Journal scan
A review of 10 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Pravesh S, et al. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. BMJ 2022;376:e065846
Abstract
Objective: To assess whether percutaneous transforaminal endoscopic discectomy (PTED) is non-inferior to conventional open microdiscectomy in reduction of leg pain caused by lumbar disc herniation.
Design: Multicentre randomised controlled trial with non-inferiority design.
Setting: Four hospitals in the Netherlands.
Participants: 613 patients aged 18-70 years with at least six weeks of radiating leg pain caused by lumbar disc herniation. The trial included a predetermined set of 125 patients receiving PTED who were the learning curve cases performed by surgeons who did not do PTED before the trial.
Interventions: PTED (n=179) compared with open microdiscectomy (n=309).
Main outcome measures: The primary outcome was self-reported leg pain measured by a 0-100 visual analogue scale at 12 months, assuming a non-inferiority margin of 5.0. Secondary outcomes included complications, reoperations, self-reported functional status as measured with the Oswestry Disability Index, visual analogue scale for back pain, health related quality of life, and self-perceived recovery. Outcomes were measured until one year after surgery and were longitudinally analysed according to the intention-to-treat principle. Patients belonging to the PTED learning curve were omitted from the primary analyses.
Results: At 12 months, patients who were randomised to PTED had a statistically significantly lower visual analogue scale score for leg pain (median 7.0, interquartile range 1.0-30.0) compared with patients randomised to open microdiscectomy (16.0, 2.0-53.5) (between group difference of 7.1, 95% confidence interval 2.8 to 11.3). Blood loss was less, length of hospital admission was shorter, and timing of postoperative mobilisation was earlier in the PTED group than in the open microdiscectomy group. Secondary patient reported outcomes such as the Oswestry Disability Index, visual analogue scale for back pain, health related quality of life, and self-perceived recovery, were similarly in favour of PTED. Within one year, nine (5%) in the PTED group compared with 14 (6%) in the open microdiscectomy group had repeated surgery. Per protocol analysis and sensitivity analyses including the patients of the learning curve resulted in similar outcomes to the primary analysis.
Conclusions: PTED was non-inferior to open microdiscectomy in reduction of leg pain. PTED resulted in more favourable results for self-reported leg pain, back pain, functional status, quality of life, and recovery. These differences, however, were small and may not reach clinical relevance. PTED can be considered as an effective alternative to open microdiscectomy in treating sciatica.
(2). Pashankar R. A woman pregnant with twins has fever, haemolysis, and thrombocytopenia caused by babesiosis: could be confused with HELLP syndrome. Lancet 2022;399(10327).
A 44-year-old woman-35 weeks pregnant with dichorionic, diamniotic twins-was admitted to our hospital with 7-day history of fever, weakness, and shortness of breath.
Notably in the week before, the patient had been seen twice by her obstetrician and found to have normal or low blood pressure along with a fever. She had no other unusual medical history. On examination, the patient was pale and breathless; her temperature was 38.8°C, blood pressure was 110/60 mm Hg, and she had petechiae scattered about her body with oedema of both legs
Laboratory investigations showed a haematocrit of 31.3% (normal >35), an elevated aspartate aminotransferase (AST) concentration of 110 units per L (normal <40), alanine aminotransferase (ALT) was normal, total bilirubin concentration of 1.7 mg/dL (normal <1.2), a platelet count of 17 x 109 (normal >150), and a 3+ proteinuria. A transvaginal ultrasound scan showed vertex twins and a marginal placenta praevia. A peripheral blood smear showed intraerythrocytic parasites-Babesia microti-with a 19.3% parasitaemia
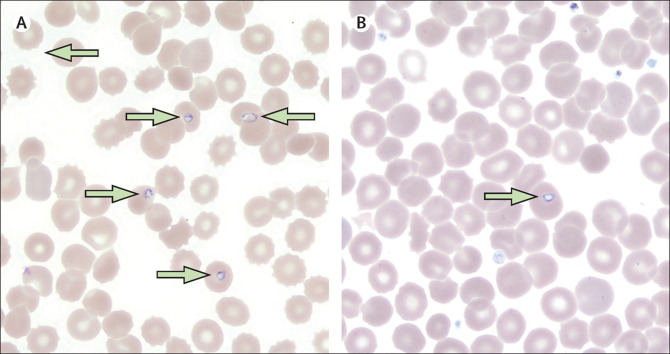
Figure: Fever, haemolysis, and thrombocytopenia caused by babesiosis
The patient was transfused platelets and packed red blood cells and treated for babesiosis with a combination of intravenous clindamycin and oral quinine, which notably cross the placenta. An emergency caesarean was performed the next day; she delivered healthy twin boys who were monitored with daily B microti PCRs and blood smears.
On day 4 of the admission, a single B microti ring-form was identified in twin A’s smear (figure) and on the same day his B microti PCR became positive. Twin B’s B microti smear and PCR remained negative. To prevent symptomatic disease, the twins were treated with oral azithromycin and oral atovaquone.
After the delivery of her twins, the patient had a complicated course of severe babesiosis and eventually after 12 days in hospital she was able to go home; the twins never became symptomatic.
Initially, we considered that our patient might have had a diagnosis of HELLP-Haemolysis, Elevated Liver enzymes, and Low Platelets-syndrome. However, the low to normal blood pressure and normal ALT, which indicated no liver injury, made us think again. Additionally, HELLP is usually preceded by hypertension without fever. Furthermore, blood smears in HELLP may show schistocytes and burr cells, but in this case, we found intraerythrocytic parasites.
The differential diagnosis for HELLP syndrome includes fatty liver of pregnancy, haemolytic uraemic syndrome, thrombotic thrombocytopenic purpura, immune thrombocytopenia, and systemic lupus flare-up-none of these fitted in this case.
Babesiosis is endemic in the New England region of the USA, including Connecticut. Most cases are asymptomatic; asplenic and immunosuppressed individuals, pregnant patients, and the very young (<2 months) and very old (>80 years) are prone to develop symptoms and may have severe disease. Vertically acquired babesiosis, as occurred in twin A, is very rare. In endemic areas, babesiosis should be considered in the list of differential diagnoses of a HELLP-like presentation. The peripheral blood smear should lead to the diagnosis.
(3). Kumar A, et al. Buruli ulcer in Ghana, A Neglected Tropical Disease (NTD). Lancet 2022;399(10327), P786-797.
Buruli ulcer, an NTD and mycobacterial disease of the skin and soft tissue, were taken in Ghana, west Africa. Buruli ulcer is endemic in 33 tropical and subtropical countries and mainly affects poor and remote communities, with the highest burden in Australia and west African countries, including Ghana. When diagnosed late, Buruli ulcer can result in long-term disability and potential disfigurement with resulting stigma. The extensive, open, persistent, and often painless wounds characteristic of Buruli ulcer result from Mycobacterium ulcerans producing mycolactone, a macrolide toxin, that dampens pain and inhibits the immune response, leading to tissue damage. Symptoms occur after exposure to this environmental pathogen, but the mode of transmission is unknown. Early diagnosis of Buruli ulcer is crucial for a good treatment outcome. Yet the initial lesion is often missed or misdiagnosed. The lesions typically increase in size over days or weeks and ulcerate in the centre. In about 10% of cases there is surrounding oedema. Untreated ulcers can cover large areas and affect the bone. A new effective Buruli ulcer treatment regimen involves oral rifampicin and clarithromycin daily for 8 weeks. Skin grafting improves healing in large lesions and physiotherapy reduces movement limitation at joints. Although progress has been made in diagnosis and management since the establishment of the WHO Global Buruli Ulcer Initiative in 1998, many patients in remote rural areas find it difficult to get a diagnosis and access treatment.

(4). Yadav N, et al. Primary hypertrophic osteoarthropathy. N Engl J Med. 2022; 386:e22

A 31-year-old man presented to the internal medicine clinic with 10 years of progressive enlargement of his fingertips and toes and intermittent aches in his distal forearms and lower legs. He had no clinically significant medical history or family history of similar symptoms. Finger and toe clubbing, with a supranormal angle of 210 degrees between the nail bed and the proximal nail fold, was observed on examination. Hyperpigmentation of the proximal nail folds; tenderness to palpation of the distal forearms and lower legs, fingertips, and toes; and widening of the distal forearms and lower legs (Panels A and B, respectively) were also observed. There was no skin thickening or hyperhidrosis. Radiographs of the fingers showed bony proliferation at the tips of the phalanges (Panel C), and radiographs of the ankles showed increased periosteal bone formation at the distal tibia and fibula (Panel D). Serum laboratory tests (including thyroid-function studies), an echocardiogram, and whole-body positron-emission tomography-computed tomography were normal. The patient received a diagnosis of primary hypertrophic osteoarthropathy, a hereditary syndrome characterized by clubbing, periosteal bone proliferation, and (not seen in this case) facial skin thickening and hyperhidrosis, in the absence of systemic conditions. The patient was initially treated with nonsteroidal antiinflammatory drugs for 3 months. Given persistent symptoms, zoledronic acid was administered, and his pain had abated at follow-up 2 months later.
(5). Sanders JJ, et al. Discussing prognosis and what matters most for people with serious illness. BMJ 2022;376:e067572
What we need to know
Serious illness is a health condition that carries a high risk of mortality and either negatively affects a person’s daily functioning or quality of life or excessively strains his or her caregivers. Examples include advanced cancer, end stage organ disease, or motor neuron disease
High quality communication that improves awareness of prognosis and elicits patients’ goals and preferences can improve care quality and patient experience
Clinicians can use structured, evidence-based tools, like the Serious Illness Conversation Guide to engage patients in such communication
Health systems can support the delivery of high-quality serious illness communication through strategies to identify patients with serious illness, train clinicians, prepare patients and families, and ensure documentation that is accessible across multiple points of care
Technological advances in medical care give clinicians unprecedented capability to prolong life. However, this may not be appropriate for patients with serious illness. Serious illness refers to health conditions that carry a high risk of mortality, poor function and quality of life, and strain on caregivers.
For people with serious illness, life prolonging treatments may not align with their preferences or help meet their goals, and may increase their suffering and that of their family members.
A multi-site observational study on patients with serious illness and a randomised controlled trial on patients with advanced cancer suggest that people with serious illness commonly express goals beside simply living longer.
Those who recognise that they are nearing the end of life generally prefer care focused on quality of life and increased time spent at home.
(6). Vousden N, et al. Severity of maternal infection and perinatal outcomes during periods of SARS-CoV-2 wildtype, alpha, and delta variant dominance in the UK: prospective cohort study. BMJMED. 2022;1.
Abstract
Objective: To compare the severity of maternal infection and perinatal outcomes during periods in which wildtype, alpha variant, and delta variant of SARS-CoV-2 were dominant in the UK.
Design: Prospective cohort study.
Setting: 194 obstetric units across the UK, during the following periods: between 1 March and 30 November 2020 (wildtype dominance), between 1 December 2020 and 15 May 2021 (alpha variant dominance), and between 16 May and 31 October 2021 (delta variant dominance).
Participants: 4436 pregnant women admitted to hospital with covid-19 related symptoms.
Main outcome measures: Moderate to severe maternal SARS-CoV-2 infection (indicated by any of the following: oxygen saturation <95% on admission, need for oxygen treatment, evidence of pneumonia on imaging, admission to intensive care, or maternal death), and pregnancy and perinatal outcomes (including mode and gestation of birth, stillbirth, live birth, admission to neonatal intensive care, and neonatal death).
Results: 1387, 1613, and 1436 pregnant women were admitted to hospital with covid-19 related symptoms during the wildtype, alpha, and delta dominance periods, respectively; of these women, 340, 585, and 614 had moderate to severe infection, respectively. The proportion of pregnant women admitted with moderate to severe infection increased during the subsequent alpha and delta dominance periods, compared with the wildtype dominance period (wildtype 24.5% v alpha 36.2% (adjusted odds ratio 1.98, 95% confidence interval 1.66% to 2.37%); wildtype 24.5% v delta 42.8% (2.66, 2.21 to 3.20)). Compared with the wildtype dominance period, women admitted during the alpha dominance period were significantly more likely to have pneumonia, require respiratory support, and be admitted to intensive care; these three risks were even greater during the delta dominance period (wildtype v delta: pneumonia, adjusted odds ratio 2.52, 95% confidence interval 2.06 to 3.09; respiratory support, 1.90, 1.52 to 2.37; and intensive care, 2.71, 2.06 to 3.56). Of 1761 women whose vaccination status was known, 38 (2.2%) had one dose and 16 (1%) had two doses before their diagnosis (of whom 14 (88%) had mild infection). The proportion of women receiving drug treatment for SARS-CoV-2 management was low, but did increase between the wildtype dominance period and the alpha and delta dominance periods (10.4% wildtype v 14.9% alpha (2.74, 2.08 to 3.60); 10.4% wildtype v 13.6% delta (2.54, 1.90 to 3.38)).
Conclusions: While limited by the absence of variant sequencing data, these findings suggest that during the periods when the alpha and delta variants of SARS-CoV-2 were dominant, covid-19 was associated with more severe maternal infection and worse pregnancy outcomes than during the wildtype dominance period. Most women admitted with SARS-CoV-2 related symptoms were unvaccinated. Urgent action to prioritise vaccine uptake in pregnancy is essential.
(7). Zeraatkar D, et al. Use of tocilizumab and sarilumab alone or in combination with corticosteroids for covid-19: A systematic review and network meta-analysis. 2022
Abstract
Objective: To compare the effects of interleukin 6 receptor blockers, tocilizumab and sarilumab, with or without corticosteroids, on mortality in patients with covid-19.
Design: Systematic review and network meta-analysis.
Data sources: World Health Organization covid-19 database, a comprehensive multilingual source of global covid-19 literature, and two prospective meta-analyses (up to 9 June 2021).
Review methods: Trials in which people with suspected, probable, or confirmed covid-19 were randomised to interleukin 6 receptor blockers (with or without corticosteroids), corticosteroids, placebo, or standard care. The analysis used a bayesian framework and assessed the certainty of evidence using the GRADE approach. Results from the fixed effect meta-analysis were used for the primary analysis.
Results: Of 45 eligible trials (20 650 patients) identified, 36 (19 350 patients) could be included in the network meta-analysis. Of 36 trials, 27 were at high risk of bias, primarily due to lack of blinding. Tocilizumab, in combination with corticosteroids, suggested a reduction in the risk of death compared with corticosteroids alone (odds ratio 0.79, 95% credible interval 0.70 to 0.88; 35 fewer deaths per 1000 people, 95% credible interval 52 fewer to 18 fewer per 1000; moderate certainty of evidence), as did sarilumab in combination with corticosteroids, compared with corticosteroids alone (0.73, 0.58 to 0.92; 43 fewer per 1000, 73 fewer to 12 fewer; low certainty). Tocilizumab and sarilumab, each in combination with corticosteroids, appeared to have similar effects on mortality when compared with each other (1.07, 0.86 to 1.34; eight more per 1000, 20 fewer to 35 more; low certainty). The effects of tocilizumab (1.12, 0.91 to 1.38; 20 more per 1000, 16 fewer to 59 more; low certainty) and sarilumab (1.07, 0.81 to 1.40; 11 more per 1000, 38 fewer to 55 more; low certainty), when used alone, suggested an increase in the risk of death.
Conclusion: These findings suggest that in patients with severe or critical covid-19, tocilizumab, in combination with corticosteroids, probably reduces mortality, and that sarilumab, in combination with corticosteroids, might also reduce mortality. Tocilizumab and sarilumab, in combination with corticosteroids, could have similar effectiveness. Tocilizumab and sarilumab, when used alone, might not be beneficial.
(8). An ounce of pandemic prevention is worth a pound of cure. Lancet Microbe. 2022 Mar;3(3):e159.
It is self-evident that the global community was insufficiently prepared for the COVID-19 pandemic because it was not prevented or at least limited to regional outbreaks. Efforts to impress upon authorities the need for adequate pandemic preparedness have a long history, but authorities did not start to give this advice fuller attention until 2020. However, despite the current interest in pandemic preparedness, prevention measures do not involve a quick fix and are therefore still met with resistance. A central premise of pandemic preparedness is that one must plan to tackle the next pandemic not the last one. For this reason, uncertainty must be accounted for; so, planning that is overly specific risks leaving us unprepared.
In a recent review in Science Advances, Aaron Bernstein and colleagues argue that pandemic preparedness will be most impactful if it is built on a foundation of broad proactive, rather than narrow reactive, plans. They highlight that many plans to date involve detecting and containing emerging threats, which amounts to action after the pathogen has caused some level of human disease. Bernstein and colleagues disagree that this is the best approach and conclude that the greatest benefit for the cost is achieved by preventing the spillover of potential zoonoses through effective surveillance and management of the interface between people and animals, given the major source of pandemic risk is viral spillover from animals to humans.
Bernstein and colleagues put it succinctly: “If the current pandemic has taught us anything, then it is that no amount of technology can save us from poor governance once an epidemic takes hold in the human population.” Yet, technological solutions are almost the only interventions enthusiastically promoted by authorities. To genuinely minimise the risk of pandemics, Bernstein and colleagues emphasise the need to put an understanding of viral diversity at the forefront of preparedness efforts. Then we must address key points at which humans and animals intersect: wildlife trade and hunting, intensive agriculture, and destruction of tropical forests. Put simply, preventing spillover of pathogens with pandemic potential requires a change in how we interact with the natural world. A familiar point, but one that cuts across many crucial issues, such as climate change. So the benefits are even greater when this broader context is accounted for.
Maybe it is possible to navigate a course between the two extremes of broad and narrow planning? In a recent review in The Lancet Microbe, Daniel Becker and colleagues outline approaches to prioritise viral discovery in zoonotic reservoirs. This approach makes the almost insurmountable task of understanding viral diversity promoted by Bernstein and colleagues seem manageable. Becker and colleagues used statistical modelling to guide sampling target prioritisation, enhanced through the comparison and validation of predictive models. Systematic validation refined the predictions and optimised wildlife sampling.
Becker and colleagues’ support for systematic validation stems from the need to overcome the various logistical constraints that limit researchers’ ability to sample wildlife for pathogens. The limitation of previous approaches is that the lack of validation or adequate documentation of model performance results in the use of models that offer little, if any, benefit over random sampling. The potential to extend this work in the future to “longitudinal tracking of viral shedding over space and time, the isolation of the live virus from wild animals, and the experimental confirmation of viral replication” will only further shift the balance of cost versus benefit in a favourable direction.
So, approaches and tools that might make significant inroads into the prevention of future pandemics and their enormous tolls on health and society are available. However, they still require foresight and investment that are difficult to come by. What is becoming increasingly clear, although it was never really in doubt, is that the hardest lessons of the COVID-19 pandemic will probably be ignored by governments. And, therefore, they will repeat the mistake of using the last pandemic as a model for addressing the next one. Maybe, with the costs of the COVID-19 pandemic still fresh in their minds, authorities might be persuaded by an argument that the right approach can save them money.
(9). Gupta N, et al. Safety and efficacy of sofosbuvir-velpatasvir-voxilaprevir for re-treatment of chronic hepatitis C virus infection in patients with previous direct-acting antiviral treatment failure in Rwanda (SHARED-3): a single-arm trial. Lancet, 2022.
Summary
Background: Hepatitis C virus (HCV) genotype 4 non-a/d subtypes, which frequently have NS5A resistance-associated substitutions, are highly prevalent in sub-Saharan Africa. These subtypes, particularly genotype 4r, have been associated with higher rates of failure of treatment regimens containing the NS5A inhibitors ledipasvir or daclatasvir, which are the most accessible direct-acting antivirals in low-income countries. Clinical evidence regarding the efficacy of re-treatment options for these subtypes is limited. We aimed to evaluate the safety and efficacy of sofosbuvir-velpatasvir-voxilaprevir for the treatment of adults in Rwanda with chronic HCV infection, predominantly of genotype 4, and a history of direct-acting antiviral treatment failure.
Methods: In this single-arm prospective trial, we enrolled adults (aged ≥18 years) with a HCV RNA titre of at least 1000 IU/mL, and a documented history of direct-acting antiviral failure. Patients were assessed for eligibility at a single study site after referral from hospitals with HCV treatment programmes throughout Rwanda, and participants for whom sofosbuvir-ledipasvir treatment had failed in the previous SHARED trial were also included. Participants with decompensated liver disease or hepatitis B virus co-infection were excluded. Participants were treated once daily with an oral fixed-dose combination tablet containing sofosbuvir (400 mg), velpatasvir (100 mg), and voxilaprevir (100 mg) for 12 weeks. The primary endpoint was the proportion of participants with a sustained virological response 12 weeks after completion of treatment (SVR12) in the intention-to-treat population. Viral sequencing of NS3, NS5A, and NS5B genes was done at baseline in all participants and at end of follow-up (week 24) in participants with treatment failure. The study is registered with ClinicalTrials.gov (NCT03888729) and is completed.
Findings: Between Sept 23, 2019, and Jan 10, 2020, 49 individuals were screened and 40 participants were enrolled. 20 (50%) were female, 20 (50%) were male, median age was 63 years (IQR 56-68), and median HCV viral load was 6.2 log10 IU/mL (5.8-6.5) at baseline. The genotype subtypes identified were 4r (18 [45%] participants), 4k (six [15%]), 4b (five [13%]), 4q (four [10%]), 4l (two [5%]), 4a (one [3%]), 4m (one [3%]), and 3h (one [3%]). One (3%) genotype 4 isolate could not be subtyped, and one (3%) isolate was of unknown genotype. All successfully sequenced isolates (33 [83%]) had at least two NS5A resistance-associated substitutions and 25 (63%) had three or more. 39 (98% [95% CI 87-100]) participants had SVR12. Seven (18%) participants had a total of ten grade 3, 4, or 5 adverse events, including three (8%) cases of hypertension, and one (3%) case each of cataract, diabetes, gastrointestinal bleeding, joint pain, low back pain, vaginal cancer, and sudden death. Four of these events were categorised as serious adverse events resulting in hospitalisation. The one sudden death occurred at home from an unknown cause 4 weeks after the completion of treatment. No serious adverse event was determined to be related to the study drug or resulted in treatment discontinuation.
Interpretation: A 12 week course of sofosbuvir-velpatasvir-voxilaprevir is safe and efficacious for the re-treatment of individuals infected with HCV genotype 4 non-a/d subtypes with frequent baseline NS5A resistance-associated substitutions, following failure of previous direct-acting antiviral treatment. Improved affordability and access to sofosbuvir-velpatasvir-voxilaprevir in regions with these subtypes is crucial.
(10). The DISCHARGE Trial Group, et al. CT or Invasive Coronary Angiography in Stable Chest Pain. N Engl J Med. 2022
Abstract
Background: In the diagnosis of obstructive coronary artery disease (CAD), computed tomography (CT) is an accurate, noninvasive alternative to invasive coronary angiography (ICA). However, the comparative effectiveness of CT and ICA in the management of CAD to reduce the frequency of major adverse cardiovascular events is uncertain.
Methods: We conducted a pragmatic, randomized trial comparing CT with ICA as initial diagnostic imaging strategies for guiding the treatment of patients with stable chest pain who had an intermediate pretest probability of obstructive CAD and were referred for ICA at one of 26 European centers. The primary outcome was major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke) over 3.5 years. Key secondary outcomes were procedure-related complications and angina pectoris.
Results: Among 3561 patients (56.2% of whom were women), follow-up was complete for 3523 (98.9%). Major adverse cardiovascular events occurred in 38 of 1808 patients (2.1%) in the CT group and in 52 of 1753 (3.0%) in the ICA group (hazard ratio, 0.70; 95% confidence interval [CI], 0.46 to 1.07; P=0.10). Major procedure-related complications occurred in 9 patients (0.5%) in the CT group and in 33 (1.9%) in the ICA group (hazard ratio, 0.26; 95% CI, 0.13 to 0.55). Angina during the final 4 weeks of follow-up was reported in 8.8% of the patients in the CT group and in 7.5% of those in the ICA group (odds ratio, 1.17; 95% CI, 0.92 to 1.48).
Conclusions: Among patients referred for ICA because of stable chest pain and intermediate pretest probability of CAD, the risk of major adverse cardiovascular events was similar in the CT group and the ICA group. The frequency of major procedure-related complications was lower with an initial CT strategy.
