Effectiveness of Rood’s approach based paediatric Occupational Therapy Management: On Children with Congenital Muscular Torticollis
M. Mahendran*
Consultant Paediatric Occupational Therapist, Unit of Hamsa Kids for Rehabilitation, Kauvery Hospitals, Trichy, India
*Correspondence: maherichy987@gmail.com
Abstract
Purpose:This study explores the effect and impact of Paediatric Occupational Therapy Interventions for Infants with Torticollis.
Methods:Data was extracted from electronic medical records between January 2023 and March 2023 to describe infants with Congenital Muscular Torticollis (CMT) who received physiotherapy.
Results:Infants met diagnostic criteria. Symptoms and signs of Torticollis were noticed by 6 months in 90% of infants, and with an occupational and physical therapy examination before 6 months in 100% of infants. Most infants had early mild CMT and greater limitation in active cervical range of motion (ROM) than passive cervical ROM. Clinicians frequently recommended weekly occupational and physical therapy that included first-choice and supplemental interventions. Episodes of care averaged weekly-5 days with 73% of infants meeting goals.
Conclusion:Paediatric occupational therapists should treat infants who have occupational therapy which resolves symptoms and improves signs
Keywords: Infantile, Paediatric occupational therapist, Torticollis
Background
Congenital muscular torticollis occurs from shortening or disproportionate contraction of the sternocleidomastoid (SCM) muscle. The reported incidence varies between 0.41.9%. Various theories have been proposed, but their true etiology remains obscure. The deformity is characterized by an almost painless, constricted and cordlike SCM muscle, which pulls the head toward the side affected, narrows and draws the shoulder upward, forcing the chin in the opposite way. Pediatrics Occupational Therapy (CMT) treatment helps to restore full neck movement as early as possible and helps reverse or control the progression of neck regional deformity, cranial facial asymmetry, and to prevent bones and postural alignment changes that may root cause asymmetric motor development. An occupational therapist would assess the infant’s range of motion and head shape, and develop a stretching program, and counsel the family suitably. (IEP) Intervention will often include strategies for positioning and playing with the baby in a way that encourages dynamic movement to the non-preferred side. When identified and treated early, majority of infants with Torticollis recover with no long-term adverse effects.
Research Methodology
| Population | Sampling size | Sample techniques | Study place | Variables | Duration of the study |
| Accessible population was adapted in this study. | Mono subjects are included in this study. | Convenient sampling technique was adapted. | The subjects were selected from Unit of Hamsa Rehab centre, Kauvery Hospitals, Trichy,
Tamil Nadu. |
Independent variables; Occupational therapy sensory play-based management Dependent variables; Torticollis
|
Total duration of the study was 8 weeks. |
Case Presentation
The patient affected with congenital muscular torticollis was a 0.8-year-old infant female baby (Fig. 1) involving mild asymmetry of sternocleidomastoid muscles (SCM), left > right. The infant was the first-born, with no positive family history of muscular torticollis. Congenital muscular torticollis was diagnosed in the first year of life. The baby had undergone occupational therapy of active neck stretching activities at the age of 0.6 months as part of the rehabilitation process in KMC hospital, a unit of Hamsa rehab centre, Trichy India. Detailed medical history revealed no events of abnormal obstetric presentation during birth or episodes of gross trauma, unusual or prolonged infection, or associated pain in the neck. No other congenital abnormality existed.
This study was conducted on the infant with Torticollis for 8 weeks. In this study, one infant, age 0.8 years, was included. Initially, permission to do the study was received from the child’s parents or caregiver by getting the consent form signed. Then details such as name, age, sex, history of Torticollis were taken by using an assessment form and the procedure was explained to the parents or caregiver. Pre and Post-test data were collected through Sensory Profile – 2 and Manual muscle power test (MMT), using evidence based occupational therapy interventions. The collected data was divided into two variables based on intervention. The Occupational therapy intervention plan was based on Activity Configuration Approach. Further, the data was analysed by calculating mean value, t value and p value.
Paediatric Occupational Therapy Management on infants with Torticollis-Session schedule
Intervention
The therapy was planned for 8 weeks. It was a 45 min group session with the frequency of 5 days a week. Total of 8 treatment sessions (each session of 5 days) was planned for infant.
Session Schedule
| Week 1 | Warm-up | Main activities |
| Session 1 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Arm wake-up
aerobics-jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Week 2 | Warm-up | Main activities |
| Session 1 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Week 3 | Warm-up | Main activities |
| Session 1 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Week 4 | Warm-up | Main activities |
| Session 1 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Week 5 | Warm-up | Main activities |
| Session 1 | Arm wake-up
Pencil aerobics |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Arm wake-up
aerobics -jumping |
Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Week 6-8 | Warm-up | Main activities |
| Session 1 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 2 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
| Session 3 | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity
-stair calming, kneeling, rollover |
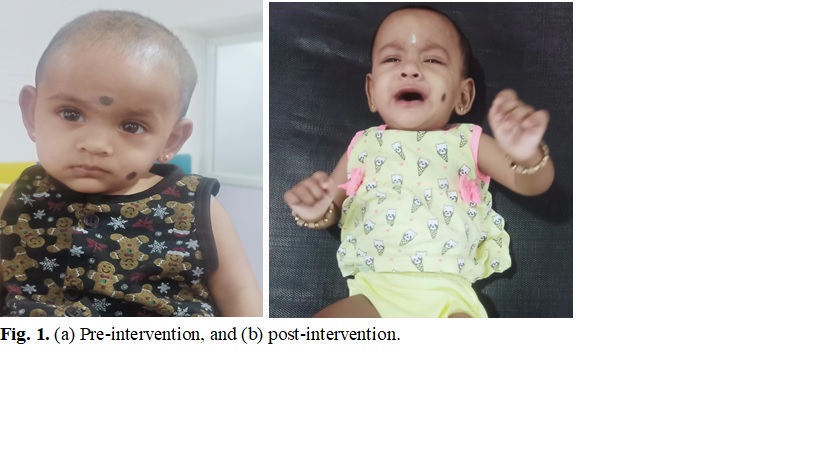
Fig. 1.(a) pre-intervention, and (b) post-intervention.
Data Collection or Statistical Analysis
- This study, collected data on pre and post-intervention.
- Statistical tests were performed using a statistical package for graph pad instate software version 3.1 respectively.
Table 1: Characteristic of data pre and post evaluation – Denver developmental profile
| Characteristic of data paired t-test | Denver (pre-test performance) | Denver (post-test performance) |
| Mean | 55.71 | 77.14 |
| Standard deviation | 13.97 | 9.51 |
| Sample size | 1 | 1 |
| The standard error (SE) means | 5.28 | 9.51 |
| 95% confidence interval | -31.32 | 11.54 |
Table 1 data shows of pre-post-evaluation (Denver scale)- of subject, mean values are 55.71 and 77.14, respectively standard deviation 13.97 and 9.51 respectively sample size 01, standard error of mean 5.28 and 9.51, 95% confidence interval -31.32 and 11.54, respectively.
Table 2: Characteristic of data pre and post evaluation- Denver developmental profile
| S.No. | Variable 1 | Variable 2 | value | t-value | Level of significance |
| 1 | Pre-test evaluation | Post-test evaluation | 0.0018 | 5.3033 | Statistically significant |
Table 2 shows that comparison between the pre-post-evaluation- Denver scale of the subject, t’ value is 5.3033 p-value is 0.0018, This difference is considered to be very statistically significant.
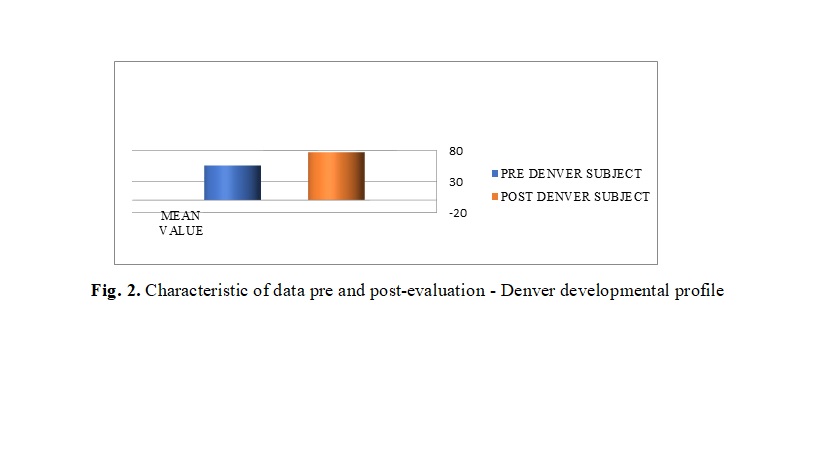
Fig. 2. Characteristic of data pre and post-evaluation – Denver developmental profile.
Table 3: Characteristic of data pre and post evaluation- Toddler sensory profile-2
| Characteristic of data paired t-test | Toddler sensory profile-2 (pre-test performance) | Toddler sensory profile-2(post-test performance) |
| Mean | 88.75 | 39.25 |
| Standard deviation | 22.50 | 20.79 |
| Sample size | 1 | 1 |
| The standard error (SE) means | 11.25 | 10.40 |
| 95% confidence interval | 13.53 | 85.47 |
Table 3 shows the pre-post-evaluation (Toddler sensory profile-2) of the subject, mean values are 88.75 and 39.25, respectively standard deviation 22.50 and 20.79 respectively sample size 01, standard error of the mean of 11.25 and 10.40, 95% confidence interval 13.53 and 85.47, respectively.
Table 4: Characteristic of data pre and post evaluation- Toddler sensory profile-2
| S.No. | Variable 1 | Variable 2 | value | t-value | Level of significance |
| 1 | Pre-test evaluation | Post-test evaluation | 0.0220 | 4.3795 | Statistically significant |
Table 4 shows that comparison between the pre-post-evaluation-Toddler sensory profile-2 of subject,t’ value is 4.3795 p-value is 0.0220, This difference is considered to be statistically significant.
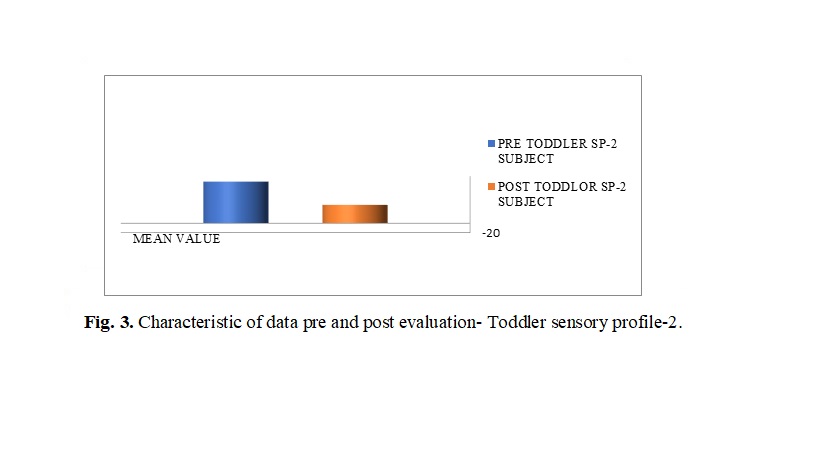
Fig. 3. Characteristic of data pre and post evaluation- Toddler sensory profile-2.
Table 5: Characteristic of data pre and post evaluation – Manual Muscle Power Grade Test (MMT)
| Characteristic of data paired t-test | MMT (pre-test performance) | MMT (post-test performance) |
| Mean | 65.00 | 85.00 |
| standard deviation | 30.00 | 19.15 |
| Sample size | 1 | 1 |
| The standard error (SE) means | 15.00 | 9.57 |
| 95% confidence interval | -45.98 | 5.98 |
Table 5 shows of pre-post-evaluation Manual Muscle Power Grade Test (MMT) of the subject, mean values are 65.00 and 85.00, respectively standard deviation 30.00 and 19.15 respectively sample size 01, standard error of mean 15.00 and 9.57, 95% confidence interval -45.98 and 5.98, respectively.
Table 6: Characteristic of data pre and post-evaluation – Manual Muscle Power Grade Test (MMT)
| S.No. | Variable 1 | Variable 2 | value | t-value | Level of
significance |
| 1 | Pre-test evaluation | Post-test evaluation | 0.0917 | 2.4495 | No statistically significant |
Table 6 shows that comparison between the pre-post-evaluation-Manual Muscle Power Grade Test (MMT)of the subject,t’ value is 2.4495 p-value is 0.0917, This difference is considered to be not quite statistically significant.
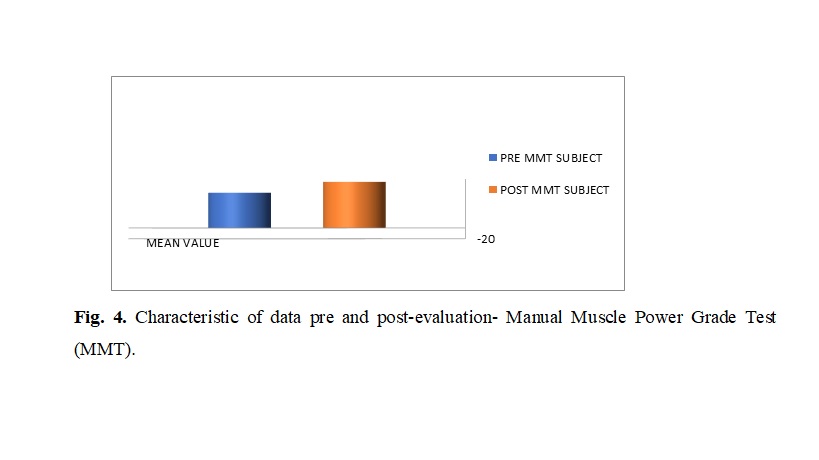
Fig. 4. Characteristic of data pre and post-evaluation- Manual Muscle Power Grade Test (MMT).
Table 7: Characteristic of data pre and post evaluation- Range of motion (ROM)
| Characteristic of data paired t-test | Range of motion (pre-test performance) | Range of motion (post-test performance) |
| Mean | 42.50 | 61.25 |
| Standard deviation | 32.27 | 18.87 |
| Sample size | 1 | 1 |
| The standard error (SE) means | 16.14 | 9.44 |
| 95% confidence interval | -58.99 | 21.49 |
Table 7 shows the pre-post-evaluation (Range of motion ) of the subject, mean values are 88.75 and 39.25, respectively standard deviation of 42.50 and 61.25, respectively sample size 01, standard error of the mean of 16.14 and 9.44, 95% confidence interval -58.99 and 21.49, respectively.
Table 8: Characteristic of data pre and post-evaluation- Range of motion
| S.No | Variable 1 | Variable 2 | value | t-value | Level of significance |
| 1 | Control pre-test evaluation | Control post-test evaluation | 02348 | 1.4828 | No statistically significant |
Table 8 shows that comparison between the pre-post-evaluation- Range of motion of the subject,t’ value is 4.3795 p-value is 0.0220, This difference is considered to be statistically significant.
Fig. 5. Characteristic of data pre and post-evaluation – Range of motion.
Discussion
Torticollis occurs in 0.42% of all births. The etiology is to some extent understood, even though multiple theories exist, including intrauterine crowding or vascular phenomenon, fibrosis from peripartum bleeds, a compartment syndrome, and a primary myopathy of the sternocleidomastoid muscle. A history of difficult birth was found in 3060% of infants with torticollis. Few studies showed that 90100% of infants with CMT who received early occupational therapy treatment improved within the first year of life. In this study, Paediatric occupational therapy resulted in an acceptable response rate in a high proportion of cases with complete resolution of symptoms.
Conclusion
From the result of this study, it was concluded that there is a significant effect of Occupational Therapy interventions on infants with Torticollis.
REFERENCE
- Sland Therapy Solutions, LLC Pediatric Occupational Therapy (340) 719-7007 www.islandtherapysolutions.com
- Mohan M, Bhat S, Prasad R, Sharma SM, Jain TL. Congenital muscular torticollis-case report and an effective treatment plan. J Maxillofac Oral Surg. 2012;11(3):364-7.
- Rajesh Kumar R, Manish Kumar, Abhijit Subhash, Saurav Kumar, Pankaj Kumar. Case report on torticollis. IJOS. 2017;3(4):615-617.
- The Emily Center; Torticollis, 602-933-1395 Health Education Specialist Phoenix Children’s Hospital.
- Guralnick, M., Hammond, M, Connor. Subtypes of non-social play: Comparisons of children with and without developmental delays. Am J Ment Retard. 2003;108 (5):247362.
- Hoza, B., Mrug, S., Pelham, W., Greiner, A, Gnagy. A friendship intervention for children with attention-deficit hyperactivity disorder: Preliminary findings. J Attent Disord. 2003;6(3):8798.
- Stockmeyer SA. An interpretation of the approach of Rood to the treatment of neuromuscular dysfunction. Am J Phys Med. 1967;46(1):900-61.

Dr. Mahendran
Consultant Paediatric Occupational Therapist
