Research Article
Early diagnosis of Pulmonary Artery Hypertension in CCU patients, using Echocardiography, helps towards a better clinical outcome
Yogeshwaran Sakthivel1,*, S. Aravinda Kumar2
1Masters in Emergency Medicine – Post Graduate Resident, Kauvery Heart City, Kauvery Hospital, Trichy, India
2Senior Consultant Cardiologist, HeartCity, Kauvery Hospital, Trichy, India.
*Correspondence: dryogeshmbbs@gmail.com
Abstract
Pulmonary Arterial Hypertension (PAH) is a chronic and progressive disease affecting pulmonary arteries which results from increased pulmonary arterial pressures and consequent pulmonary vascular resistance. As the disease progresses, the increased pressure in pulmonary arteries results in Right Ventricular Failure (RVF), which is a common cause of increased mortality in cardiac patients from heart failure. RVF is clinically defined as reduced cardiac output and increased right ventricular filling pressure. Patients with PAH are at risk of developing pulmonary embolism and cardiac arrhythmias. Critically ill patients with PAH remain at high risk of adverse outcomes, requiring a diligent and thoughtful approach to diagnosis and treatment. Our objective was to evaluate the outcomes of patients with PAH admitted to the Critical Care Unit (CCU) using Echocardiography (Echo), and this early diagnosis, and appropriate and efficient therapeutic actions in time, may prevent the patients from developing cardiac dysfunction. From the study, we report that the patients who have high PAH have a longer length of stay in CCU.
Keywords: Pulmonary Hypertension, Echocardiography, Average Length of Stay, CCU, Heart Failure
Background
Pulmonary Arterial Hypertension (PAH) is a progressive disorder characterized by high blood pressure (hypertension) in the arteries of the lungs (pulmonary artery) for no apparent reason. The pulmonary arteries are the blood vessels that carry blood from the right side of the heart through the lungs. Patients with PAH are admitted to the critical care unit (CCU) for a variety of reasons. Symptoms of PAH include shortness of breath (dyspnoea), especially during exercise, chest pain, and fainting episodes. Pulmonary Hypertension (PH) is a general term for high blood pressure that occurs only in the arteries in the lungs and may affect the right side of the heart. The term PAH refers to a specific cause of pulmonary hypertension but there are other causes of pulmonary hypertension as mentioned in Table 1.
Table 1. Causes of Pulmonary Hypertension
Cardiac Diseases | Congenital heart diseases: for example, Atrial Septal Defect, Persistent Ductus Arteriosus |
| Left-sided heart diseases: Mitral valve disease, left ventricular dysfunction |
Respiratory Diseases | Obstructive lung diseases: Asthma, Bronchiectasis |
| Parenchymal lung diseases: Idiopathic pulmonary fibrosis |
| Thoracic abnormalities: Kyphoscoliosis |
Thromboembolic diseases | Amniotic fluid embolism |
| Pulmonary veno-occlusive disease |
Collagen vascular diseases | Primary pulmonary hypertension includes drug-related, and from infections like the human immunodeficiency virus |
Chronic damage and destruction of pulmonary vasculature increase Pulmonary Vascular Resistance (PVR) and pulmonary arterial pressures which lead to Right Ventricular Failure (RVF). The right ventricle responds to increased pulmonary pressures with compensatory structural changes that compromise the ability of the heart to maintain sufficient cardiac output. Understanding the physiology of pulmonary hypertension and the underlying defects on the right side of the heart is required to treat this complex and life-threatening disorder that can develop in patients in the CCU.
Physiology of Pulmonary Hypertension
The normal structure and function of the right ventricle reflect the low resistance and high compliance and capacitance of the pulmonary vasculature system to which it delivers blood. The thin-walled structure of the right ventricle implies the low resistance of the pulmonary vasculature. Functionally, the right ventricle spends little time in isovolumic contraction or relaxation and as a result, can generate cardiac output with only a fifth of the energy demanded by the left ventricle (LV). The right ventricle receives a continuous flow of coronary blood via the Right Coronary Artery (RCA) during both systole and diastole. This blood supply sustains the thin-walled structure of the RV as well as its relatively small isovolumic activity. Given this physiology, adapted specifically for the low resistance pulmonary vasculature, the right ventricle has difficulty responding to the increased resistance of pulmonary hypertension. The adaptive changes that the RV undergoes cause structural changes that compromise its ability to maintain cardiac output (Fig. 1).
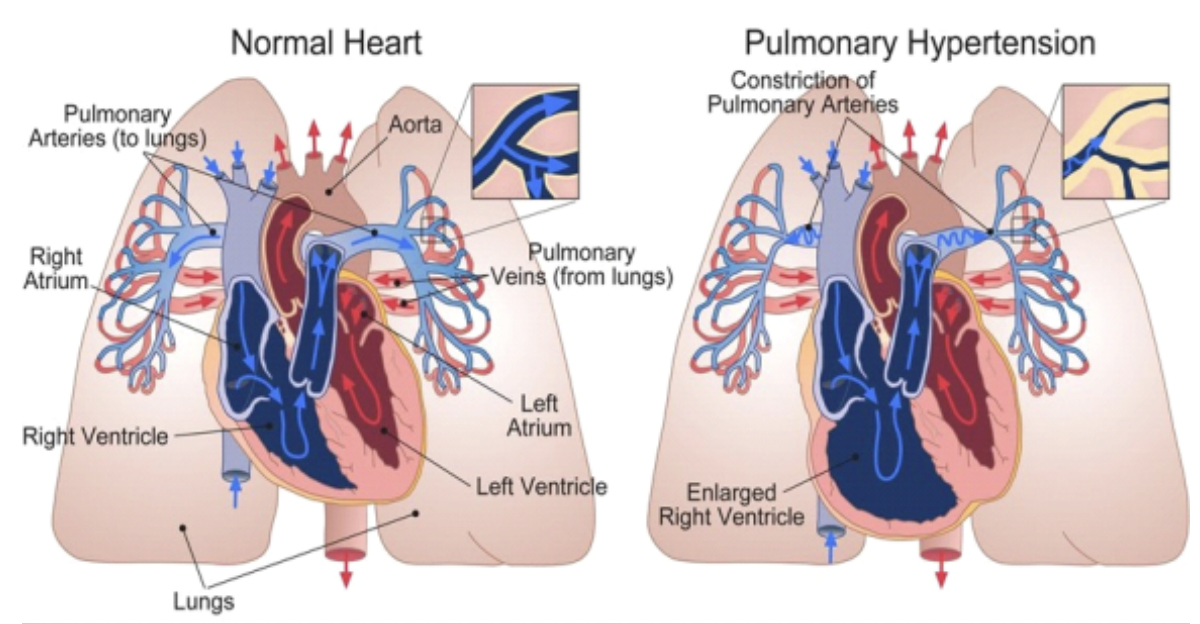
Fig. 1. Shows the physiology of Pulmonary Hypertension.
To reduce the wall tension caused by the increased afterload of PAH, hypertrophy of the right ventricle occurs. As a result, coronary flow no longer occurs in diastole despite the increased demand of the hypertrophied right ventricle. Also, the right ventricle spends more time in isovolumic contraction and relaxation to overcome increased pulmonary pressures, which results in a reduction of right heart output and greater energy demand. RV hypertrophy also interferes with the normal motion of the tricuspid valve and together with increased pulmonary pressures results in tricuspid regurgitation. The hypertrophy of the right ventricle also impedes the function of the LV as the interventricular septum bulges into the LV. These changes in the right ventricle all contribute to the reduction of cardiac output, which in turn decreases coronary flow to the RV and causes ischemic damage. Finally, this hypertrophy of the right ventricle accompanied by ischemic damage eventually leads to ventricular dilatation and right heart failure (Fig. 2).
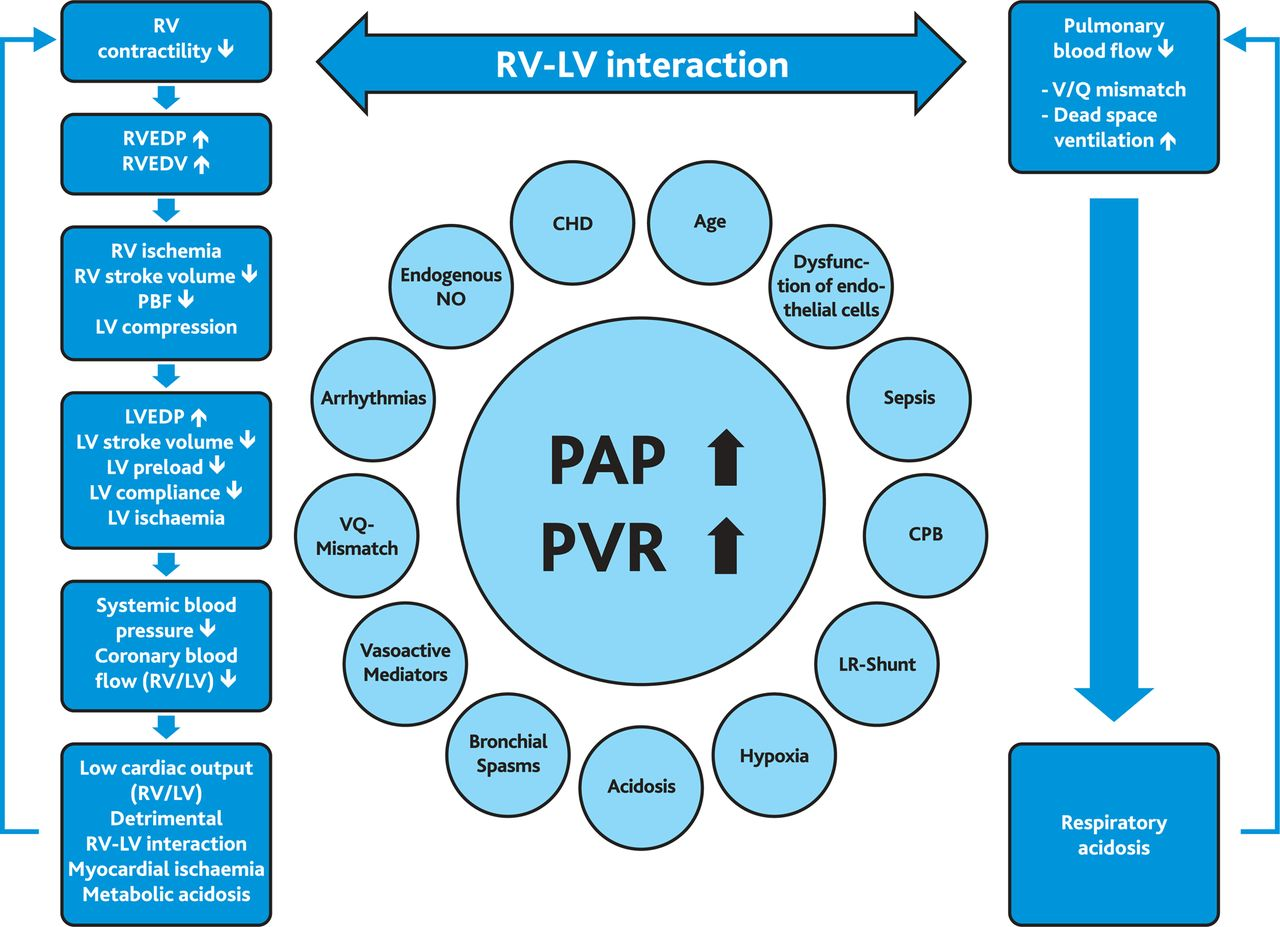
Fig. 2. Schematic diagram of PAH crisis and contributing factors. A pulmonary hypertensive crisis develops with an acute increase of PAP. This leads to an increase in RV pressure and volume causing a shift of the interventricular septum towards the left side and reducing LV volume. Filling pressures of ventricles rise, compensatory tachycardia and the drop in systemic blood pressure compromise coronary perfusion pressure and flow, leading to low cardiac output and metabolic acidosis. Furthermore, the increase in PAP causes decreased pulmonary blood flow and airway obstruction related to arterial distension of the smaller intrapulmonary arteries and lung oedema. Consequently, dead space ventilation increases; together with a mismatch of pulmonary ventilation and perfusion, this causes hypoxia and respiratory acidosis. PAH, pulmonary arterial hypertension; RVEDV, RV end-diastolic volume; RVEDP, RV end-diastolic pressure; LVEDP, LV end-diastolic pressure; V/Q, pulmonary ventilation, and perfusion; PAH, pulmonary arterial hypertension; PAP, pulmonary artery pressure; PVR, pulmonary vascular resistance; CHD, congenital heart disease; NO, nitric oxide; CPB, cardiopulmonary bypass; LR-Shunt, left-to-right shunt; PBF, pulmonary blood flow.
As the heart remodels in response to PAH, patients become susceptible to atrial arrhythmias. The remodelling process predisposes patients with PAH to arrhythmias by modulating autonomic activity and delaying cardiac repolarization. Also, ischemic myocardial damage to the RV itself can predispose patients to develop an arrhythmia. Atrial arrhythmias are challenging to manage in the CCU given the potential negative inotropic effects of beta-blockers and high doses of calcium channel blockers on the right heart.
Materials and Methods
We have performed a prospective study in the CCU of Heart-City KMC Hospital at Trichy. The study was to evaluate the outcomes of the patient in CCU with pulmonary hypertension. The number to be evaluated was determined as 100 patients in CCU, whose PAH was estimated by using echocardiography in each patient. The objective of this study was to compare the PAH with the average length of stay (ALOS) in the CCU. The hypothesis to be investigated was that the patients who have high PAH have a longer length of stay in the CCU.
Results and Discussion
Pulmonary Hypertension leading to decompensation of the cardiovascular system can be considered a syndrome with non-specific signs and symptoms presenting late in the disease process and may be strongly associated with, or directly caused by, several and very heterogeneous underlying conditions.
Evaluation of Pulmonary Hypertension patients in CCU
Most symptoms and signs of PH are non-specific, which causes a delay in diagnosis and initiation of treatment, especially in idiopathic PAH. The symptoms may include dyspnea (especially on exertion), chest pain, cough, palpitations, fatigue, orthopnea, paroxysmal nocturnal dyspnea, syncope, near-syncope, and peripheral edema. Abdominal pain, distension, and early satiety may also occur due to RV failure, from hepatic congestion. Moreover, hoarseness of voice may occur with compression of the left recurrent laryngeal nerve due to a dilated pulmonary artery (Ortner’s syndrome). Hemoptysis rarely occurs, but if present, it is usually associated with PAH or concomitant pulmonary embolism, pulmonary infarction, or severe mitral stenosis.
Physical examination generally reveals signs of decompensated RV failure, including jugular vein distention, hepatomegaly, ascites, and peripheral pitting edema. Other signs may include a left parasternal lift, accentuated P2 sound, pansystolic murmur due to tricuspid regurgitation, diastolic murmur due to pulmonary insufficiency, S3 and S4 gallops, cooling of extremities, and diminished pulse pressure. Some signs may suggest a specific cause of PH; for example, the presence of venous stasis ulcers may suggest sickle cell disease.
Echocardiography is a diagnostic tool for Pulmonary Hypertension
Transthoracic echocardiography (TTE) with the use of Doppler ultrasound is the most available and widely used tool for diagnosing and monitoring patients with PH. Although it may not be an accurate tool, especially in critically ill patients, it provides valuable information for clinicians. It can effectively identify congenital heart diseases, such as intracardiac shunts or left heart disease as the underlying cause of PH. Moreover, it can estimate the right atrial pressure (RAP), mPAP, and level of RV dysfunction and help determine the underlying cause of PH non-invasively.
To estimate mPAP, TTE uses functional tricuspid regurgitation (TR), which occurs because of disturbance in the geometrical structure of RV in PH; therefore, this measurement is prone to over-or underestimation. Furthermore, an increase or decrease in mPAP is not necessarily correlated with the clinical status or prognosis of patients. Signs indicating a dysfunctional RV include RV and RA hypertrophies, dyskinesia of the right free wall of RV (McConnell’s sign), and straightening or leftward bowing of the interventricular septum (D-shaped LV), paradoxical movement of the septum in the systole, and a dilated inferior vena cava).
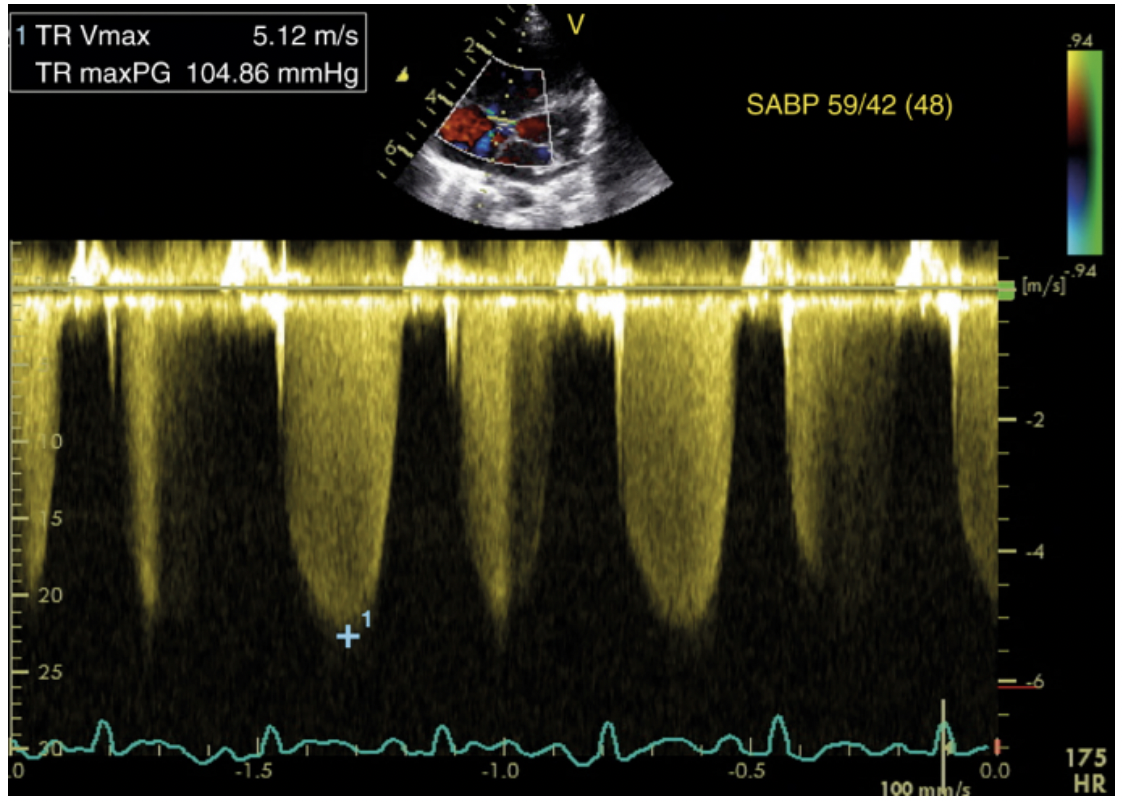
Fig. 3. Calculation of Pulmonary Arterial Pressure (PAP) by Echocardiography.
Evaluation of the RV’s size and function may be challenging due to its crescent shape and thin walls. Several parameters have been used to assess the RV function, which seems to be well correlated with the disease prognosis, including estimated RAP, RV longitudinal strain, tricuspid annular plane systolic excursion, right ventricular Tei index (myocardial performance index), RV fractional area change, and RV strain based on speckle tracking. Other parameters that can be used at the bedside to evaluate the RV function may include the RV/LV area ratio, LV eccentricity index, peak velocity of systolic excursion, and RV systolic pressure.
Three-dimensional (3D) echocardiography is emerging as a useful tool for the assessment of RV. It can accurately estimate the RV size and ejection fraction (EF) and improve the assessment of RV function non-invasively. The findings of 3D echocardiography are well correlated with cardiac MRI, and therefore, it is reasonable to use it as a non-invasive and accurate tool for the evaluation of RV function in combination with 2D echocardiography.
Statistical Analysis
Statistical analysis was performed using SPSS (version 23.0). The continuous variable will be expressed as mean and standard deviation. Categorical variables will be expressed as frequency and percentage. An Independent T-test will be used to find the significant difference between groups. Correlations relationship between two variables analysed by applying Pearson’s Co-efficient. The Chi-square test and fisher’s exact test will be used to find out the association between the categorical variables. P <0.05 will be considered statistically significant.
In this study, we have performed echocardiography for 100 patients who were admitted in CCU, to rule out pulmonary hypertension. The collected data on pulmonary artery pressure in each patient was classified into Normal (<35 mmHg), Mild (36-45 mmHg), Moderate (46-60 mmHg), and Severe (>60 mmHg).
Table 2. Calculation of ALOS × Pulmonary Artery Pressure
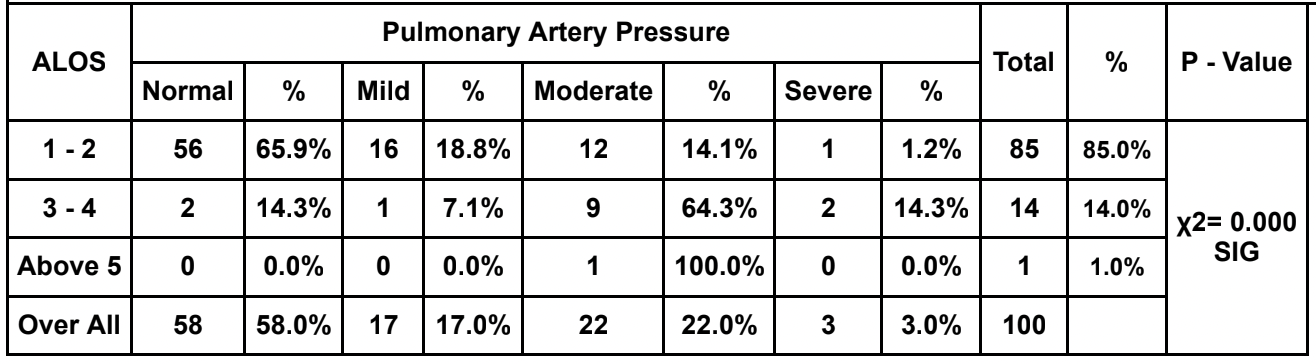
The above table shows the correlation of pulmonary artery pressure with the average length of stay (ALOS) in CCU for each patient.
Explanation of Data Analysis
- Among 100, 58 patients with normal pulmonary artery pressure, 56 patients had a maximum of 2 days of the length of stay and 2 patients had less than 4 days of length of stay in CCU.
- Among 100, 17 patients with Mild Pulmonary artery hypertension,16 patients had 2 days of the length of stay and 1 patient had 3 days of the length of stay in CCU.
- Among 100, 22 patients with Moderate Pulmonary artery hypertension,12 patients had 2 days of the length of stay and 9 patients had 4 days of the length of stay in CCU and 1 patient had stayed more than 5 days of the length of stay in CCU.
- Among 100, 3 patients with severe pulmonary artery hypertension, 1 patient had 2 days of the length of stay and 2 patients had more than 4 days of the length of stay in CCU.
Thus, the increase in the pulmonary artery pressure i.e., the PAH patients had a prolonged length of stay in the Critical Care Unit – CCU which denotes the poor outcome of patients with Pulmonary Arterial Hypertension in CCU.
Conclusion
Pulmonary Hypertension is a serious complication in the patient in CCU at risk, including those after surgery for CHD, and has a major impact on clinical outcomes in patients with and without chronic PAH. Treatment in the CCU should be based on the underlying pathophysiology but ultimately needs to focus on the basic goals of lowering RV afterload and augmenting RV preload and contractility. Furthermore, maintaining adequate coronary perfusion pressure and flow will help to preserve myocardial oxygen and energy supply, and thus RV and LV systolic function and oxygen delivery. Therefore, this study shows that patients with pulmonary artery hypertension have prolonged lengths of stay in the Critical Care Unit. Thus, the early diagnosis using Echocardiography of patients at particular risk, and timely establishment of efficient therapeutic actions may prevent the development of severe cardiac dysfunction, low cardiac output, and death.
Acknowledgement
The authors Drs. SY and SAK acknowledge the nursing staff at the CCU – Heart City, Trichy, and submit their heartfelt thanks to the patients involved in this study. We submit heartful thanks to Mr. Dhasaratharaman for statistical analysis support.
References
- Merlos P, Níºí±ez J, Sanchis J, et al. Echocardiographic estimation of pulmonary arterial systolic pressure in acute heart failure. Prognostic implications. Eur J Intern Med. 2013; 24(6):562-7.
- Huynh TN, Weigt SS, Sugar CA, et al. Prognostic factors and outcomes of patients with pulmonary hypertension admitted to the intensive care unit. J Crit Care. 2012;27(6):739.e7-13.
- Nowroozpoor A, Malekmohammad M, Seyyedi SR, et al. Pulmonary Hypertension in intensive care units: an updated review. Tanaffos. 2019;18(3):180-207.
- Broder N, Zolty R. Pulmonary arterial hypertension in the ICU. In: Oropello JM, Pastores SM, Kvetan V. eds. Critical Care. McGraw Hill; . Accessed March 14, 2022. https://accessmedicine.mhmedical.com/content.aspx?bookid=1944§ionid=14351731
- Kaestner M, Schranz D, Warnecke G, et al. Pulmonary hypertension in the intensive care unit. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPKHeart 2016;102:ii57-ii66.
- Kosaraju A, Goyal A, Grigorova Y, et al. Left Ventricular ejection fraction. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459131/HHS Vulnerability Disclosure.

Dr. S. Yogeshwaran
Emergency Medicine – Post Graduate Resident

Dr. S. Aravindakumar
Chief Consultant Interventional Cardiologist
