfortable test, as well as the use of hospital supplies and nursing/staff time.
Using the ADA guidelines and the previously mentioned approach, there can be a refocus on the patient for reevaluation of diabetes management. Given the comorbidities and altered mental status, temporarily halting metformin use on admission and administering QACHS finger sticks would have been appropriate. With only 1 FSBG value of greater than 180 mg/dL in his first 48 hours of hospitalization and a stable medical condition, the FSBG checks could have been reduced to twice daily, which would have spared the patient from 12 finger sticks and saved nursing staff 48 to 120 minutes during the last 6 days of hospitalization. An alternative strategy would be to discontinue FSBG checks entirely if no treatment with insulin was indicated during the first 48 hours with a plan to resume monitoring if a subsequent metabolic panel identified a glucose level greater than 180 mg/dL or if there was a substantial change in clinical status.
Moving forward, patients receiving non-insulin-based regimens for type 2 diabetes who are admitted to the hospital should first be evaluated with FSBG checks to determine the need for treatment with insulin. If the threshold for the initiation of insulin is not met after 24 to 48 hours, or if stability is achieved while receiving basal dosing, finger sticks may be reduced in frequency. Additional studies should focus on patient outcomes of less frequent FSBG monitoring and investigate additional strategies for reducing FSBG checks. This patient-centered approach may help reduce waste while optimizing diabetes management in the inpatient setting.
(8). Alsagaff MY, et al. Diagnostic Dilemma of Pericarditis Concurrent With ST Elevation Myocardial Infarction. JAMA Intern Med. 2022.
A 57-year-old man presented to the emergency department with persistent diffuse ST elevation (STE) after failed treatment with streptokinase therapy that was administered the day prior (the onset of chest pain to lytic bolus was 8 hours). The pain was persistent, radiated to the back, and was exacerbated by coughing. He had normal blood pressure (100/60 mm Hg), mild dyspnea with bibasilar rales (22 breaths per minute), elevated jugular venous pulse, and pericardial friction rub.
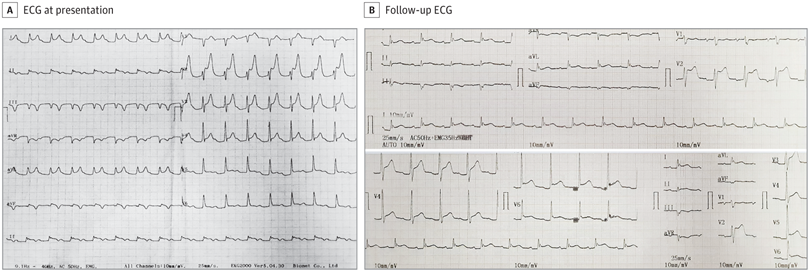
Fig. Serial 12-Lead Electrocardiogram (ECG), (A) The ECG demonstrated sinus tachycardia, diffuse ST-segment elevation (except leads III and V1), knuckle sign in aVR (PR-segment elevation and ST-segment depression), and a prolonged PR-segment interval (280 milliseconds). (B) The ECG recordings performed 24 hours after rescue percutaneous coronary intervention demonstrated sinus rhythm, a return to baseline of the ST-segment elevation with a new Q wave in the inferior leads (II, III, aVF), PR-segment depression, knuckle sign in aVR, and the persistence of ST-segment elevation and an upright T wave in the anterolateral leads (V2-V6, lead I, and aVL).
Question: What ECG characteristics help distinguish STE myocardial infarction (STEMI) from the simultaneous occurrence of pericarditis and STEMI?
Interpretation
The ECG indicated diffuse STE in most leads and knuckle sign (PR-segment elevation and ST-segment depression in aVR) (Figure, A). Laboratory test results revealed elevated levels of cardiac troponin (0.46 ng/mL [to convert to μg/L, multiply by 1]; reference value, 0.001 ng/mL), leukocytes (27 X 103/μL [to convert to ×109/L, multiply by 0.001]), and C-reactive protein (2.0 mg/dL [to convert to mg/L, multiply by 10]; reference value, <10 mg/L). Transthoracic echocardiography (TTE) demonstrated minimal-to-moderate pericardial effusion (PE) and regional wall motion abnormalities in the inferior and posterior regions. Diagnostic coronary angiography was performed because of persistent chest pain, and the progression of ECG features to an intermittent total atrioventricular (AV) block (TAVB). Critical stenosis (99% diameter) of the distal right coronary artery (RCA) and moderate-to-high critical calcified stenosis (99% diameter) of the proximal left circumflex artery (LCX) with grade 2 collaterals from the distal left anterior descending artery were observed. No signs of thrombus or plaque rupture were detected. The obstruction was recanalized with balloon angioplasty followed by use of drug-eluting stents to the RCA and LCX to achieve acceptable angiographic results. Inferior STEMI with pericarditis was diagnosed. The patient was treated with high-dose aspirin (750 mg, 3 times a day), colchicine (0.5 mg, once daily), ticagrelor, furosemide, ramipril, atorvastatin, and lansoprazole. The follow-up ECG after rescue percutaneous coronary intervention revealed a return to baseline of the STE with a new Q wave in the inferior leads, PR-segment depression, knuckle sign in aVR, and persistence of STE and an upright T wave in the anterolateral leads (Figure, B). The patient recovered and was discharged on the fifth day.
Discussion
The ST-segment changes observed in patients with STEMI and pericarditis may present a diagnostic dilemma for emergency physicians. Furthermore, pericarditis may complicate the course of myocardial infarction (MI), and, in this case, pericarditis might mask the STEMI-derived need for reperfusion. The working diagnosis of pericarditis in this case was made based on diffuse STE, pericardial friction rub, and PE. However, the patient’s complaints of chest pain were confusing. Although chest pain is one of the most common symptoms of pericarditis, it may be occasionally difficult to use this factor to differentiate pericarditis from MI, especially if there is pericarditis-associated myocardial involvement. In this case, the elevated troponin I level, regional wall motion abnormalities, transient TAVB, and critical stenosis in the LCX and RCA ultimately led to the diagnosis of inferior STEMI with pericarditis.
Electrocardiography is the mainstay of the initial diagnosis of pericarditis or MI. In contrast to STEMI, pericarditis is characterized by diffuse and concave STE in most or all precordial and limb leads. There was no reciprocal ST-segment depression and no abnormal Q waves. In addition, the T wave in pericarditis displays normal morphology and may be inverted after a variable period (weeks or months). Other essential clues of pericarditis include PR-segment depression in most leads and knuckle sign in aVR.
By contrast, the STE in STEMI usually displays a convex morphology and appears according to the anatomical groupings, which correspond to the vascular territory of infarction. Nevertheless, a less specific concave morphology can also be observed. Moreover, reciprocal ST-segment depression in opposing leads has high diagnostic specificity for STEMI. In inferior MI, the conduction disturbance can cause transient sinus bradycardia and TAVB, because the sinoatrial node, AV node, and his bundle are primarily supplied by the RCA.7 Such weakening of electrical activity in the infarcted myocardium decreases the R wave amplitude. When myocardial cells are no longer active, as in the case of extensive infarction, only the activity of opposing areas appears in the ECG as Q waves.
In the case described in this article, the diffuse and concave STE in the anterior leads led to the diagnosis of pericarditis. However, the convex STE, different evolution of T and Q waves in the inferior leads, and conduction disturbance resulting in intermittent TAVB might indicate inferior STEMI. When STEMI and pericarditis occur together, the typical ECG changes observed in pericarditis are often overshadowed by STEMI-associated changes. However, a persistently elevated ST-segment with persistent upright T waves or early gradual reversal of inverted T waves may aid in the early recognition and diagnosis of pericarditis (sensitivity, 100%; specificity, 77%) (Figure, B). Concurrent STEMI and pericarditis present a further diagnostic challenge because no ECG criteria exist to confirm this condition. Therefore, the final diagnosis depends on the clinical context and additional supporting findings.
Transthoracic echocardiography aids in the diagnosis of pericarditis and STEMI. This technique can differentiate between these 2 diagnoses by excluding PE and regional wall motion abnormalities that match the distribution of coronary blood flow. However, the absence of PE does not rule out pericarditis, as it may only occur in 60% of cases.2 Regional wall motion abnormalities support the diagnosis of MI when co-occurring with increased cardiac troponin levels.9 Troponin elevation is seen in patients with myocardial involvement that is caused by pericarditis (perimyocarditis) and MI. Differentiating perimyocarditis and STEMI might be challenging because both share elevated levels of cardiac markers, regional wall motion abnormalities, conduction disturbance, and STE. To confirm the diagnosis of perimyocarditis, diagnostic coronary angiography is required to exclude coronary occlusion. Cardiovascular magnetic resonance imaging is also recommended to verify myocardial involvement and rule out ischemic myocardial necrosis in the absence of substantial coronary disease. Lastly, an endomyocardial biopsy is necessary for definitive confirmation of perimyocarditis.
Take-home Points
ST elevation myocardial infarction and pericarditis may occur together.
In most cases, ECG, TTE, and cardiac markers may help in differentiating acute pericarditis from STEMI.
In cases of pericarditis with suspected myocardial involvement, invasive coronary angiography is recommended to exclude STEMI diagnosis.
(9). Kissling S. Concomitant Urinary Triple Phosphate and Cystine Crystals. N Engl J Med. 2022;386:1165.
A 37-year-old man with cystinuria was seen in the nephrology clinic for routine follow-up. He had received a diagnosis of cystinuria at 1 year of age, when he had presented with nephrolithiasis and pyelonephritis; subsequent workup had shown elevated 24-hour cystine urinary excretion and homozygous variants in the gene SLC3A1. Since then, he had been treated with urinary alkalinization, high fluid intake, and tiopronin. At the current presentation, he was asymptomatic. The serum creatinine level was normal, and a urinalysis showed a pH of 7.0, with no hematuria or bacteriuria.
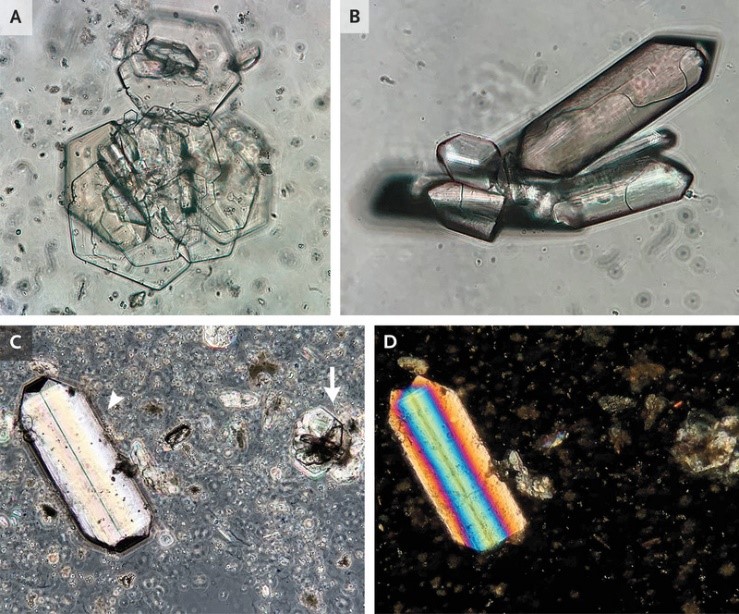
Microscopic examination of a spun urine specimen showed hexagonal cystine crystals (Panel A) and rhombohedral triple phosphate – or struvite – crystals (Panel B). In the same field of view elsewhere in the specimen (Panel C), triple phosphate crystals of a different shape (arrowhead) and cystine crystals (arrow) were seen. Under polarized light, these triple phosphate crystals showed polychromatic properties, and the cystine crystals showed moderate polarizing properties (Panel D). Triple phosphate crystals are associated with urease-producing organisms. The patient had been treated for urinary tract infection 2 weeks before this presentation, but the causative organism had been unknown. At follow-up 1 month later, the patient had no recurrent symptoms of urinary tract infection.
(10). Jarvis, JN, et al. Single-Dose Liposomal Amphotericin B Treatment for Cryptococcal Meningitis. N Engl J Med. 2022;386:1109-1120.
Background
Cryptococcal meningitis is a leading cause of human immunodeficiency virus (HIV)-related death in sub-Saharan Africa. Whether a treatment regimen that includes a single high dose of liposomal amphotericin B would be efficacious is not known.
Methods
In this phase 3 randomized, controlled, noninferiority trial conducted in five African countries, we assigned HIV-positive adults with cryptococcal meningitis in a 1:1 ratio to receive either a single high dose of liposomal amphotericin B (10 mg per kilogram of body weight) on day 1 plus 14 days of flucytosine (100 mg per kilogram per day) and fluconazole (1200 mg per day) or the current World Health Organization-recommended treatment, which includes amphotericin B deoxycholate (1 mg per kilogram per day) plus flucytosine (100 mg per kilogram per day) for 7 days, followed by fluconazole (1200 mg per day) for 7 days (control). The primary end point was death from any cause at 10 weeks; the trial was powered to show noninferiority at a 10-percentage-point margin.
Results
A total of 844 participants underwent randomization; 814 were included in the intention-to-treat population. At 10 weeks, deaths were reported in 101 participants (24.8%; 95% confidence interval [CI], 20.7 to 29.3) in the liposomal amphotericin B group and 117 (28.7%; 95% CI, 24.4 to 33.4) in the control group (difference, −3.9 percentage points); the upper boundary of the one-sided 95% confidence interval was 1.2 percentage points (within the noninferiority margin; P<0.001 for noninferiority). Fungal clearance from cerebrospinal fluid was −0.40 log10 colony-forming units (CFU) per milliliter per day in the liposomal amphotericin B group and −0.42 log10 CFU per milliliter per day in the control group. Fewer participants had grade 3 or 4 adverse events in the liposomal amphotericin B group than in the control group (50.0% vs. 62.3%).
Conclusions
Single-dose liposomal amphotericin B combined with flucytosine and fluconazole was noninferior to the WHO-recommended treatment for HIV-associated cryptococcal meningitis and was associated with fewer adverse events.
(11). Kristi L. Watterberg, et al. Hydrocortisone to Improve Survival without Bronchopulmonary Dysplasia, a Visual abstract. N Engl J Med. 2022;386:1121-1131.
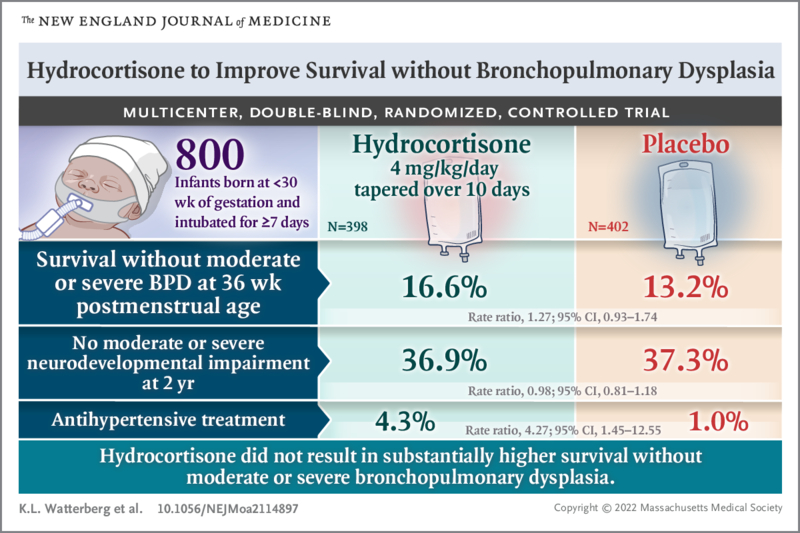
Glucocorticoids might prevent bronchopulmonary dysplasia in extremely preterm infants but have adverse neurodevelopmental effects. In this trial involving preterm infants, there was little difference in survival without bronchopulmonary dysplasia or in the occurrence of neurodevelopmental impairment with hydrocortisone as compared with placebo
(12). Mahase E. Covid-19: What do we know about the delta omicron recombinant variant? BMJ 2022;376:o792.
A combination of the delta (AY.4) and BA.1 omicron variants has been named by the World Health Organization as the BA.1 x AY.4 recombinant. First detected in France in January 2022, it has since picked up the nickname “deltacron”
How does a recombinant emerge?
Recombinants can emerge when multiple variants infect the same person at the same time, allowing the variants to interact during replication, mix up their genetic material, and form new combinations. These events become more likely when cases are higher-an important consideration, as covid-19 cases worldwide have once again started to rise after several weeks of decline.
Maria Van Kerkhove, the World Health Organization’s covid-19 technical lead, said in a post on social media, “[This is] what happens when we allow the virus to circulate at such an intense level. The virus continues to evolve and more variants are expected. Recombinants are also expected …. as we have been explaining for a very long time.”
She emphasised that vaccines alone could not be used to control the SARS-CoV-2 pandemic but that other measures were also needed, while testing and sequencing around the world were vital.
What do we know about “deltacron”?
So far, very little. The literature on deltacron is sparse, although a perspective published by the Chinese Center for Disease Control and Prevention has provided some insight.4 The researchers have reported that the recombinant is very similar to the delta (AY.4) variant except when it comes to the region encoding the spike gene, which is similar to BA.1. Of the 36 amino acid mutations found in the spike protein, 27 were found in BA.1 and five in AY.4, while four were found in both.
The authors have also highlighted that while this is not the first recombination event identified in SARS-CoV-2, and while some have even seen a small amount of community transmission, no previous events have involved such large genomic fragments. As such, the authors said that the emergence of the BA.1 x AY.4 recombinant could be a cause for concern.
They warned, “Although the emergence and subsequent spread of variants of concern has had a huge impact on global health and economy, it may not have been the worst case until now, as recombination (a major mechanism bringing genetic diversity to coronaviruses) has not really emerged on a large scale and shown its power before the emergence of ‘deltacron.’
“The emergence of ‘deltacron’ is therefore a ‘grey rhino’ [an obvious threat that has been ignored or played down] rather than ‘black swan’ [an unlikely but extremely serious] event . . . With the advent of ‘deltacron,’ further concerns are coming.”
On the other hand, a preprint released through medRxiv suggested that delta and omicron coinfections and recombination events were still rare.5 Researchers sequenced 29 719 positive samples taken from November 2021 to February 2022, when delta and omicron were co-circulating in the US. They found 20 coinfections and two independent cases of infection by a delta-omicron recombinant virus. They concluded that these recombinants were rare and that there was currently no evidence that those identified in this study were more transmissible than the omicron lineages already circulating (BA.1, BA.2).
Shishi Luo, lead author and a senior bioinformatics scientist at the genomics company Helix, told The BMJ, “We haven’t seen any evidence for concern for either of the recombinants reported in our study. However, given that these recombinants are being identified at around the same time around the world, we should definitely be increasing our ability to monitor and track them.”
Speaking to The BMJ, Eric Topol, professor of molecular medicine at the Scripps Research Institute in California, echoed the message that while this recombinant may not pose a threat, it could be a warning of what is to come.
“There have been at least three different ‘deltacron’ variants identified now,” he said. “Our concern about them is tempered by lack of evidence that any of these have spread potential or signs of increased virulence. But their appearance emphasises the potential for these recombinant, fusion, hybrid occurrences.
“At the same time, more simultaneous coinfections of variants are being recognised, and there’s also the potential of these occurring in animal reservoirs, or like with bird flu-influenza, a recombinant between humans and animals harbouring SARS-CoV-2.”
(13). Stuart CG Rison, et al. Investigating hypertension in younger patients. BMJ 2022;376:e067924
What we need to know
- Secondary hypertension may account for up to 30% of diagnoses of young onset hypertension
- Thyroid dysfunction, renal parenchymal disease, and renal artery stenosis secondary to fibromuscular dysplasia are the most common causes of secondary hypertension in younger patients
- Testing for 24 hour urinary metanephrines should be carried out only if the patient has phaeochromocytoma symptoms, clinical signs, or relevant family history
- Random (spot) serum cortisol tests are usually uninformative. Consider late evening salivary cortisol if available
- If treating patients with young onset hypertension empirically, revisit a diagnosis of secondary hypertension following post-treatment blood tests, or if blood pressure control is not achieved or deteriorates
(14). Dalbye R, et al. Two midwives during the second stage of labour to reduce severe perineal trauma. 2022;399(10331):P1203-1205.
The reported incidence of the most severe form of perineal trauma-obstetric anal sphincter injury-varies greatly; however, estimates from WHO suggest a global incidence of 4.0-6.6% from all vaginal deliveries. Obstetric anal sphincter injury is of major concern for women because it is associated with an increased risk of pelvic floor disorders, such as anal incontinence, urinary incontinence, pelvic organ prolapse, and sexual dysfunction. Pelvic floor disorders restrict women in their daily activities and have a negative impact on their quality of life. Because the prevalence of pelvic floor disorders increases with increasing age, their cost is expected to rise due to an ageing population, with direct and indirect costs of pelvic floor disorders related to medical expenses and loss of productivity. Furthermore, a tenth of obstetric claims in the UK involves perineal trauma, including obstetric anal sphincter injury. The cost of these claims in the period 2000-10 was more than £31 million. Thus, improving the health and well-being of women giving birth is important on a personal level as well as a societal level. The prevention of obstetric anal sphincter injury during delivery, particularly through perineal support during crowning of the fetal head, is a priority for all midwives and obstetricians.
(15). Hassan R. Extraskeletal Ewing sarcoma of the duodenum presenting as duodenojejunal intussusception. Lancet 2022;399(10331):P1265.
A 25-year-old woman presented to our hospital with a 2-week history of persistent vomiting, abdominal distension, and weight loss.
4 months earlier, she had presented to the local district hospital because her work colleagues had thought she looked pale. The patient had been found to be anaemic with a haemoglobin concentration of 4.7 g/dL and a peripheral blood smear suggestive of a hypochromic microcytic anaemia. She had no other medical history. She was transfused 2 units of blood; she was investigated at the outpatient clinic but was not referred for endoscopic assessment.
4 months earlier, she had presented to the local district hospital because her work colleagues had thought she looked pale. The patient had been found to be anaemic with a haemoglobin concentration of 4.7 g/dL and a peripheral blood smear suggestive of a hypochromic microcytic anaemia. She had no other medical history. She was transfused 2 units of blood; she was investigated at the outpatient clinic but was not referred for endoscopic assessment.
Investigations showed a haemoglobin concentration of 8.1 g/dL, platelet count of 565X109 per L (normal 150-400), and white cell count of 10.5X109 per L; the mean corpuscular volume was 77.2 fL (normal 80-94) and the mean corpuscular haemoglobin was 23.1 pg per cell-suggestive of iron deficiency anaemia. The patient’s renal and liver function tests were unremarkable.
Investigations showed a haemoglobin concentration of 8.1 g/dL, platelet count of 565X109 per L (normal 150-400), and white cell count of 10.5X109 per L; the mean corpuscular volume was 77.2 fL (normal 8-94) and the mean corpuscular haemoglobin was 23.1 pg per cell-suggestive of iron deficiency anaemia. The patient’s renal and liver function tests were unremarkable.
We carried out an exploratory laparotomy and found a duodenojejunal intussusception. We were unable to manually reduce the lesion, and so carried out a segmental resection of third part of the duodenum and proximal jejunum with a side-to-side duodenojejunal anastomosis at the second part of the duodenum. Analysis of the excised lesion showed a 6 cmX5 cm well-encapsulated and pedunculated tumour of the third part of the duodenum which acted as the intussusceptum telescoping into the proximal jejunum-the intussuscipiens (appendix). Histological analysis of samples of the tumour showed a poorly differentiated extra-skeletal Ewing sarcoma of the duodenum. Immunohistochemistry stains demonstrated strong and diffuse nuclear immunoreactivity to NKX2-2 and ERG, with membranous immunoreactivity to CD99, and an absence of nuclear immunoreactivity to FLI1: supporting a possible fusion of the EWSRI gene on chromosome 22q12 with the gene encoding the transcription factor ERG (appendix). The tumour cells exhibited no immunoreactivity to cytokeratin AE1/AE3, CD20, CD3, LCA, TdT, synaptophysin, chromogranin, desmin, myogenin, S100, and α-smooth muscle actin.
Postoperatively, the patient recovered well and was discharged after a week. One month later, she returned reporting persistent abdominal and lower back pain. An abdominal CT showed enlarged coeliac, para-caval, and para-aortic lymph nodes with no lung metastases in the lower half of the thorax. Skeletal x-rays of the axial and cortical bones displayed no osteolytic bone lesions. The patient was urgently transferred to the oncology clinic but died before treatment was commenced.
Extraskeletal Ewing sarcoma of the small intestine is an extremely rare tumour with poor prognosis. However, if detected early, it may be successfully treated with surgical resection and adjuvant chemotherapy. Young adults presenting with recurrent vomiting, weight loss, an abdominal mass, and anaemia should raise the suspicion of an aggressive malignancy
(16). King B, et al. Two Phase 3 Trials of Baricitinib for Alopecia Areata. N Engl J Med. 2022
Background
Alopecia areata is an autoimmune condition characterized by rapid hair loss in the scalp, eyebrows, and eyelashes, for which treatments are limited. Baricitinib, an oral, selective, reversible inhibitor of Janus kinases 1 and 2, may interrupt cytokine signaling implicated in the pathogenesis of alopecia areata.
Methods
We conducted two randomized, placebo-controlled, phase 3 trials (BRAVE-AA1 and BRAVE-AA2) involving adults with severe alopecia areata with a Severity of Alopecia Tool (SALT) score of 50 or higher (range, 0 [no scalp hair loss] to 100 [complete scalp hair loss]). Patients were randomly assigned in a 3:2:2 ratio to receive once-daily baricitinib at a dose of 4 mg, baricitinib at a dose of 2 mg, or placebo. The primary outcome was a SALT score of 20 or less at week 36.
Results
We enrolled 654 patients in the BRAVE-AA1 trial and 546 in the BRAVE-AA2 trial. The estimated percentage of patients with a SALT score of 20 or less at week 36 was 38.8% with 4-mg baricitinib, 22.8% with 2-mg baricitinib, and 6.2% with placebo in BRAVE-AA1 and 35.9%, 19.4%, and 3.3%, respectively, in BRAVE-AA2. In BRAVE-AA1, the difference between 4-mg baricitinib and placebo was 32.6 percentage points (95% confidence interval [CI], 25.6 to 39.5), and the difference between 2-mg baricitinib and placebo was 16.6 percentage points (95% CI, 9.5 to 23.8) (P<0.001 for each dose vs. placebo). In BRAVE-AA2, the corresponding values were 32.6 percentage points (95% CI, 25.6 to 39.6) and 16.1 percentage points (95% CI, 9.1 to 23.2) (P<0.001 for each dose vs. placebo). Secondary outcomes for baricitinib at a dose of 4 mg but not at a dose of 2 mg generally favored baricitinib over placebo. Acne, elevated levels of creatine kinase, and increased levels of low- and high-density lipoprotein cholesterol were more common with baricitinib than with placebo.
Conclusions
In two phase 3 trials involving patients with severe alopecia areata, oral baricitinib was superior to placebo with respect to hair regrowth at 36 weeks. Longer trials are required to assess the efficacy and safety of baricitinib for alopecia areata
Longer trials are required to assess the efficacy and safety of baricitinib for alopecia areata
Background: The risks for anaphylaxis among intravenous (IV) iron products currently in use have not been assessed.
Objective: To compare risks for anaphylaxis among 5 IV iron products that are used frequently.
Design: Retrospective cohort study using a target trial emulation framework.
Setting: Medicare fee-for-service data with Part D coverage between July 2013 and December 2018.
Participants: Older adults receiving their first administration of IV iron.
Measurements: The primary outcome was the occurrence of anaphylaxis within 1 day of IV iron administration, ascertained using a validated case definition. Analysis was adjusted for 40 baseline covariates using inverse probability of treatment weighting. The adjusted incidence rates (IRs) for anaphylaxis per 10 000 first administrations and odds ratios (ORs) were computed.
Results: The adjusted IRs for anaphylaxis per 10 000 first administrations were 9.8 cases (95% CI, 6.2 to 15.3 cases) for iron dextran, 4.0 cases (CI, 2.5 to 6.6 cases) for ferumoxytol, 1.5 cases (CI, 0.3 to 6.6 cases) for ferric gluconate, 1.2 cases (CI, 0.6 to 2.5 cases) for iron sucrose, and 0.8 cases (CI, 0.3 to 2.6 cases) for ferric carboxymaltose. Using iron sucrose as the referent category, the adjusted ORs for anaphylaxis were 8.3 (CI, 3.5 to 19.8) for iron dextran and 3.4 (CI, 1.4 to 8.3) for ferumoxytol. When cohort entry was restricted to the period after withdrawal of high-molecular-weight iron dextran from the U.S. market in 2014, the risk for anaphylaxis associated with low-molecular-weight iron dextran (OR, 8.4 [CI, 2.8 to 24.7]) did not change appreciably. Anaphylactic reactions requiring hospitalizations were observed only among patients using iron dextran or ferumoxytol.
Conclusion: The rates of anaphylaxis were very low with all IV iron products but were 3- to 8-fold greater for iron dextran and ferumoxytol than for iron sucrose.
(18). Wensink MJ. Preconception Antidiabetic Drugs in Men and Birth Defects in Offspring, a Nationwide Cohort Study. Ann Intern Med. 2022.
Background: Diabetes reduces semen quality and increasingly occurs during reproductive years. Diabetes medications, such as metformin, have glucose-independent effects on the male reproductive system. Associations with birth defects in offspring are unknown.
Objective: To evaluate whether the risk for birth defects in offspring varies with preconceptional pharmacologic treatment of fathers with diabetes.
Design: Nationwide prospective registry-based cohort study.
Setting: Denmark from 1997 to 2016.
Participants: All liveborn singletons from mothers without histories of diabetes or essential hypertension.
Measurements: Offspring were considered exposed if their father filled 1 or more prescriptions for a diabetes drug during the development of fertilizing sperm. Sex and frequencies of major birth defects were compared across drugs, times of exposure, and siblings.
Results: Of 1 116 779 offspring included, 3.3% had 1 or more major birth defects (reference). Insulin-exposed offspring (n = 5298) had the reference birth defect frequency (adjusted odds ratio [aOR], 0.98 [95% CI, 0.85 to 1.14]). Metformin-exposed offspring (n = 1451) had an elevated birth defect frequency (aOR, 1.40 [CI, 1.08 to 1.82]). For sulfonylurea-exposed offspring (n = 647), the aOR was 1.34 (CI, 0.94 to 1.92). Offspring whose fathers filled a metformin prescription in the year before (n = 1751) or after (n = 2484) sperm development had reference birth defect frequencies (aORs, 0.88 [CI, 0.59 to 1.31] and 0.92 [CI, 0.68 to 1.26], respectively), as did unexposed siblings of exposed offspring (3.2%; exposed vs. unexposed OR, 1.54 [CI, 0.94 to 2.53]). Among metformin-exposed offspring, genital birth defects, all in boys, were more common (aOR, 3.39 [CI, 1.82 to 6.30]), while the proportion of male offspring was lower (49.4% vs. 51.4%, P = 0.073).
Limitation: Information on underlying disease status was limited.
Conclusion: Preconception paternal metformin treatment is associated with major birth defects, particularly genital birth defects in boys. Further research should replicate these findings and clarify the causation.
(19). Buck Louis GM, et al. Paternal Preconception Diabetes Drugs and Birth Defects in Offspring: A Call for More Conclusive Study.2022.
Birth defects remain the leading cause of infant mortality in many geographic regions, including the United States where they account for approximately 20% of deaths. Given that most birth defects have a relatively low incidence, they can be exceedingly difficult to study and often require investigation at the population level and over time to ensure sufficiently powered epidemiologic investigations. These methodological challenges can delay the identification of emerging teratogens, especially in the context of rapid changes in the health status of reproductive-aged populations, such as the growing percentage of young adults who are overweight or obese.What is the problem and what is known about it so far?
Poorly controlled diabetes can reduce sperm quality. However, the effects of diabetes medications on sperm quality are uncertain. Information is lacking about the risk for birth defects in babies born to fathers with diabetes. If birth defects were more common with some diabetes medications, birth outcomes could potentially be improved if men with diabetes switched to other diabetes medications when trying to father a child.
Why did the researchers do this particular study?
Why did the researchers do this particular study?
Who was studied?
The researchers studied 1 116 779 babies born in Denmark from 1996 to 2017 to mothers who did not have diabetes or high blood pressure.
How was the study done?
The researchers used health databases in Denmark. Babies were considered exposed to a diabetes drug if their father filled at least 1 prescription during the 3 months when the fertilizing sperm were developing. The researchers then compared birth defects in the babies across diabetes drugs and the timing of taking the drug relative to development of fertilizing sperm in unexposed siblings of the babies. The study only looked at 3 types of diabetes drugs: insulin, metformin, and sulfonylureas.
What did the researchers find?
Of the 1 116 779 babies studied, 3.3% had a major birth defect overall. Babies whose fathers took insulin had no increased risk for a birth defect compared with the general group. Babies whose fathers took metformin had an increased risk for birth defects. There were too few babies whose fathers took sulfonylureas to determine risks for birth defects with any certainty. The researchers did not find an increased risk for birth defects in babies whose fathers took metformin before or after but not during the period of sperm development. Siblings who were not exposed to metformin did not have increased risk for birth defects.
What were the limitations of the study?
There are newer drug classes used to treat type 2 diabetes that were not studied. The study did not account for how well a father’s diabetes was controlled during sperm development. The researchers were unable to determine whether fathers taking insulin had type 1 or type 2 diabetes. Metformin and sulfonylureas are only used to treat type 2 diabetes, so it is reasonable to assume that the fathers receiving these drugs had type 2 diabetes.
What are the implications of the study?
Metformin taken during the period of sperm development seems to increase the risk for birth defects in babies fathered during this time. Further studies are needed to confirm and better understand this association. However, men with diabetes who are taking metformin should talk to their doctors about whether they should switch to another treatment when trying to conceive a child. Because diabetes control also affects sperm quality, discontinuing metformin treatment could also affect birth outcomes.
(20). Bergamaschi L, et al. Malignant Anterior ST-Segment Elevation. JAMA Intern Med. 2022.
Case Presentation
A patient in the 70s was admitted to the emergency department for chest pain. The patient’s medical history included hypertension and previous high-grade bladder urothelial carcinoma that was treated with radical cystectomy (regular urological follow-up). The patient’s cardiological history was negative, and electrocardiogram (ECG) reports were normal. The admission 12-lead ECG is shown in the Figure.
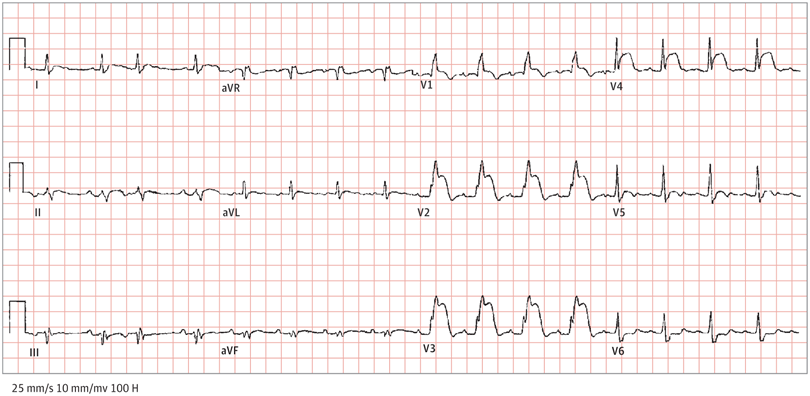
Admission 12-lead ECG recorded in the emergency department showed sinus rhythm (95 beats per minute) with atrial premature complexes. There was a typical right bundle branch block (QRS, 126 milliseconds) with concordant convex ST-segment elevation in the anterior leads (V1, V2, V3, and V4) without reciprocal ST-segment depression in the inferior leads.
Because the 12-lead ECG indicated marked anterior ST-segment elevation (STE), the patient was immediately transferred to the catheterization laboratory to undergo emergency coronary angiography, the results of which showed nonobstructive coronary arteries. Troponin I levels (0-3 hours) were 0.285 to 0.374 ng/mL (normal range, <0.04 ng/mL; to convert to μg/L, multiply by 1), and the brain natriuretic peptide levels were 1734 pg/mL (normal range, <100 pg/mL). Therefore, the patient was admitted to the cardiology department for subsequent treatment. Serial ECGs that were performed during the 2-week hospital stay showed persistent STE changes.
Questions: Regarding the ECG report, what are the most likely mechanisms for STE, and how would you treat this patient?
Interpretation and Clinical Course
The ECG (Figure) shows sinus rhythm (95 beats per minute) with atrial premature complexes, right bundle branch block (QRS width, 126 milliseconds) and a convex STE in the anterior leads (V1, V2, V3, and V4) without reciprocal ST-segment depression in the inferior leads. To rule out an obstructive coronary artery disease, the patient underwent urgent coronary angiography, which showed no coronary stenosis; therefore, it fulfilled the diagnostic criteria for acute myocardial infarction with nonobstructive coronary arteries (MINOCA).1
In this case, in addition to an echocardiogram, cardiac magnetic resonance imaging (MRI) was performed and showed an invasive mass with areas of central necrosis located at the apex of the right ventricle infiltrating the pericardium and the apical interventricular septum (IVS). The mass appeared markedly hyperintense in the T2 sequences and exhibited late gadolinium enhancement, all features consistent with malignant tumors.
Regarding the subsequent clinical course, a transcatheter biopsy was performed and confirmed the diagnosis of high-grade urothelial carcinoma metastasis. Given the high surgical risk, the patient received palliative chemotherapy but unfortunately died 6 months later.
Discussion
The present case is a unique example of STE-MINOCA due to an invasive malignant cardiac mass in the right ventricle. As known, the working diagnosis of MINOCA may underlie a wide spectrum of etiologies, including cardiac and extracardiac conditions. In this setting, it is recommended to follow a specific diagnostic algorithm, and cardia MRI plays a pivotal role. The ability of cardiac MRI and other diagnostic methods, such as intracoronary imaging, to reveal the exact mechanisms of damage has important implications on clinical management.
Another interesting aspect of this clinical case is that cardiac masses are a diagnostic challenge, especially the correct discrimination between benign, malignant, or pseudo tumors with markedly different clinical management and prognosis. To evaluate a cardiac mass, the medical history is pivotal; however, a first-level examination, such as 12-lead ECG, could be useful (eg, when marked alterations are present without a clear etiological cause, such as coronary obstruction or myopericarditis). The first-level imaging examination remains the transthoracic echocardiogram given its high availability and noninvasiveness. However, a multimodal second-level imaging approach may add valuable information, including cardiac MRI or cardiac computed tomography, as would functional imaging techniques, such as positron emission tomography. Finally, an invasive biopsy could be fundamental in understanding the nature of the cardiac mass.
In this case, as shown in the Figure, all the ECG abnormalities could be associated with the effect of the cardiac tumor. Because the mass infiltrated the IVS, it is possible that there was an involvement of the right bundle branch that resulted in a complete bundle block. The STE is a consequence of the mass that transmurally invaded the apical IVS, perfectly mimicking an anterior STE myocardial infarction (STEMI) with a transmural wavefront lesion. In fact, in this case, the ST-segment alteration was present only in the leads (V1, V2, V3, and V4) that directly explore the territories where the cardiac mass infiltrates the myocardium, whereas the ST segment dropped to the isoelectric line toward the anterolateral leads as the left ventricular free wall is spared. Finally, possible explanations for the absence of ST-segment depression in the reciprocal leads, which is a marker of the ischemic transmural lesion, are interesting and generate several speculations. First, in this case, the absence of a true ischemic process that determines existing distant ischemia did not generate the displacement of the injury current vector away from the noninfarcted myocardium.8 Second, the specific area of the cardiac mass infiltration was more limited and constant over time as opposed to a classic myocardial ischemia wave front, which is a large and dynamic electric process.
Numerous other medical conditions have been known to mimic STEMI-like ECG changes, and there have been some case reports of cardiac tumors that presented with ST abnormalities. However, the feature to solving this ECG presentation was the absence of reciprocal ECG changes, which is a pivotal electrocardiographic phenomenon that needs to be researched carefully. The presence of reciprocal change increases the positive predictive value for a diagnosis of acute myocardial infarction to more than 90%.
Take-home Points
Several medical conditions, other than acute coronary obstruction, could exhibit STE on a 12-lead ECG. The presence of reciprocal ECG changes is a crucial sign of ischemia, whereas the absence of reciprocal ST depression should lead to the consideration of a non-ischemia-related diagnosis.
The STE associated with cardiac mass is infrequent and was reported only in some clinical cases. Metastatic tumors of the heart are more frequently observed than primary tumors.
The MINOCA and cardiac tumors are clinically challenging, and a comprehensive diagnostic algorithm is essential to diagnose and understand the underlying mechanism.
