Learning from Experience – Chapters 8 – 10
Chapter 8
Elective APR in an Octogenarian
Dr. Vasanthi Vidyasagaran*
Department of Anaesthesiology, Kauvery Hospital, Chennai, Tamilnadu, India
*Correspondence: Vasanthi.vidyasagaran@gmail.com


An 89-year-old, diagnosed with operable carcinoma of the rectum, was posted for anterior perineal resection. Her past medical history was highly significant comprising of an entire list of co-morbidities including insulin dependent diabetes mellitus, hypothyroidism on replacement Eltroxin 50 µg, hypertension on treatment with Hydrochlorothiazide and Amlodipine 10 mg. She had suffered inferior wall MI 4 years ago, with witnessed cardiac arrest during hospital admission, from which she was revived successfully.
On examination, she was pale. Her pulse rate was 64 beats/min, BP 130/90 mm Hg.
Investigations showed haemoglobin level of 9.0 gm/dl, fasting blood sugar level of 110 mg/dl. ECG showed Q waves in leads II and III, AVF and echocardiogram revealed left ventricular hypertrophy, moderate diastolic dysfunction, no regional wall motion abnormality, left ventricular ejection fraction 35%, no significant valvular abnormality except for a mild aortic stenosis.
She was premedicated with Promethazine12.5 mg and Pentazocine15 mg IM, 45 minutes before surgery. To prevent dehydration, maintenance fluid Ringer Lactate was started at 50 ml/hour ten hours prior to surgery.
The surgery was planned under a combined epidural and general anaesthesia. Attention to detail was given at every stage as enlisted below:
- Preoperative fluid status optimization (post bowel preparation)
- Euthyroid status ensured
- Cardiac drugs given
- Glucose control with Insulin
- Care during movement and positioning (elderly, osteoporotic bones)
- Smooth anaesthesia with stable haemodynamics, bearing in mind to maintain MAP >80 mmHg (shift in auto regulatory curve to the right in octogenarians)
- Urine output monitoring
- Temperature control
The epidural catheter tip was placed at T12. Intra operative vitals were monitored. CVP line was placed (knowing its limitations) for two reasons – to titrate intravenous fluid administration and for inotropes if needed. Continuous non-invasive cardiac output monitoring was contemplated, we had it ready in case there was any major bleed during surgery.
Hypotension (80/50 mm Hg) was encountered after the first epidural bolus dose (5cc 0.25% Bupivacaine) which recovered with a single dose of 3 mg Ephedrine. The surgery was completed uneventfully in 4 hours after which she was reversed and extubated on table. Meticulous care was given in maintaining haemodynamics, and avoiding hyperventilation. Urine output maintained at 0.5 ml/kg/hour, suggesting adequate renal perfusion. Neuromuscular monitoring and BIS monitoring were done.
Postoperatively she was shifted to a high dependency unit, with attention to input/output, oxygenation, early mobilization, and prevention of deep vein thrombosis (DVT). Most postoperative cardiac and respiratory events happen within first 24 hours. She was shifted to the ward on the second postoperative day, and discharged home on day 7. She was subsequently taken up for colostomy closure, and anastomosis (another major procedure) She has been attending yearly follow up and doing well 15 years down the line. This may be the longest post-operative follow up of a patient by an anaesthetist! And she has hit a century!
Discussion
At the outset, this patient with such a significant medical history will probably be refused by any anaesthesiologist (at that time, when facilities were much lesser than the present days) due to high peri- operative risk of mortality for such a major morbid procedure. Age > 80 years, presence of heart failure, severity of coexisting disease and extent of invasive surgery account for surgical risk and outcome.
But examining her as a whole, her attitude, family support and willingness to undergo surgery gave the team the inclination and courage to take up this case with informed consent. Also, the need for surgery in a malignancy was a valid reason to proceed. The decision to take up the patient for the procedure depends to a great extent on the skills, knowledge and attitude of the surgeon involved. This criterion cannot be overlooked.
Aging and anaesthesia:
- Age related progressive loss of functional reserve.
- Increased sensitivity to anaesthetic drugs.
- may affect the brain, heart, respiration, and vasomotor tone.
- Labile blood pressure may need continuous monitoring and appropriate correction.
- Respiratory depressant effect exaggerated in perioperative period.
- Perioperative analgesia-quite tricky, can tilt the balance, unless titrated carefully.
- Prevention of nausea, vomiting, POCD, post-operative respiratory depression, and maintaining adequate renal function are main focus.
Anaesthesia plan to reduce perioperative morbidity and mortality in similar cases:
- Preoperative optimisation as mentioned above, based on ERAS (Enhanced Recovery after Surgery) guidelines. Low carbohydrate drink given previous 24 hours, oral liquids given up to 2 hours before, to maintain volume status. Glucose control in diabetic patient’s essential.
- It is advised to maintain euvolemic status and not overload patient.
- DVT Prophylaxis.
- Antibiotic prophylaxis.
- Smooth GA+/- epidural. Epidural induced hypotension may be very harmful. So, it must be placed and used only in selected patients. Fentanyl patch is a good alternative option for postoperative analgesia.
- Prevent postoperative nausea and vomiting and hypothermia.
- NG tube removed at end of surgery provided there is no indication to retain it in the post- operative period. Plan to proceed with early oral feeding.
- Postoperative care plan must be clearly documented and checked personally.
References
- Gustafsson UO, et al. Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2013;37:259-84.
- Turrentine FE, et al. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865.
- Dodds C. Physiology of ageing. Anaesth. Intensive Care Med. 2006;12:456-8.
- Dodds C, et al. Day Case Anaesthesia in the elderly. CPD Anaesthesia 1999;1:3.
- The Anaesthesia Team. The Association of Anaesthetists of Great Britain and Ireland. August 1998.
- Rivera R, et al. Perioperative drug therapy in elderly patients. Anesthesiology 2009;110:1176.
- Phillip B, et al. The prevalence of preoperative diastolic filling abnormalities in geriatric surgical patients. Anesth Analg. 2003;97:1214.
Choose your surgeon – compatibility between surgeon and anaesthetist is important for the welfare of the patient and of yourself.
A holistic approach to any situation will make you a successful anaesthesiologist.
Chapter 9
Hypertensive Crisis in a Patient with Cataract even before the Procedure
Elderly patient for cataract surgery under local anaesthesia
A 78-year-old man, with history of hypertension well controlled, was posted for cataract surgery under local anaesthesia. Patient received phenylephrine drops as mydriatic. Soon after that he began to feel uncomfortable, sweaty and clammy. His blood pressure was 190/120 mm Hg. The anaesthetist was only then called for! Fortunately, he was available.
Patient was reassured, oxygenated, and sedated with 2 mgs midazolam. Measures were taken to reduce blood pressure to normal levels. IV Esmolol boluses were used. His ECG showed ischemic changes for about 30 minutes, during which time he was under observation and a physician was called for. Blood pressure came down to 140/94, patient recovered well and advised to follow up with his physician. Surgery was postponed.
Discussion
Phenylephrine 2.5% one drops each eye is the dose needed. But often errors happen with excess application and this leads to erratic systemic absorption. Variety of medical emergencies may get precipitated in these patients. Transient but very high increase in blood pressure with topical eye drops may occur. The drug is used on regular basis before cataract surgery for dilatation. These patients usually are elderly with known hypertension and/or diabetes, with autonomic dysfunction. The topical eye drops can cause steep rise in BP and arrhythmias leading to ischemic events. It may even precipitate cardiac arrest. It is important to ensure 10% Phenylephrine is not used.
It should be remembered that they may be suffering from BHP, and may develop postoperative urinary retention, which makes it extremely uncomfortable for the patient post cataract surgery. Hence it is important to evaluate the patient as a whole in the pre-operative period itself.
Other ophthalmic drugs and side-effects:
- Pilocarpine: Used to reduce intraocular pressure. May cause bradycardia, hypotension and bronchospasm. Vagotonic like Halothane may aggravate the cardiac effects.
- Anticholinergic drugs: Atropine, Cyclopentolate, Tropicamide used for mydriasis, may precipitate Central anticholinergic syndrome with disorientation, convulsion, and psychosis.
- Adrenergic antagonists: Timolol eye drops for Glaucoma – may produce systemic beta blockade. It should be cautiously used in patients with obstructive airway diseases, congestive cardiac failure, heart block and diabetes.
- Topical local anaesthetics: Most of them are free of complications. However inappropriate use by patients or applicator may cause corneal ulceration or perforation which can lead to systemic absorption.
It is not advisable to start even minor ophthalmic procedures under local anaesthesia without the presence of an anaesthesiologist, and a proper theatre setting with all necessary resuscitation equipment.
Ophthalmic general anaesthesia is often challenging, because patient groups involved are usually extremes of age with comorbidities, requiring particular attention to detail. Paediatric ophthalmic anaesthesia is a great challenge as these children invariably have co-existing congenital anomalies and are often syndromic children with difficult airway. They may also be brought for repeated procedures requiring multiple anaesthesia during a short span of time.
References
- Fraunfelder FW, et al. Adverse systemic effects from pledgets of topical ocular phenylephrine 10%. Am J Ophthalmol. 2002;134:624-5.
- Baldwin FJ, et al. Intraoperative pulmonary oedema in a child following systemic absorption of phenylephrine eye drops. Br J Anaesth. 2002;88:440-2.
- Barash PG, et al. Clinical Anaesthesia. 5th ed. Lippincott Williams & Wilkins, Philadelphia, 2006:974-98.
The drugs or the techniques in anaesthesia practice are just a handful but the drug interactions during anaesthesia is enormous and widely variant.
Thorough knowledge is essential to handle such a situation.
Chapter 10
Implantable Cardiac Device
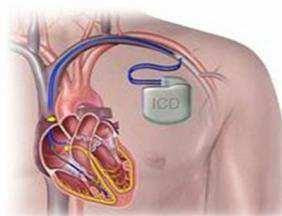
A 44-year-old man was admitted with knee injury. He was diagnosed to have patellar fracture. He was posted for ORIF as day-care. He gave no history of hypertension, diabetes or any other comorbidities. The anaesthetist examined the patient just before surgery and it was identified that he had cardiac pacemaker device fitted. The surgeon had no idea that the patient had a cardiac device! On further questioning, patient revealed that he had pacemaker fitted 10 years ago for complete heart block and he had followed up with his cardiologist, but had no records in hand. He also gave history of syncopal attacks two years ago. A new ICD was fitted in at that point but the history did not provide us with details of diagnosis. He was asymptomatic now, and did not think it was of any relevance for surgery on his knee!
No history of chest pain, dyspnoea or palpitations. On examination vitals were normal and chest was clear. Hence at this juncture, with a complicated history and potential cardiac events in the perioperative period, the patient was considered inappropriate for day care, though the surgical procedure itself was minor. Thorough cardiac workup was requested and the case was postponed to be taken up after cardiology opinion. Haematological investigations, ECG and ECHO were requested. Implanted cardiac device check was done.
The device was a pacemaker and implantable cardiac defibrillator combination device. The device was programmed for pacing due to his complete heart block and then defibrillating option was added due to sustained ventricular tachycardia causing syncopal attacks. Following discussion with cardiologist, and the site of surgery being more than 10 cm away from device and risk of electromagnetic interference very minimal, the device was left unaltered.
The pros and cons were explained to the patient and relatives. The plan was to perform the procedure under sedation and femoral nerve block. Patient was premedicated with oral .5 mg alprazolam and shifted to operating theatre.
Precautions taken:
- Defibrillator was made readily available in theatre in case of emergency and malfunctioning of device.
- Electromagnetic interference was minimized by avoiding proximity of cautery tool to pulse generator leads.
- Short bursts at lowest possible energy were used.
- Bipolar cautery and ultrasonic scalpel was used,
Surgery was performed as planned, under nerve block and sedation, patient recovered uneventfully.
Discussion
This case is presented because this kind of situation is more likely to occur in present day practice and in future. It is important to know the implication and perioperative management of such patients. Never be hesitant to defer a case in view of safety. Indications for placement of pacemaker and implantable cardiac defibrillator have to be known to have an idea about management of any perioperative complications with rate and rhythm. Knowledge of type of device and working method is essential, especially while anaesthetising patients for major surgical procedures.
Questions to ask:
Will there be electromagnetic interference?
- Is the patient pacemaker dependent and if yes, is the distance from source of EMI <15 cm: If so reprogram to asynchronous mode
- If not dependent – no reprogramming is necessary, have magnet available. Magnet may be used to temporarily stop the anti-tachyarrhythmia function of the device so that external defibrillator may be used in event of tachyarrhythmia.
- If device is >15 cm away depending on type of surgery, judgment has to be made whether placing in asynchronous mode is required or not.
Discussion with cardiologist and immediate availability of pacemaker technician at time of surgery is important. It must be borne in mind that sudden jerky movement of patient, fasciculation from Suxamethonium can be judged as fibrillation and device turned on, which can be detrimental. Emergency drugs must be immediately available.
Should the need for defibrillation arise, device must be disabled with magnet or reprogramming and then paddles must be placed in axis perpendicular to device/ anteroposterior.
Postoperatively, the device must be reprogrammed to original mode in the recovery area. Patient must be monitored closely for rate and rhythm. Defibrillator facilities must be available in the post-operative ward.
References
- Practice Advisory for the Perioperative Management of Patients with cardiac rhythm management devices: pacemakers and ICD’s: a report by the American Task Force on perioperative management of patients. Anesthesiology 2005;103:186-8.
- Practice Advisory for the Perioperative Management of Patients with Cardiac Electronic Devices: Pacemakers and Implantable Cardioverter Defibrillators. An updated report by the American Society of Anesthesiologist Task Force on Perioperative Management of patients with cardiac Implantable Electronic Devices. Anesthesiology 2011;114:247-61.
- Barash PG, et al. Stoelting Clinical anesthesia sixth edition, Appendix: Electrophysiology 1586-7.
