Journal scan: A review of 35 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Tulika Chatterjee. A Case of Gigantic Unruptured Abdominal Aneurysm Successfully Treated With Endovascular Repair (EVAR). 2022.
Aortic aneurysms are focal dilations of more than 50% the normal aortic diameter; giant abdominal aortic aneurysms (AAAs) have diameters greater than or equal to 10 cm and are rare clinical entities. We present a case of an elderly man with an AAA with a 14.6-cm diameter, treated successfully with endovascular repair (EVAR). AAAs pose anatomical challenges for EVAR because of their narrow necks, extreme angulation, and dislocation of intra-abdominal organs. A literature review shows only 5 EVARs have been attempted for the repair of giant AAAs; 4 were successful. With the technical advancement and careful patient selection, successful EVAR of giant AAAs is possible.
Background
An aortic aneurysm is a focal dilation of 50% or more over the normal aortic diameter. The most frequent form of aortic aneurysms is infrarenal aneurysms, which are strongly associated with smoking (1). The definition of a giant abdominal aneurysm varies in the literature, but the most inclusive definition is an abdominal aortic aneurysm (AAA) diameter equal to and larger than 10 cm (2-4). Current aggressive screening practices and a high propensity of rupture beyond a 5-cm diameter make giant AAA a relatively rare clinical entity. As the size of the AAA increases, anatomical challenges such as tortuosity and extreme angulation of the neck also increase. As a result, open surgical repair is needed in most cases of giant AAA, and very few endovascular repair (EVAR) attempts for giant AAA are reported in the literature. We present a case of giant AAA with a diameter of 14.6 cm successfully treated with EVAR.
Objective
Giant AAA is a life-threatening condition if undiagnosed and untreated so, age-appropriate and risk factor-based AAA screening and monitoring are important. It is unclear why certain AAAs continue to expand to gigantic sizes without rupture. The large size of an AAA can pose anatomical challenges for endovascular repair, and patients often need invasive open surgical repair. This case report emphasizes that EVAR can be successful in carefully selected patients, especially with recent advancements in aortic endograft devices and deployment techniques.
Case Report
An 84-year-old man with a medical history of hyperlipidemia, hypertension, hypothyroidism, tobacco use, and AAA was admitted for the management of an asymptomatic, 14.6-cm infrarenal abdominal aneurysm. The patient was recently evaluated at an outpatient clinic and noted to have an abdominal mass with pulsations. The patient did not report shortness of breath, dizziness, nausea, vomiting, lower extremity weakness, or abdominal, back, or chest pain. The last known size of his AAA was 3 cm 9 years previous. Of note, the patient had a 20-pack-year smoking history and for the past 10 years has been smoking pipe tobacco. On arrival, the patient was afebrile, with a blood pressure of 120/76 mm Hg, pulse rate of 73 beats/min, and respiratory rate of 16/minute. Physical examination was pertinent for a well-defined large pulsatile mass palpable in the epigastric region with a soft bruit audible on auscultation. Pulses were palpable in the lower extremities bilaterally. Complete blood count and electrolyte levels were within normal limits. A computed tomographic angiogram (CTA) of the abdomen and pelvis demonstrated a saccular aneurysm of the abdominal aorta measuring 14.6 cm × 12.6 cm in the greatest transaxial dimension and a craniocaudal dimension of 14.7 cm (Figure 1). The aneurysm extended to the aortic bifurcation with normal-sized iliac arteries. There were dense calcifications of the iliac vessels, but no narrowing was observed. The right ureter was significantly displaced anterolaterally because of the dilated abdominal aorta. There were no signs of impending rupture. Even with an aneurysmal neck angulation of greater than 60 degrees and tortuosity of the neck, it was thought that the patient would be best suited for EVAR because of his elder age, frailty, and functional status. Despite the previously mentioned difficult anatomy, the patient underwent a successful EVAR with aortic endograft placement. The postoperative angiogram showed no endoleak, with good perfusion to both renal arteries as well as both internal iliac arteries and common iliac arteries (Figure 2). The patient did well postoperatively and was discharged in stable condition. Four months after the EVAR, a repeat CTA of the abdomen showed no endoleak (Figure 3) and the patient did well clinically as well.
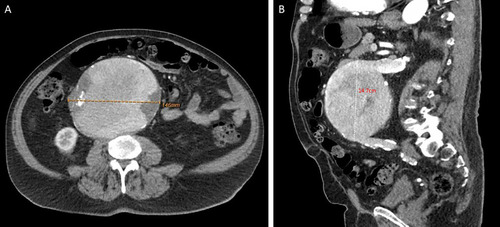
Fig. 1.
Computed tomographic angiogram (CTA) of the abdomen and pelvis. (A) Axial view demonstrating a 14.6-cm diameter unruptured infrarenal abdominal aneurysm. (B) Sagittal view demonstrating the 14.7-cm craniocaudal length of the infrarenal abdominal aneurysm.
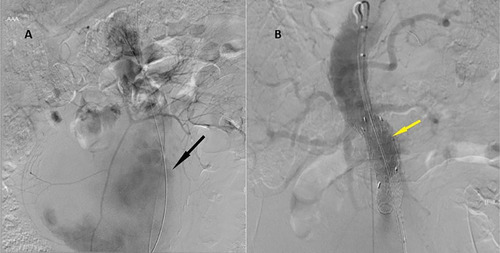
Fig. 2.
(A) Abdominal aortic aneurysms before endograft insertion (black arrow). (B) Successful placement of a Gore conformable endograft in an infrarenal position. Bilateral iliac limbs were deployed just proximal to bilateral hypogastric arteries. The graft seemed to be in a good position with no appreciable endoleak (yellow arrow).
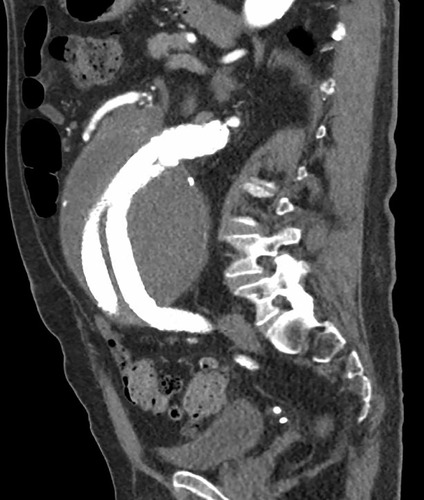
Fig. 3.
A computed tomography scan taken 4 months after the procedure showed no endoleak.
The incidence of AAA is 4% to 8% in men aged 65 years and older, whereas it is much less frequent in women of the same age group, with an approximate incidence of 1.3% (1). The cutoff diameter for defining giant AAA varies in the literature, ranging from 10 to 13 cm (1-3). Most AAAs are diagnosed when they are less than 6 cm in diameter. The annual risk for rupture reaches 30% to 40% once the diameter is more than 8 cm (4). Recent data suggest that the risk for rupture starts to increase exponentially when the diameter of the AAA reaches between 5 and 6 cm (1). Because the rupture rate increases substantially with increasing size, AAAs larger than 10 cm are rarely seen clinically (3). Moreover, rigorous surveillance protocols of AAA lead to elective repair even before they become symptomatic or reach the size of 5.5 cm. This further reduces the incidence of gigantic aneurysms (2). The literature reports an annual incidence of gigantic AAAs of approximately 0.03% (3). The most common modifiable risk factor associated with the occurrence, enlargement, and rupture of AAA is smoking. Even though the incidence of AAA is 4 times more in males, the risk for rupture is 4 times more in females for the same aortic diameter (2). Some of the known factors associated with the risk for rupture are family history, size, shape, rate of size increase, and wall stress (1), but it is still unclear why some of the AAA reach gigantic size without rupture.
Ng et al, in their comprehensive literature review, reported 40 cases of giant AAA, including 4 patients in their case series. The AAA size ranged from diameters of 10 cm to 25.6 cm, which is the largest reported in current literature. Most patients were aged 65 years and more than 87% were males. Of these 40 patients, only 3 had successful EVAR. An overwhelming number of patients required open repair (3). Short neck size of the aneurysm, tortuosity of the neck, extreme neck angulation, and intra-aneurysmal thrombus are some of the anatomical challenges to performing EVAR in most cases of giant AAA (5, 6). Sometimes, because of the large size of the aneurysm, internal organs are displaced, and viscera can be adherent to the aneurysm wall along with possible fistula formation, making EVAR impractical (7). However, since its advent in the early 1990s, endovascular technology and endograft manufacturing have undergone tremendous advancement to overcome procedural challenges (5). With the advent of newer aortic grafts and flexible guidewires, EVAR is being attempted more frequently, even in anatomically challenging cases.
As opposed to open repair, EVAR is minimally invasive, with reduced intraoperative and perioperative mortality, which is found to be quite suitable for elderly patients with multiple comorbid conditions. Despite the perioperative safety of EVAR, it is not without its own long-term complications, which include endoleak, graft migration, and secondary ruptures (5).
Our patient case is unique because no other case of giant AAA of this magnitude has been reported in the literature with successful management with EVAR. The 3 reported cases of giant AAA managed with EVAR had diameters less than or equal to 10.3 cm. One EVAR was attempted in a 25-cm AAA but resulted in the patient’s death on day 8 after the procedure
(2). Matthias K Auer, et al., Congenital adrenal hyperplasia. Lancet 2023; 401(10372), P227-244. Summary
Congenital adrenal hyperplasia is a group of autosomal recessive disorders leading to multiple complex hormonal imbalances caused by various enzyme deficiencies in the adrenal steroidogenic pathway. The most common type of congenital adrenal hyperplasia is due to steroid 21-hydroxylase (21-OHase, henceforth 21OH) deficiency. The rare, classic (severe) form caused by 21OH deficiency is characterised by life-threatening adrenal crises and is the most common cause of atypical genitalia in neonates with 46,XX karyotype. After the introduction of life-saving hormone replacement therapy in the 1950s and neonatal screening programmes in many countries, nowadays neonatal survival rates in patients with congenital adrenal hyperplasia are high. However, disease-related mortality is increased and therapeutic management remains challenging, with multiple long-term complications related to treatment and disease affecting growth and development, metabolic and cardiovascular health, and fertility. Non-classic (mild) forms of congenital adrenal hyperplasia caused by 21OH deficiency are more common than the classic ones; they are detected clinically and primarily identified in female patients with hirsutism or impaired fertility. Novel treatment approaches are emerging with the aim of mimicking physiological circadian cortisol rhythm or to reduce adrenal hyperandrogenism independent of the suppressive effect of glucocorticoids.
(3). The National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury Clinical Trials Network, et al. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension. N Engl J Med. 2023;388(6):499-510. Abstract Background:
Intravenous fluids and vasopressor agents are commonly used in early resuscitation of patients with sepsis, but comparative data for prioritizing their delivery are limited.
Methods:
In an unblinded superiority trial conducted at 60 U.S. centers, we randomly assigned patients to either a restrictive fluid strategy (prioritizing vasopressors and lower intravenous fluid volumes) or a liberal fluid strategy (prioritizing higher volumes of intravenous fluids before vasopressor use) for a 24-hour period. Randomization occurred within 4 hours after a patient met the criteria for sepsis-induced hypotension refractory to initial treatment with 1 to 3 liters of intravenous fluid. We hypothesized that all-cause mortality before discharge home by day 90 (primary outcome) would be lower with a restrictive fluid strategy than with a liberal fluid strategy. Safety was also assessed.
Results:
A total of 1563 patients were enrolled, with 782 assigned to the restrictive fluid group and 781 to the liberal fluid group. Resuscitation therapies that were administered during the 24-hour protocol period differed between the two groups; less intravenous fluid was administered in the restrictive fluid group than in the liberal fluid group (difference of medians, -2134 ml; 95% confidence interval [CI], -2318 to -1949), whereas the restrictive fluid group had earlier, more prevalent, and longer duration of vasopressor use. Death from any cause before discharge home by day 90 occurred in 109 patients (14.0%) in the restrictive fluid group and in 116 patients (14.9%) in the liberal fluid group (estimated difference, -0.9 percentage points; 95% CI, -4.4 to 2.6; P=0.61); 5 patients in the restrictive fluid group and 4 patients in the liberal fluid group had their data censored (lost to follow-up). The number of reported serious adverse events was similar in the two groups.
Conclusions:
Among patients with sepsis-induced hypotension, the restrictive fluid strategy that was used in this trial did not result in significantly lower (or higher) mortality before discharge home by day 90 than the liberal fluid strategy.
(4). Gaofeng Yi, et al., Colocolonic Intussusception. N Engl J Med. 2023;388:263.
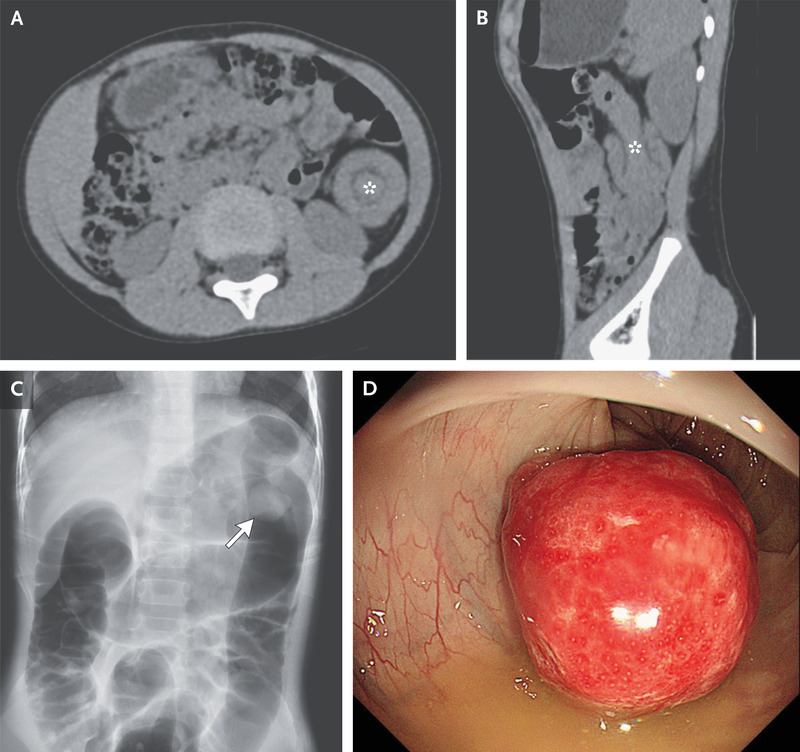
A 5-year-old boy presented with a 2-day history of intermittent abdominal pain and mucus-covered stool. CT of the abdomen revealed a target sign and telescoping in the descending colon.
(5). Major Extremity Trauma Research Consortium (METRC). Aspirin or Low-Molecular-Weight Heparin for Thromboprophylaxis after a Fracture. N Engl J Med. 2023;388:203-213. Abstract Background:
Clinical guidelines recommend low-molecular-weight heparin for thromboprophylaxis in patients with fractures, but trials of its effectiveness as compared with aspirin are lacking.
Methods:
In this pragmatic, multicenter, randomized, noninferiority trial, we enrolled patients 18 years of age or older who had a fracture of an extremity (anywhere from hip to midfoot or shoulder to wrist) that had been treated operatively or who had any pelvic or acetabular fracture. Patients were randomly assigned to receive low-molecular-weight heparin (enoxaparin) at a dose of 30 mg twice daily or aspirin at a dose of 81 mg twice daily while they were in the hospital. After hospital discharge, the patients continued to receive thromboprophylaxis according to the clinical protocols of each hospital. The primary outcome was death from any cause at 90 days. Secondary outcomes were nonfatal pulmonary embolism, deep-vein thrombosis, and bleeding complications.
Results:
A total of 12,211 patients were randomly assigned to receive aspirin (6101 patients) or low-molecular-weight heparin (6110 patients). Patients had a mean (±SD) age of 44.6±17.8 years, 0.7% had a history of venous thromboembolism, and 2.5% had a history of cancer. Patients received a mean of 8.8±10.6 in-hospital thromboprophylaxis doses and were prescribed a median 21-day supply of thromboprophylaxis at discharge. Death occurred in 47 patients (0.78%) in the aspirin group and in 45 patients (0.73%) in the low-molecular-weight-heparin group (difference, 0.05 percentage points; 96.2% confidence interval, -0.27 to 0.38; P<0.001 for a noninferiority margin of 0.75 percentage points). Deep-vein thrombosis occurred in 2.51% of patients in the aspirin group and 1.71% in the low-molecular-weight-heparin group (difference, 0.80 percentage points; 95% CI, 0.28 to 1.31). The incidence of pulmonary embolism (1.49% in each group), bleeding complications, and other serious adverse events were similar in the two groups.
Conclusions:
In patients with extremity fractures that had been treated operatively or with any pelvic or acetabular fracture, thromboprophylaxis with aspirin was noninferior to low-molecular-weight heparin in preventing death and was associated with low incidences of deep-vein thrombosis and pulmonary embolism and low 90-day mortality.
(6). Jonathan KY, et al. Assessment of photopsia (flashing lights). BMJ 2023;380:e064767.
What you need to know
If photopsia is monocular, consider an ocular cause; for simultaneous bilateral photopsia, consider neurological or systemic causes
Posterior vitreous detachment (manifesting as monocular temporal flashes) is the most common cause of photopsia, and may lead to sight threatening retinal tears and detachment
Consider specialist assessment within 24 hours for all suspected ocular causes of acute photopsia
(7). Kirsten E Lyke, et al. Low-dose intravenous and subcutaneous CIS43LS monoclonal antibody for protection against malaria (VRC 612 Part C): a phase 1, adaptive trial. Lancet Infect Dis. 2023. Abstract Background:
Human monoclonal antibodies might offer an important new approach to reduce malaria morbidity and mortality. In the first two parts of a three-part clinical trial, the antimalarial monoclonal antibody CIS43LS conferred high protection against parasitaemia at doses of 20 mg/kg or 40 mg/kg administered intravenously followed by controlled human malaria infection. The ability of CIS43LS to confer protection at lower doses or by the subcutaneous route is unknown. We aimed to provide data on the safety and optimisation of dose and route for the human antimalaria monoclonal antibody CIS43LS.
Methods:
VRC 612 Part C was the third part of a three-part, first-in-human, phase 1, adaptive trial, conducted at the University of Maryland, Baltimore Center for Vaccine Development and Global Health, Baltimore, MD, USA. We enrolled adults aged 18-50 years with no previous malaria vaccinations or infections, in a sequential, dose-escalating manner. Eligible participants received the monoclonal antibody CIS43LS in a single, open-label dose of 1 mg/kg, 5 mg/kg, or 10 mg/kg intravenously, or 5 mg/kg or 10 mg/kg subcutaneously. Participants underwent controlled human malaria infection by the bites of five mosquitoes infected with Plasmodium falciparum 3D7 strain approximately 8 weeks after their monoclonal antibody inoculation. Six additional control participants who did not receive CIS43LS underwent controlled human malaria infection simultaneously. Participants were followed-up daily on days 7-18 and day 21, with qualitative PCR used for P falciparum detection. Participants who tested positive for P falciparum were treated with atovaquone-proguanil and those who remained negative were treated at day 21. Participants were followed-up until 24 weeks after dosing. The primary outcome was safety and tolerability of CIS43LS at each dose level, assessed in the as-treated population. Secondary outcomes included protective efficacy of CIS43LS after controlled human malaria infection. This trial is now complete and is registered with ClinicalTrials.gov, NCT04206332.
Findings:
Between Sept 1, 2021, and Oct 29, 2021, 47 people were assessed for eligibility and 31 were enrolled (one subsequently withdrew and was replaced) and assigned to receive doses of 1 mg/kg (n=7), 5 mg/kg (n=4), and 10 mg/kg (n=3) intravenously and 5 mg/kg (n=4) and 10 mg/kg (n=4) subcutaneously, or to the control group (n=8). CIS43LS administration was safe and well tolerated; no serious adverse events occurred. CIS43LS protected 18 (82%) of 22 participants who received a dose. No participants developed parasitaemia following dosing at 5 mg/kg intravenously or subcutaneously, or at 10 mg/kg intravenously or subcutaneously. All six control participants and four of seven participants dosed at 1 mg/kg intravenously developed parasitaemia after controlled human malaria infection.
Interpretation:
CIS43LS was safe and well tolerated, and conferred protection against P falciparum at low doses and by the subcutaneous route, providing evidence that this approach might be useful to prevent malaria across several clinical use cases.
Funding:
National Institute of Allergy and Infectious Diseases, National Institutes of Health.
(8). Daren K Heyland, et al. The effect of higher protein dosing in critically ill patients with high nutritional risk (EFFORT Protein): an international, multicentre, pragmatic, registry-based randomised trial. 2023. Summary Background:
On the basis of low-quality evidence, international critical care nutrition guidelines recommend a wide range of protein doses. The effect of delivering high-dose protein during critical illness is unknown. We aimed to test the hypothesis that a higher dose of protein provided to critically ill patients would improve their clinical outcomes.
Methods:
This international, investigator-initiated, pragmatic, registry-based, single-blinded, randomised trial was undertaken in 85 intensive care units (ICUs) across 16 countries. We enrolled nutritionally high-risk adults (≥18 years) undergoing mechanical ventilation to compare prescribing high-dose protein (≥2·2 g/kg per day) with usual dose protein (≤1·2 g/kg per day) started within 96 h of ICU admission and continued for up to 28 days or death or transition to oral feeding. Participants were randomly allocated (1:1) to high-dose protein or usual dose protein, stratified by site. As site personnel were involved in both prescribing and delivering protein dose, it was not possible to blind clinicians, but patients were not made aware of the treatment assignment. The primary efficacy outcome was time-to-discharge-alive from hospital up to 60 days after ICU admission and the secondary outcome was 60-day morality. Patients were analysed in the group to which they were randomly assigned regardless of study compliance, although patients who dropped out of the study before receiving the study intervention were excluded. This study is registered with ClinicalTrials.gov, NCT03160547.
Findings:
Between Jan 17, 2018, and Dec 3, 2021, 1329 patients were randomised and 1301 (97·9%) were included in the analysis (645 in the high-dose protein group and 656 in usual dose group). By 60 days after randomisation, the cumulative incidence of alive hospital discharge was 46·1% (95 CI 42·0%-50·1%) in the high-dose compared with 50·2% (46·0%-54·3%) in the usual dose protein group (hazard ratio 0·91, 95% CI 0·77-1·07; p=0·27). The 60-day mortality rate was 34·6% (222 of 642) in the high dose protein group compared with 32·1% (208 of 648) in the usual dose protein group (relative risk 1·08, 95% CI 0·92-1·26). There appeared to be a subgroup effect with higher protein provision being particularly harmful in patients with acute kidney injury and higher organ failure scores at baseline.
Interpretation:
Delivery of higher doses of protein to mechanically ventilated critically ill patients did not improve the time-to-discharge-alive from hospital and might have worsened outcomes for patients with acute kidney injury and high organ failure scores.
(9). Giovanni E Ferreira, et al., Efficacy, safety, and tolerability of antidepressants for pain in adults. BMJ 2023;380:e072415 Abstract Objective:
To provide a comprehensive overview of the efficacy, safety, and tolerability of antidepressants for pain according to condition. Design Overview of systematic reviews.Data sources PubMed, Embase, PsycINFO, and the Cochrane Central Register of Controlled Trials from inception to 20 June 2022.Eligibility criteria for selecting studies Systematic reviews comparing any antidepressant with placebo for any pain condition in adults.Data extraction and synthesis Two reviewers independently extracted data. The main outcome measure was pain; for headache disorders it was frequency of headaches. Continuous pain outcomes were converted into a scale of 0 (no pain) to 100 (worst pain) and were presented as mean differences (95% confidence intervals). Dichotomous outcomes were presented as risk ratios (95% confidence intervals). Data were extracted from the time point closest to the end of treatment. When end of treatment was too variable across trials in a review, data were extracted from the outcome or time point with the largest number of trials and participants. Secondary outcomes were safety and tolerability (withdrawals because of adverse events). Findings were classified from each comparison as efficacious, not efficacious, or inconclusive. Certainty of evidence was assessed with the grading of recommendations assessment, development, and evaluation framework.Results 26 reviews (156 unique trials and >25 000 participants) were included. These reviews reported on the efficacy of eight antidepressant classes covering 22 pain conditions (42 distinct comparisons). No review provided high certainty evidence on the efficacy of antidepressants for pain for any condition. 11 comparisons (nine conditions) were found where antidepressants were efficacious, four with moderate certainty evidence: serotonin-norepinephrine reuptake inhibitors (SNRIs) for back pain (mean difference -5.3, 95% confidence interval -7.3 to -3.3), postoperative pain (-7.3, -12.9 to -1.7), neuropathic pain (-6.8, -8.7 to -4.8), and fibromyalgia (risk ratio 1.4, 95% confidence interval 1.3 to 1.6). For the other 31 comparisons, antidepressants were either not efficacious (five comparisons) or the evidence was inconclusive (26 comparisons).Conclusions Evidence of efficacy of antidepressants was found in 11 of the 42 comparisons included in this overview of systematic reviews-seven of the 11 comparisons investigated the efficacy of SNRIs. For the other 31 comparisons, antidepressants were either inefficacious or evidence on efficacy was inconclusive. The findings suggest that a more nuanced approach is needed when prescribing antidepressants for pain conditions.
(10). Casey Crump, et al. Adverse pregnancy outcomes and long term risk of ischemic heart disease in mothers: national cohort and co-sibling study. BMJ 2023;380:e072112 Abstract Objective:
To examine the associations between five major adverse pregnancy outcomes and long term risks of ischemic heart disease in mothers.
Design:
National cohort study.
Setting:
Sweden.
Participants:
All 2 195 266 women with a first singleton delivery in Sweden during 1973-2015.
Main outcome measures
: The main outcome measure was incidence of ischemic heart disease from delivery to 2018, identified from nationwide inpatient and outpatient diagnoses. Cox regression was used to calculate hazard ratios for ischemic heart disease associated with preterm delivery, small for gestational age, pre-eclampsia, other hypertensive disorders of pregnancy, and gestational diabetes, adjusting for other adverse pregnancy outcomes and maternal factors. Co-sibling analyses assessed for confounding by shared familial (genetic and environmental) factors.
Results:
During 53.6 million person years of follow-up, ischemic heart disease was diagnosed in 83 881 (3.8%) women. All five adverse pregnancy outcomes were independently associated with increased risk of ischemic heart disease. In the 10 years after delivery, adjusted hazard ratios for ischemic heart disease associated with specific adverse pregnancy outcomes were 2.09 (95% confidence interval 1.77 to 2.46) for other hypertensive disorders of pregnancy, 1.72 (1.55 to 1.90) for preterm delivery, 1.54 (1.37 to 1.72) for pre-eclampsia, 1.30 (1.09 to 1.56) for gestational diabetes, and 1.10 (1.00 to 1.21) for small for gestational age. The hazard ratios remained significantly increased even 30-46 years after delivery: 1.47 (1.30 to 1.66) for other hypertensive disorders of pregnancy, 1.40 (1.29 to 1.51) for gestational diabetes, 1.32 (1.28 to 1.36) for pre-eclampsia, 1.23 (1.19 to 1.27) for preterm delivery, and 1.16 (1.13 to 1.19) for small for gestational age. These findings were only partially (<45%) explained by shared familial (genetic or environmental) factors. Women who experienced multiple adverse pregnancy outcomes showed further increases in risk (eg, <10 years after delivery, adjusted hazard ratios associated with 1, 2, or ≥3 adverse pregnancy outcomes were 1.29 (1.19 to 1.39), 1.80 (1.59 to 2.03), and 2.26 (1.89 to 2.70), respectively)).
Conclusions
: In this large national cohort, women who experienced any of five major adverse pregnancy outcomes showed an increased risk for ischemic heart disease up to 46 years after delivery. Women with adverse pregnancy outcomes should be considered for early preventive evaluation and long term risk reduction to help prevent the development of ischemic heart disease.
(11). Kathy Oxtoby. Helping patients get their lives back: the colorectal surgeon. BMJ 2023;380:p94
At the age of 6 Tayo Oke decided she wanted to become a surgeon-to satisfy her curiosity about what really happens in an operating theatre. “Whenever I’d see one of the Doctor in the House films and there was an operation, I’d always wonder what was happening to the person under the surgical drape. I wanted to know what the doctor was actually doing. And I was curious about what human insides looked like,” she recalls.
That curiosity drove her towards a career in colorectal surgery-a specialty she describes as “my natural home.”
“During my training I considered all the surgical subspecialties, but colorectal surgery was where I felt I could make the most difference-for example, doing colon cancer surgery,” says Oke, a consultant general and colorectal surgeon at Queen Elizabeth Hospital, Woolwich, part of Lewisham and Greenwich NHS Trust.
Oke enjoys the anatomical aspects of surgery- “putting bits of bowel together.” And she also appreciates how the specialty allows her to operate alongside other surgical colleagues, such as gynaecologists or urologists.
She finds the “strong bond” that she develops with patients extremely rewarding. “When someone is really unwell their life comes to a standstill. Some patients have been carrying their ailments with them a long time, and have been unable really to talk about them. So you need to build trust. It’s an absolute privilege to be entrusted with the welfare of another human being, and to be part of a team that will hopefully get a patient back to full health again.”
That bond with patients “is unique, and it stays with you forever,” she says. “During the pandemic, I received phone calls from concerned former patients wanting to know I was okay. Patients send me thank you cards. All of this spurs you on and encourages you,” she says.
Born in London, Oke trained at University College Hospital, Ibadan, Nigeria, where her family was originally from. She returned to the UK in 1989, passed her Professional and Linguistic Assessments Board test and did various surgical senior house officer jobs. During her training she worked for some inspiring female surgeons. “Consultant surgeon Anne Davis was my first mentor and role model. She encouraged me and saw me through dark days when life was difficult. I learnt a lot from her.”
Jean McDonald “was the first black female surgeon I’d ever met, and she had a massive impact on me,” says Oke. “She kept me going, told me to believe in myself, and said as long as I did the work and knew what I was doing, I would eventually get to where I wanted to be in my career.”
During her higher surgical training, Oke was also inspired by colorectal surgeon Christine Hall. “She was a teacher who took an interest in your welfare and gave you courage.”
Since being appointed to her first-and current-consultant role in 2001, she has tried to give that same level of support and encouragement to trainees. “I aim to create a pleasant environment for trainees to learn in, and to become competent surgeons. It’s important to be empathetic and sympathetic, to talk through any problems, and to give your full support.”
As for Oke’s career ambitions, she intends to stay on the “front line” of healthcare, rather than diversifying into other clinical or management roles, preferring to “take on complex cases.”
“It’s a wonderful feeling when I’ve been able to help these patients get their life back,” she says.
Outside of work she winds down by taking long walks while listening to music. “I get lost in my own world. My music taste is eclectic, from classical and gospel, to hip hop and smooth jazz.”
But she has no intention of winding down her career, or moving away from her love of surgery. “The beauty of colorectal surgery is that no two abdomens are the same. I’m still blindsided by some of the cases I come across. My curiosity about what’s under the surgical drapes may be satisfied. But life is still full of surprises.”
Nominated by Sala Abdalla
“I first met Ms Oke in 2015 when I worked at the trust as trainee colorectal registrar. I had chosen to work for her as she has a reputation for being an excellent trainer. My time with her was so rewarding that some years later I returned to do a second stint with her firm.
“I have been inspired by Tayo, not least because of her exceptional skills and expertise as a surgeon, but because she has taught me something extremely valuable-which is to care about patients, not to just care for them.
“In working for Tayo I have learnt that investing extra time in getting to know patients beyond their disease process enhances their experience and can improve clinical outcomes.
“I am indebted to Tayo Oke for the training, time, and dedication she has given me, and for the way she has made me feel while working with her-respected and valued.”
Sala Abdalla is a consultant general and upper gastrointestinal surgeon, Ealing Hospital, London North West University Healthcare NHS Trust.
(12). Helen Salisbury. The urgent and the important. BMJ 2023;380:p209
In a gentler age, when few patients had cars and many didn’t have telephones, my predecessors in the practice did routine visits every month or so to check up on their most vulnerable housebound patients. There were few guidelines to follow or boxes to tick, and general practices were paid according to the number of patients they looked after, with an allowance for the number of partners involved.
Now I find myself wondering if we may have lost something important. Much of our current work consists of responding to urgent demand: the queue may be physical, on the phone, or in the online triage inbox, but there are always people waiting for our attention. And when we’ve finished with the queue we must turn our focus towards the business, making sure that we’ve ticked the boxes in the quality metrics to gain points-and points mean prizes (or, at least, enough money to pay the staff and the bills). We need to make sure that our practice protocols are up to date, just in case the Care Quality Commission comes calling and wants to see evidence that we’ve all done our Prevent training.
If we weren’t so taken up with the urgent, and the externally imposed “necessary,” what important things might we do instead? We recently looked at our list of housebound patients to see how many haven’t been visited by a GP in the past year. They may have seen a paramedic for an acute illness, or a district nurse bringing a flu vaccination, but this doesn’t replace a conversation in person with your own doctor.
These visits are my opportunity not only to check blood pressure and review medications-which arguably could be done by other members of the team-but to update my knowledge of my patients. How quickly do they move? How sharp or clouded is their vision, hearing, and intellect? I like to have a mental image of each of my elderly patients so that, when they do become unwell, I know what their normal is. This informs conversations and decisions made with their families and other health professionals. Our practice’s brief audit has revealed that some of our patients have missed out in the past year, and we plan to make sure that they’re all offered a visit by their named doctor in the near future.
Does it matter to patients? Perhaps not to all, but I think many of them do value having a doctor they know and who knows them. It’s much easier to ask for help from someone you’ve already met, and to trust that they’ll respond. And not everyone has this feeling of safety-the reassurance that someone is looking after them.
Maybe it’s time to re-examine our priorities: should I really be poring over spreadsheets of targets and results, retrospectively adding exception codes? Or would that time be more usefully spent caring for my patients?
(13). Richard Smith. “Functional disorders”: one of medicine’s biggest failures. BMJ 2023;380:p221.
About a third of patients attending neurological and gastrointestinal, or almost every outpatient clinic-have functional disorders, meaning that they do not have a physical cause that can be detected with a microscope, scanners, or blood or genetic tests. These are patients whom medicine has failed more than almost any other group.
I’ve been reading Suzanne O’Sullivan’s The Sleeping Beauties: And Other Stories of Mystery Illness, a book that was recommended by a doctor colleague because it had had a big impact on him. It’s now had a big impact on me and probably will on you if you read it. O’Sullivan is a Queen Square neurologist who specialises in functional disorders and a gifted writer who is acutely aware of the limitations of her medical craft. Her book tells the stories of outbreaks of mass psychogenic illness, including the young asylum seekers in Sweden who have been “asleep” for years, the American diplomats in Havana and Beijing suffering symptoms attributed to a sonic bomb weapon, and several others. The stories make excellent reading, but the value of the book to doctors is that it can benefit their practice and deepen their understanding of medicine.
Language, as always, is part of the problem. Functional disorder is perhaps the best term for these conditions, but psychosomatic, psychogenic, conversion disorder, and in the past hysteria have all been used. Hysteria, with its association with women, is clearly unacceptable, and the prefix “psycho” is unhelpful. As O’Sullivan writes “Every medical problem is a combination of the biological, the psychological, and the social. It is only the weighting of each that changes.” Medicine was cursed when René Descartes divided the mind from the body.
Almost any symptom, perhaps every symptom, can result from functional disorder. O’Sullivan lists paralysis, blindness, headache, dizziness, coma, tremor, skin rashes, breathlessness, chest pain, palpitations, bladder problems, diarrhoea, stomach cramps, and so on and on. I might add fatigue, abdominal pain, diarrhoea, cough, backache, pain in any part of the body, and a gamut of symptoms that have no known physical cause.
We are all aware that mental activity or emotion can cause bodily symptoms like tears and blushing, but most of us find it hard to accept that mental activity could cause something as extreme as a coma, fits, or blindness. If no physical cause can be found then people are tempted to think that the symptoms are “not real,” “all in the mind,” or that the patient is faking them. These are serious mistakes to make: the symptoms are as “real” as with any physical cause and just as severe; they are not “all in the mind” because the body is clearly affected and the division between mind and body is not helpful; and there is no fakery. It’s also a mistake, writes O’Sullivan, to attribute them to “stress.”
Our understanding of how people develop these symptoms is poor, but the starting point is distress of some kind. “Embodied cognition” is the theory that sensory and motor systems are integrated with cognitive processing. As O’Sullivan writes: “The body is awash with white noise, so symptoms can always be found if a person looks hard enough.” “Looking hard,” implies a conscious action, which is probably not what she intended. Those symptoms are then linked with illnesses, even diseases, we know about. “Illness is a socially patterned behaviour, far more than people realise,” writes O’Sullivan, “How a person interprets and reacts to bodily changes depends on trends within society, their knowledge, their education, their access to information and their past experience of disease.” Modern medicine offers an increasing range of diseases for people to unconsciously connect with.
The philosopher Ian Hacking has described a phenomenon he calls “Making up people.” New classifications “bring into being a new kind of person” who have the classification attached to them or attach it to themselves. Their symptoms may then be added to the new classification, changing, and expanding it. “The classification changes the person, who in turn changes the features of the classification,” which has been called “the looping effect.”
Past experiences can be important in developing functional disorders. O’Sullivan uses the example of patients who have lost their voices after a severe bout of laryngitis. The next time the patients develop sore throats, perhaps milder ones, the prior experience may lead to the patients losing their voices again. “The top-down priors overwhelm the sensory input.”
Our understanding is, it seems to me, limited, and the theories and mechanisms that O’Sullivan discusses are unfamiliar to most doctors.
Just as culture dictates how we try to make sense of symptoms it also dictates how we respond. Our usual response is to see a doctor, and the doctors feel obliged to exclude physical disease. The patient undergoes a barrage of tests, and some of those tests may suggest something wrong both because of false positives and because “normal” is often defined as being within two standard deviations of the mean, which means 5% of results will be “abnormal” by mathematical definition. Patients are understandably made anxious by tests that suggest that something may be wrong, and more tests are needed to exclude disease, giving further opportunities for misleading results. Many patients will conclude that “Something must be seriously wrong if the doctors are doing all these tests.”
The patients may then begin the merry-go-round of specialists. Only the crass will say “there is nothing wrong with you” because the patient clearly has something wrong. Indeed, after all the tests and anxiety he or she may be feeling worse. When no physical cause is found the patients may be referred to psychiatrists, with at least the implication that the patients have a psychological problem. Because of the stigma unjustly attached to psychological problems this can cause distress and offence and is anyway to fall into the trap of thinking the physical and psychological separate.
O’Sullivan worries about this: “Like many Western doctors, I medicalise feelings and behaviour. People come to me so that I will do that for them-give them a medical explanation for their suffering-but, in truth, I worry all the time that what I’m doing, faithful as it is to my training and welcome as it may be to my patients, is wrong and potentially harmful.”
O’Sullivan finds herself attracted to some of the conditions that western medicine calls mass psychogenic illness. Grisi siknis occurs only among the Miskito, an indigenous people from the coast of Nicaragua and Honduras. The sickness begins with mild symptoms but progresses to irrational behaviour, convulsions, and hallucinations. Patients, who are mostly young and female, see a dark figure that they know to be the devil.
The condition does not attract blame but rather community support, and it usually passes. O’Sullivan writes: “I found a great deal in grisi siknis that I could admire. It can be a very effective culturally agreed means of expressing distress. It is an acceptable way to exteriorize and deal with personal and social conflict. It is also a useful one, because it comes without blame. The demon infiltrator presents an external cause that removes the focus from the individual. It also provides something at which to aim treatment.”
She draws a contrast with people with functional disorders exposed to modern medicine. Not only must they undergo many tests and pick up “diagnoses” along the way but they may also become permanent patients. Worse still, the patients may find themselves in battles with the medical establishment.
People recover from functional disorders, but treatment is difficult. Doctors and patients in conflict is the worst outcome for everybody. O’Sullivan concludes her book by emphasising the role of community: “I also learned that the best chance of recovery comes when you surround yourself with a community that allows patients and their doctors to find that common ground. A community that can listen without judgement. A community that provides support. A community that can tolerate imperfection and failure, and which has the humility to put aside its vested interests. A community that is able to take a holistic view of health.”
(13). Mason W. Freeman. Phase 2 Trial of Baxdrostat for Treatment-Resistant Hypertension. N Engl J Med. 2023;388:395-405. Abstract Background:
Aldosterone synthase controls the synthesis of aldosterone and has been a pharmacologic target for the treatment of hypertension for several decades. Selective inhibition of aldosterone synthase is essential but difficult to achieve because cortisol synthesis is catalyzed by another enzyme that shares 93% sequence similarity with aldosterone synthase. In preclinical and phase 1 studies, baxdrostat had 100:1 selectivity for enzyme inhibition, and baxdrostat at several dose levels reduced plasma aldosterone levels but not cortisol levels.
Methods:
In this multicenter, placebo-controlled trial, we randomly assigned patients who had treatment-resistant hypertension, with blood pressure of 130/80 mm Hg or higher, and who were receiving stable doses of at least three antihypertensive agents, including a diuretic, to receive baxdrostat (0.5 mg, 1 mg, or 2 mg) once daily for 12 weeks or placebo. The primary end point was the change in systolic blood pressure from baseline to week 12 in each baxdrostat group as compared with the placebo group.
Results:
A total of 248 patients completed the trial. Dose-dependent changes in systolic blood pressure of -20.3 mm Hg, -17.5 mm Hg, -12.1 mm Hg, and -9.4 mm Hg were observed in the 2-mg, 1-mg, 0.5-mg, and placebo groups, respectively. The difference in the change in systolic blood pressure between the 2-mg group and the placebo group was -11.0 mm Hg (95% confidence interval [CI], -16.4 to -5.5; P<0.001), and the difference in this change between the 1-mg group and the placebo group was -8.1 mm Hg (95% CI, -13.5 to -2.8; P=0.003). No deaths occurred during the trial, no serious adverse events were attributed by the investigators to baxdrostat, and there were no instances of adrenocortical insufficiency. Baxdrostat-related increases in the potassium level to 6.0 mmol per liter or greater occurred in 2 patients, but these increases did not recur after withdrawal and reinitiation of the drug.
Conclusions:
Patients with treatment-resistant hypertension who received baxdrostat had dose-related reductions in blood pressure.
(14). Paolo Spriano. Managing Uncertainty in the Practice of Medicine. 2023
Medicine is a highly complex profession. Physicians are called upon to provide diagnoses, to come up with treatment plans, and to give prognoses about the disease course and outcomes of their patients. In clinical practice, they often encounter cases in which a patient presents with symptoms that are common to various conditions. To establish the actual cause, the physician must perform a differential diagnosis. This process involves gathering the individual’s medical history, carrying out a targeted exam, and ordering any additional tests that are necessary. Is it any wonder, then, that uncertainty should be a daily presence in physicians’ lives?
Decision analysis in medicine shows that there is a high level of uncertainty when the best decision that the physician may make is not immediately clear (that is, when many solutions are perceived as good) and when the problem is one that occurs infrequently or that requires a high degree of knowledge.
Having strategies to deal with uncertainty could be helpful, according to an editorial published in The American Journal of Medicine. The author, Daniel M. Lichtstein, MD, mentions aspects of daily clinical practice to which these strategies can be applied.
Acknowledge Uncertainty
Physicians are responsible for striving to do the best they can for their patients at all times, yet diagnostic dilemmas are common, and the preferred evaluation and treatment are not always clear. The most important step for physicians to take when dealing with uncertainty is to acknowledge it.
All physicians make errors. Some of these errors can be traced to not acknowledging uncertainty and to not having the humility or willingness to admit when they do not know something. Being humble enough to say, “I don’t know,” and to recognize when consultation with colleagues or consultants is indicated is critically important and is something that patients deserve.
Clinical Practice Strategies
Sharing uncertainty and taking a patient-centered approach to decision-making help to create open and trusting relationships with patients. Lichtstein writes, “I realized that by initially not sharing my uncertainty with my patients, it resulted in more stress and worry.”
Patients should always be instructed to call if their condition changes or worsens, and physicians should be specific about what the patient should look for and how to get in touch.
In addition, close follow-up is crucial in dealing with uncertainty. The correct diagnosis may become apparent as an illness evolves, and close follow-up increases the likelihood that a physician may recognize it.
If a patient is being discharged from the hospital and another physician (likely the patient’s primary care physician) is going to assume follow-up, that physician should be contacted directly, and any uncertainty regarding the patient’s condition or plans of care moving forward should be made clear. The same principle applies during a hospitalization as care is transitioned from one shift to another or from one physician to another.
When uncertain about the course a condition may take or how the patient may respond to treatment, a physician may feel that he or she is letting the patient down or is disappointing them in some way. But as Katrina Armstrong, MD, wrote in her article, “If You Can’t Beat It, Join It: Uncertainty and Trust in Medicine,” “The greatest comfort to a patient can be hearing that, regardless of clinical uncertainty, their physician will be with them no matter what the future brings.”
(15). Clare Thakker, et al. Investigating eosinophilia. BMJ 2023;380:e070295 What you need to know
Eosinophilia can indicate one or more underlying diseases
Common causes are allergy, atopy, asthma, drug hypersensitivity, and helminth infection
If eosinophilia persists with no identified reactive cause, consider haematology assessment for investigation of primary eosinophilia
Eosinophilia with evidence of end organ damage warrants urgent secondary care assessment
(16). Avner Reshef, et al., New medications to mitigate attacks of hereditary angioedema: does one size fit all? Lancet 2023;401(10375):413-415.
Hereditary angioedema has received renewed attention in the past two decades, with the elucidation of the biochemical pathways resulting in bradykinin overproduction in patients with congenital C1esterase inhibitor (C1INH) deficiency, leading to recurrent attacks of tissue swelling due to uncontrolled vascular permeability. 1 Oedema attacks affecting the lingual or laryngeal area can become lethal as a result of asphyxiation. 2 Several new treatments have emerged, 143 years after Quincke’s first description of hereditary angioedema and 15 years after the introduction of the first specific bradykinin B2 receptor inhibitor (icatibant). These drugs specifically target crucial steps in the kallikrein-kinin (contact) cascade downstream of bradykinin production. 3 Many of these agents have shown their efficacy and safety in acute (on-demand) treatment and prophylaxis of hereditary angioedema attacks, saving lives and revolutionising patients’ quality of life. 4 These modalities fit well into the modern paradigm in hereditary angioedema treatment, supporting patients’ autonomy, recommending self-administration, and reducing reliance on hospital emergency rooms, health-care providers, and medical points of care.
(17). Carmen Amado et al., Tuberculous Optochiasmatic Arachnoiditis. 2023.
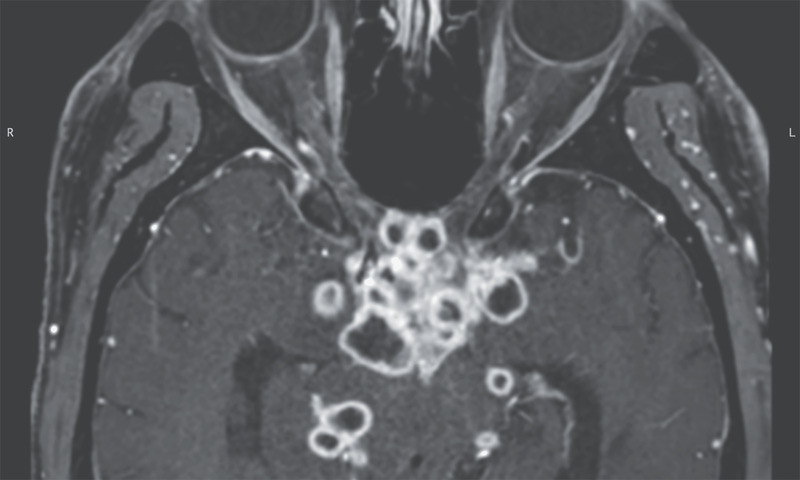
A 29-year-old man presented to the emergency department with a 1-week history of headache and blurry vision. Six weeks earlier, he had received a diagnosis of gastrointestinal tuberculosis and had begun antituberculosis therapy. Physical examination was notable for nuchal rigidity, papilledema, and a relative afferent pupillary defect on the right side. Ophthalmologic evaluation revealed visual acuity of 20/200 in the left eye and only light perception in the right eye. Magnetic resonance imaging of the head revealed multiple ringlike enhancing lesions near the optic chiasm, optic tracts, and perimesencephalic and suprasellar cisterns (see image). Cerebrospinal fluid analysis showed lymphocytic pleocytosis, and nucleic acid amplification testing identified Mycobacterium tuberculosis. A diagnosis of tuberculous optochiasmatic arachnoiditis was made. Tuberculous optochiasmatic arachnoiditis is a complication of tuberculous meningitis in which exudates cause inflammation of the arachnoid of the optic nerve and chiasm, which can result in vision loss. In this patient, the development of this condition was thought to be a paradoxical reaction to antituberculosis therapy that resulted in the development of new lesions. Treatment with dexamethasone was initiated, and the antituberculosis therapy was continued. At a 3-month follow-up visit, the patient’s symptoms had abated.
(18). Alan T.N. Tita. Azithromycin to Prevent Sepsis or Death in Women Planning a Vaginal Birth. 2023 Abstract Background:
The use of azithromycin reduces maternal infection in women during planned cesarean delivery, but its effect on those with planned vaginal delivery is unknown. Data are needed on whether an intrapartum oral dose of azithromycin would reduce maternal and offspring sepsis or death.
Methods:
In this multicountry, placebo-controlled, randomized trial, we assigned women who were in labor at 28 weeks’ gestation or more and who were planning a vaginal delivery to receive a single 2-g oral dose of azithromycin or placebo. The two primary outcomes were a composite of maternal sepsis or death and a composite of stillbirth or neonatal death or sepsis. During an interim analysis, the data and safety monitoring committee recommended stopping the trial for maternal benefit.
Results:
A total of 29,278 women underwent randomization. The incidence of maternal sepsis or death was lower in the azithromycin group than in the placebo group (1.6% vs. 2.4%), with a relative risk of 0.67 (95% confidence interval [CI], 0.56 to 0.79; P<0.001), but the incidence of stillbirth or neonatal death or sepsis was similar (10.5% vs. 10.3%), with a relative risk of 1.02 (95% CI, 0.95 to 1.09; P=0.56). The difference in the maternal primary outcome appeared to be driven mainly by the incidence of sepsis (1.5% in the azithromycin group and 2.3% in the placebo group), with a relative risk of 0.65 (95% CI, 0.55 to 0.77); the incidence of death from any cause was 0.1% in the two groups (relative risk, 1.23; 95% CI, 0.51 to 2.97). Neonatal sepsis occurred in 9.8% and 9.6% of the infants, respectively (relative risk, 1.03; 95% CI, 0.96 to 1.10). The incidence of stillbirth was 0.4% in the two groups (relative risk, 1.06; 95% CI, 0.74 to 1.53); neonatal death within 4 weeks after birth occurred in 1.5% in both groups (relative risk, 1.03; 95% CI, 0.86 to 1.24). Azithromycin was not associated with a higher incidence in adverse events.
Conclusions:
Among women planning a vaginal delivery, a single oral dose of azithromycin resulted in a significantly lower risk of maternal sepsis or death than placebo but had little effect on newborn sepsis or death
(19). Natasha S, et al., Chagas Disease. Ann Intern Med. 2023. Abstract
Chagas disease, which is caused by infection with the parasite Trypanosoma cruzi, is a leading neglected tropical disease in the United States. An estimated 240 000 to 350 000 persons in the United States are infected, primarily immigrants from Mexico, Central America, and South America, where the disease is endemic. The parasite is transmitted by the triatomine bug but can also be passed through blood transfusion, via organ transplant, or congenitally. Approximately 30% of infected persons later develop cardiac and/or gastrointestinal complications. Health care providers should consider screening at-risk patients with serologic testing. Early diagnosis and treatment with benznidazole or nifurtimox can help prevent complications.
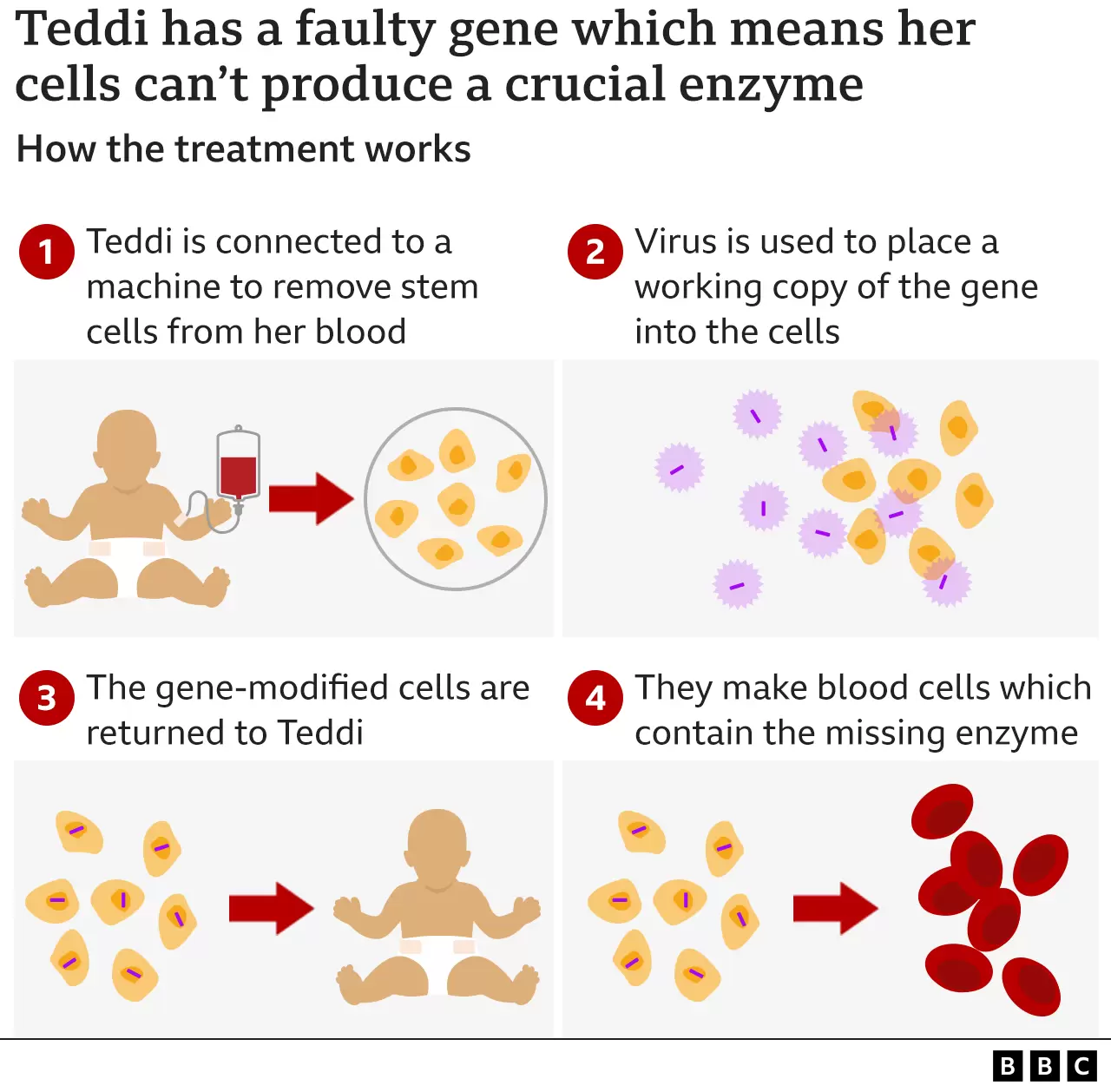
(20). MLD, Metachromatic Leuko Dystrophy
Three-year-old Nala – and Teddi, who is 19 months old – both have MLD, metachromatic leukodystrophy. Children with this fatal genetic disease are born apparently healthy, but MLD severely damages the brain and nervous system.gradually attacks the brain and body.
Teddi was diagnosed in time because her older sister Nala showed symptoms – but it was too late to treat Nala, who is now terminally ill.
The one-off treatment, called Libmeldy, costs £2.875m and is the most expensive medicine ever approved for the NHS.
MLD is caused by a faulty gene which means children affected cannot produce an important enzyme called ARSA – a protein that helps the body’s metabolism work.
As a result, fatty chemicals called sulfatides build up. These gradually destroy the protective layer around cells in the brain and nervous system, leading to a devastating deterioration. Children lose the ability to walk, talk or eat – and eventually to see or hear.
Libmeldy involves altering a patient’s own cells to correct the faulty gene. In June 2022, Teddi was hooked up to a machine at Royal Manchester Children’s Hospital where blood was removed and filtered, so a single bag of stem cells could be collected. The process looks similar to dialysis.
The cells were then sent to Milan, where scientists used a harmless virus to insert a working version of Teddi’s faulty gene – the one which should produce her missing enzyme – back into the stem cells. The gene-corrected stem cells were then sent to Manchester to be infused back into Teddi.
The infusion of Libmeldy took less than an hour. Over the following days the gene-altered cells migrated to Teddi’s bone marrow and began producing the enzyme she had been missing since birth.
What is remarkable is that this is a one-off treatment, with the hope that it provides a permanent fix for MLD.
Libmeldy was developed by a British company, Orchard Therapeutics. Its CEO and co-founder, Bobby Gaspar, spent many years as a consultant at Great Ormond Street Hospital, while carrying out research into potential therapies.
“Bringing a new medicine to the world that can potentially cure these devastating diseases is incredibly rewarding,” he says, adding that it was “a very long journey to develop a medicine like this”.
Libmeldy took nearly 20 years to develop, with the first human trials taking place in 2010. It got EU approval in December 2020 and is now available through the NHS.
(21). Martje M. Suverein et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N Engl J Med. 2023;388:299-309. Background
Extracorporeal cardiopulmonary resuscitation (CPR) restores perfusion and oxygenation in a patient who does not have spontaneous circulation. The evidence with regard to the effect of extracorporeal CPR on survival with a favorable neurologic outcome in refractory out-of-hospital cardiac arrest is inconclusive.
Methods
In this multicenter, randomized, controlled trial conducted in the Netherlands, we assigned patients with an out-of-hospital cardiac arrest to receive extracorporeal CPR or conventional CPR (standard advanced cardiac life support). Eligible patients were between 18 and 70 years of age, had received bystander CPR, had an initial ventricular arrhythmia, and did not have a return of spontaneous circulation within 15 minutes after CPR had been initiated. The primary outcome was survival with a favorable neurologic outcome, defined as a Cerebral Performance Category score of 1 or 2 (range, 1 to 5, with higher scores indicating more severe disability) at 30 days. Analyses were performed on an intention-to-treat basis.
Results
Of the 160 patients who underwent randomization, 70 were assigned to receive extracorporeal CPR and 64 to receive conventional CPR; 26 patients who did not meet the inclusion criteria at hospital admission were excluded. At 30 days, 14 patients (20%) in the extracorporeal-CPR group were alive with a favorable neurologic outcome, as compared with 10 patients (16%) in the conventional-CPR group (odds ratio, 1.4; 95% confidence interval, 0.5 to 3.5; P=0.52). The number of serious adverse events per patient was similar in the two groups.
Conclusions
In patients with refractory out-of-hospital cardiac arrest, extracorporeal CPR and conventional CPR had similar effects on survival with a favorable neurologic outcome
(22). Sarah E. Turecamo, et al. Association of Rurality With Risk of Heart Failure. JAMA Cardiol. 2023. Question:
Are rural populations at increased risk of heart failure?
Findings:
In this cohort study of Black and White adults, rural participants had an increased risk of heart failure compared with urban participants. The risk of heart failure associated with rurality was independent of cardiovascular risk factors and socioeconomic status and varied across race-sex groups, and Black men had the highest risk.
Meaning:
To address this association between rurality and higher risk of developing heart failure, particularly among Black men, interventions should focus on primary prevention of heart failure among these high-risk communities.
Importance:
Rural populations experience an increased burden of heart failure (HF) mortality compared with urban populations. Whether HF incidence is greater among rural individuals is less known. Additionally, the intersection between racial and rural health inequities is understudied.
Objective:
To determine whether rurality is associated with increased risk of HF, independent of cardiovascular (CV) disease and socioeconomic status (SES), and whether rurality-associated HF risk varies by race and sex.
Design, Setting, and Participants
: This prospective cohort study analyzed data for Black and White participants of the Southern Community Cohort Study (SCCS) without HF at enrollment who receive care via Centers for Medicare & Medicaid Services (CMS). The SCCS is a population-based cohort of low-income, underserved participants from 12 states across the southeastern United States. Participants were enrolled between 2002 and 2009 and followed up until December 31, 2016. Data were analyzed from October 2021 to November 2022.
Exposures
: Rurality as defined by Rural-Urban Commuting Area codes at the census-tract level.
Main Outcomes and Measures
: Heart failure was defined using diagnosis codes via CMS linkage through 2016. Incidence of HF was calculated by person-years of follow-up and age-standardized. Sequentially adjusted Cox proportional hazards regression models tested the association between rurality and incident HF.
Results:
Among 27 115 participants, the median (IQR) age was 54 years (47-65), 18 647 (68.8%) were Black, and 8468 (32.3%) were White; 5556 participants (20%) resided in rural areas. Over a median 13-year follow-up, age-adjusted HF incidence was 29.6 (95% CI, 28.9-30.5) per 1000 person-years for urban participants and 36.5 (95% CI, 34.9-38.3) per 1000 person-years for rural participants (P < .001). After adjustment for demographic information, CV risk factors, health behaviors, and SES, rural participants had a 19% greater risk of incident HF (hazard ratio [HR], 1.19; 95% CI, 1.13-1.26) compared with their urban counterparts. The rurality-associated risk of HF varied across race and sex and was greatest among Black men (HR, 1.34; 95% CI, 1.19-1.51), followed by White women (HR, 1.22; 95% CI, 1.07-1.39) and Black women (HR, 1.18; 95% CI, 1.08-1.28). Among White men, rurality was not associated with greater risk of incident HF (HR, 0.97; 95% CI, 0.81-1.16).
Conclusions and Relevance:
Among predominantly low-income individuals in the southeastern United States, rurality was associated with an increased risk of HF among women and Black men, which persisted after adjustment for CV risk factors and SES. This inequity points to a need for additional emphasis on primary prevention of HF among rural populations.
(23). Ruihai Zhou. A Paradoxical ST-Segment Elevation Distribution Rendering a Challenging Prediction of the Culprit Vessel in Acute Myocardial Infarction. JAMA Intern Med. 2023.
Case Presentation
A patient in their 50s, a current cigarette smoker with a history of hypertension but no known cardiac disease, presented with sudden-onset chest pain via emergency medical services (EMS). The patient was hypertensive with a systolic blood pressure of 220 mm Hg by EMS. On arrival at the emergency department, the patient was in acute distress due to ongoing chest pain. The patient was afebrile, heart rate was 72 bpm, respiration rate was 16 breaths per minute, and blood pressure was 153/97 mm Hg. The cardiopulmonary examination was overall unremarkable. The electrocardiograms (ECGs) obtained by EMS and in the emergency department showed ST-segment elevation (STE), up to 5 mm in amplitude, in leads V1 through V3 and horizontal/down sloping ST depression (STD) in leads V4 through V6. The diagnosis was STE myocardial infarction (STEMI). The patient was subsequently brought to the cardiac catheterization laboratory for emergency cardiac catheterization and coronary angiography as a code STEMI.
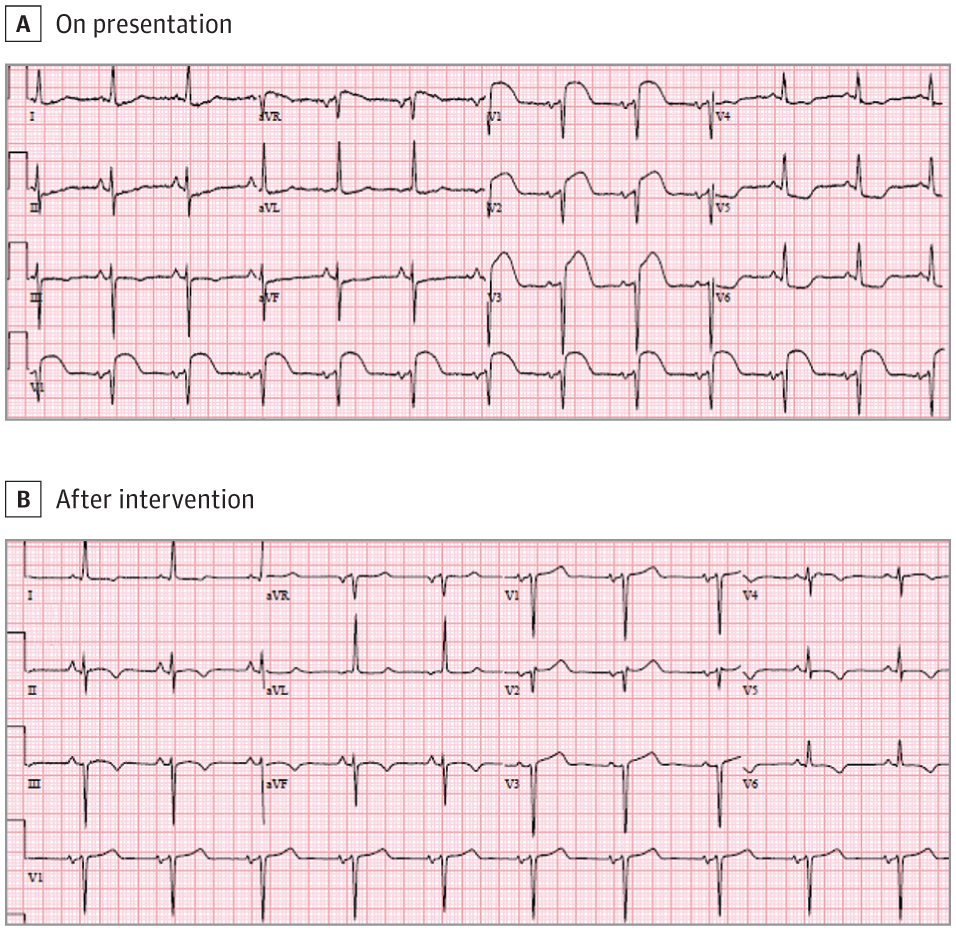
The ECG on presentation showed significant ST-segment elevation (STE) in leads V1 through V3 and ST-segment depression in leads V4 through V6 (A) consistent with STE myocardial infarction (STEMI). The STE resolved after successful primary percutaneous coronary intervention to total proximal occlusion of the nondominant right coronary artery as the culprit of STEMI (B).Questions: What is the most likely culprit vessel responsible for the STEMI? If the STEMI is due to an occluded right coronary artery (RCA), what do you expect to find in terms of the coronary anatomy?
Clinical Course
Coronary angiography showed total occlusion of the RCA from its proximal portion with Thrombolysis in Myocardial Infarction (TIMI) 0 flow (Figure, A). The patient underwent successful primary percutaneous coronary intervention (PCI) with a drug-eluting stent placement to the proximal RCA, resulting in restoration of TIMI 3 flow and no residual stenosis. The RCA was a nondominant vessel, and the left coronary arteries had no significant obstruction. The left circumflex artery (LCx) was dominant, supplying the lateral and inferior left ventricle (LV). The chest pain resolved after PCI. The post-PCI ECG showed resolution of the STE in leads V1 through V3 (Figure, B). The STD in V4 through V6 also recovered with development of shallow T-wave inversion. The echocardiography obtained the same day after PCI showed normal left and right ventricles in size and systolic function with no evident regional wall motion abnormality. The patient has been well since the primary PCI. The patient reported no symptoms at follow-ups.
Discussion
Findings from ECGs were first correlated with angiographic findings in patients presenting with STEMI by studies in the 1980s. In the setting of STEMI, the STE is present in the leads with positive electrodes overlying the infarcted region, and the STE distribution pattern can be used to predict the culprit vessel. The STE reflects an ischemia-induced injury current derived from the electrical voltage gradient at the boundary between the ischemic and normal myocardium.1
In the present case, the ECG showed dramatic STE in leads V1 through V3, which usually connotes anterior/anteroseptal infarction from proximal left anterior descending artery (LAD) occlusion.1 In contrast to our initial belief, the culprit vessel turned out to be the nondominant RCA, and there was no significant obstruction in the left coronary arteries. Emergency revascularization of the RCA by PCI led to resolution of chest pain and normalization of precordial ST-segment deviation on ECG. The precordial STE was believed to result from the right ventricle (RV) ischemic injury due to proximal occlusion of the nondominant RCA and RV branches.
Proximal occlusion of a dominant RCA may cause infarcts of inferior LV and RV. Concomitant infarctions in RV and inferior LV can cause STE in both anterior and inferior leads.2,3 However, in most patients with RV and inferior LV infarctions, precordial STE is absent. The ECG manifestations of RV injury may be dominated by the electrical forces of the simultaneous inferior or inferolateral LV injury,4 and as a result, only inferior but no anterior STE is seen. Whether anterior STE develops with proximal RCA occlusion may also be affected by RV infarct topography. A study showed that posterior RV infarct had more RV involvement than anterior RV infarct.5 On the other hand, the STE can be associated with reciprocal STD (RSTD) in remote leads directly opposite to the leads showing STE.1 Reciprocal STD can be just a mirror image of the classic STE in the opposite location or a result of myocardial ischemia remote from the infarct site. Precordial RSTD can occur during inferior STEMI.
In general, the RV is supplied by the RCA through RV marginal branches. Right coronary artery occlusion-related anterior STE has been reported in the setting of proximal occlusion of a nondominant RCA,6,7 conus branch occlusion from a dominant RCA,8 or proximal RCA occlusion with good collateral formation from other arteries.9,10 In the current case, the totally occluded nondominant RCA supplied primarily the RV while the inferior LV was supplied by the left posterior descending artery from the dominant LCx. This explains the lack of inferior infarction; therefore, no inferior STE and associated precordial RSTD would be expected. The absence of inferior LV infarction to offset the anterior spatial vector arising from RV infarct allowed the RV infarct-derived electrical force to predominate, hence manifesting as STE in the anterior/precordial leads.
Clinical Significance
Right ventricle infarction requires high suspicion due to its relation to shock and RV failure requiring volume resuscitation. For nondominant RCA lesions, many cardiologists choose to treat medically without intervention. However, life-threatening ventricular tachycardia or fibrillation can happen due to nondominant RCA total occlusion involving the conus artery or RV branches.6,7 Therefore, revascularization of an occluded nondominant RCA as the culprit vessel of STEMI can be lifesaving.
Take-home Points
Isolated anterior/anteroseptal STE can develop due to total proximal occlusion of a nondominant RCA, mimicking anterior STEMI from proximal LAD occlusion.
The mechanism underlying this paradoxical ECG phenomenon could be a result of RV infarct-related anterior STE becoming predominant because of a lack of counterbalancing force from inferior LV as would be expected in the setting of dominant RCA total occlusion causing inferior LV and RV infarction.
Due to the risk of RV infarction and associated life-threatening ventricular arrhythmia, timely revascularization of a proximally occluded nondominant RCA as the culprit vessel of anterior STEMI is needed.
(24). Thierry Carrel et al. Acute aortic dissection. The Lancet 2023;401(10378):P773-788.
Although substantial progress has been made in the prevention, diagnosis, and treatment of acute aortic dissection, it remains a complex cardiovascular event, with a high immediate mortality and substantial morbidity in individuals surviving the acute period. The past decade has allowed a leap forward in understanding the pathophysiology of this disease; the existing classifications have been challenged, and the scientific community moves towards a nomenclature that is likely to unify the current definitions according to morphology and function. The most important pathophysiological pathway, namely the location and extension of the initial intimal tear, which causes a disruption of the media layer of the aortic wall, together with the size of the affected aortic segments, determines whether the patient should undergo emergency surgery, an endovascular intervention, or receive optimal medical treatment. The scientific evidence for the management and follow-up of acute aortic dissection continues to evolve
(25). Nitish Mondal. The resurgence of dengue epidemic and climate change in India. 2023;401:P727-728.
Climate change is influencing the incidence of Aedes aegypti and Aedes albopictus mosquito-borne dengue illnesses. More than half of the world’s population is in danger, with an annual estimate of 100-400 million infections, 96 million clinical symptoms, and 40 000 fatalities. Despite evidence of 30-50-fold increases in occurrences in tropical and subtropical regions in the past 50 years, and the fastest growing risk of dengue infection, an estimated 3·97 billion people (in 129 countries) are vulnerable.2, 3 Dengue disease has steadily increased in the past half century as a result of various factors including global trade and travel, urbanisation, population growth, and climate variability and change, all of which provide conducive conditions for dengue vectors and viruses to multiply.3, 4 Climate change, rising temperatures, urbanisation, vector suitability, and vulnerability of populations threaten dengue vector-to-human transmission.3, 4
In the 1950s and 1960s, the disease was restricted to a few southeast Asian countries, but regional and worldwide dengue epidemics began in the 1970s and spread in the next two decades. By 2012-13, the face of dengue incidence in India radically transformed. Dengue has become an annual epidemic in many parts of southeast Asia, and the disease is becoming more hazardous as the environment changes. According to the most recent data, 110 473 dengue cases were documented in India between January and October, 2022, which is similar to the number of cases reported in 2018 (101 192). Notably, there was a substantially higher number of dengue cases recorded in previous years: 188 401 in 2017; 157 315 in 2019; and 193 245 in 2021.5 When the COVID-19 wave began in India in 2020, dengue incidence reduced by 56-60% (44 585).5 Between 1951-60 and 2012-21, the number of months appropriate for A aegypti dengue transmission in India increased by 1·69% every year to 5·6 months.6 However, locations with endemic dengue face the risk of a twin pandemic, which could overwhelm health-care systems as the world grapples with the weight of the COVID-19 pandemic, and could be difficult to discern due to clinical and laboratory markers that are similar.7
We must not underestimate the current COVID-19 pandemic’s severity, which has wreaked havoc in terms of morbidity, mortality, and economic burden, and has occasionally affected the prevention, control, and management programme of infectious and vector-borne diseases, including dengue, as a result of changes in health policy and priorities related to COVID-19. The rising frequency of dengue and COVID-19, and the possibility of co-infection, are putting a strain on health-care infrastructure. Reducing transmission and fatality will be made possible by treating dengue cases as soon as possible and addressing the socioeconomic and environmental factors associated with dengue and other vector-borne illnesses.
(26). Richard Pham. Wide QRS Complex Transient Pattern in a Patient With Severe COVID-19. JAMA Intern Med. 2023.
A patient in their 60s presented to the emergency department with shortness of breath for a duration of 2 days. The patient had no known medical history and was not vaccinated against the COVID-19 virus. On admission, the patient’s COVID-19 test result was positive, with computed tomography pulmonary angiography results revealing multifocal opacities that were consistent with COVID-19 pneumonia, but no pulmonary embolism. The patient had an unremarkable electrocardiogram (ECG) and echocardiogram results during the first few days of hospitalization. The patient’s illness progressed, and they developed acute respiratory distress syndrome that required intubation and proning. The patient’s course was also complicated by acute kidney failure, ultimately requiring them to undergo hemodialysis. On day 11, the intensive care team noted unusual changes in the patient’s telemetry results (frontal leads II and III) (Figure, A).
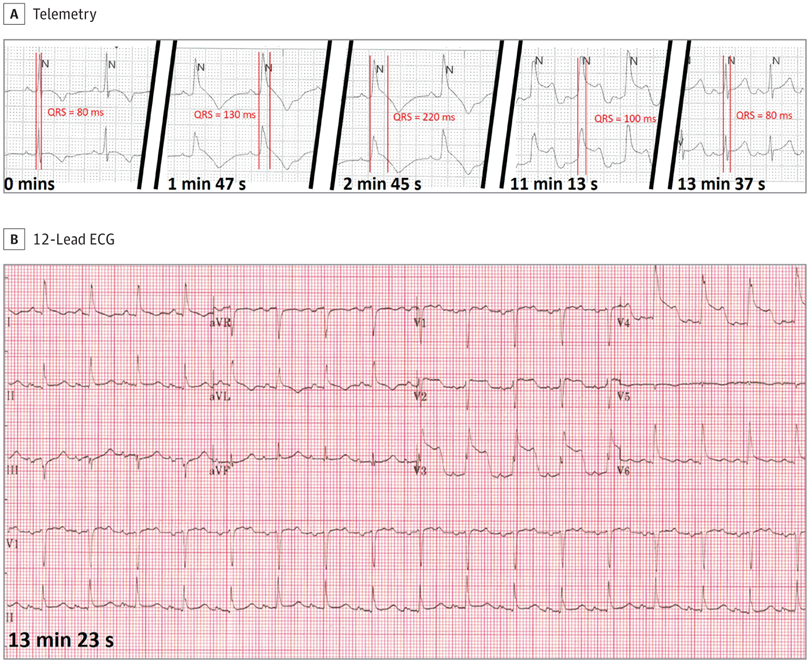
A, Transient progressive QRS widening is demonstrated on telemetry at various points. The displayed leads are the frontal leads II and III. B, A 12-lead ECG during the time of the event obtained at 13 minutes and 23 seconds demonstrating acute ST-segment elevation in leads V2 to V4.
Questions:
What findings were observed in the patient’s telemetry, and what is the potential mechanism for these changes?
Interpretation and Clinical Course
The patient’s telemetry results showed a progressive widening and then narrowing of the QRS complex over approximately 13 minutes. Although there was a gradual increase in the patient’s rate, there was intact 1:1 atrioventricular conduction with P-wave morphologies consistent with sinus rhythm. At 11 minutes and 13 seconds, there were notable ST-segment changes as the QRS complex narrowed, with concerns for ischemia. A 12-lead ECG was performed and confirmed the ST elevations in the anterior leads at 13 minutes and 23 seconds. Repeated 12-lead ECG 5 minutes after showed resolution of the ECG changes. Additional data obtained at the time of these telemetry findings included normal potassium levels and a modest troponin peak of 7.28 ng/mL (to convert to μg/L, multiply by 1), with echocardiogram results showing an ejection fraction of 45% to 50% without wall motion abnormalities. Given the resolution of the patient’s transient ST elevations, catheterization with invasive coronary angiography was deferred until the patient was more stable. The patient continued to require maximum ventilatory support and died on day 14 of admission.
Discussion
The differential for the widening of the QRS waveform with sinus rhythm includes aberrant conduction, hyperkalemia, accessory pathway conduction, and ischemia. Widening of QRS may also be seen in the antiarrhythmic use of class 1 sodium blockers. Aberrant conduction may occur during atrial tachycardias without adequate time for repolarization of part of the conduction system, which is followed by broader QRS complexes. In this patient with normal baseline ECG results and no known prior conduction disease during a stable sinus rate, it is unlikely aberrant conduction. The transient nature of this rhythm without characteristic peaked T waves and other features, such as PR prolongation, P-wave flattening, or bradycardia, makes hyperkalemia unlikely as the mechanism, and potassium levels were confirmed to be normal. Enhanced accessory pathway conduction may manifest at different heart rates, especially when there is variable conduction velocity within the atrioventricular node, which can result in variability of the QRS duration. However, there was less concern for preexcitation without evidence of a δ wave in this patient. Additionally, this patient was not receiving antiarrhythmic therapy for any effects by sodium channel blockade resulting in QRS widening.
A, Transient progressive QRS widening is demonstrated on telemetry at various points. The displayed leads are the frontal leads II and III. B, A 12-lead ECG during the time of the event obtained at 13 minutes and 23 seconds demonstrating acute ST-segment elevation in leads V2 to V4.
In this case, we describe a patient with severe COVID-19 at risk for ischemia. COVID-19 is associated with various cardiac manifestations, including myopericarditis,1 coronary vasospasm,2-4 hypercoagulability leading to coronary thrombus,5 and conduction abnormalities.6 This patient’s telemetry manifestation was accompanied by 12-lead ECG evidence of ST-segment elevations and laboratory evidence of myocardial injury with troponin level elevation and subsequent resolution. The resolution of these changes within minutes on telemetry and ECG with down-trending troponins was highly suggestive of transient transmural ischemic injury either due to transient coronary spasm or coronary thrombus with subsequent lysis. This characteristic appearing QRS pattern, known as the triangular QRS-ST-T waveform pattern, has been described previously but is rare. This is a high-risk ECG feature associated with a large burden of myocardial ischemia.7,8 The blurring of the QRS complex due to its fusion with the ST segment and T-wave results in what has been described as a shark-fin pattern that represents ST deviation in the setting of ischemia. It is also known as λ wave or giant R waves.7 This pattern has also been reported in acute myocarditis, as well as Takotsubo cardiomyopathy,9,10 representing repolarization abnormalities in those settings. Although this pattern is associated with acute myocardial infarction and frequently complicated by cardiogenic shock or cardiac arrest, this patient presented transiently in the setting of severe COVID-19, and the cause of death was respiratory failure.
Take-home Points
The differential of widening of the QRS includes aberrant conduction, hyperkalemia, accessory pathway conduction, and antiarrhythmic use, but also ischemia.
A shark-fin pattern is a rare but serious marker of ischemia.
COVID-19 can be associated with ischemia via mechanisms that may be transient, such as coronary vasospasm or thrombus formation.
(27). Xingli Xin, et al. Incorrect ECG diagnoses?-Follow the Leads. JAMA Intern Med. 2023.
An individual in their early 70s presented to the emergency department with frequently recurring paroxysmal chest pain; each episode had a duration of 3 to 5 minutes. The patient had a medical history of hypertension and diabetes mellitus; vital signs were normal, except for elevated blood pressure (153/92 mm Hg). Chest auscultation revealed normal breath and heart sounds with no murmurs. The laboratory test results (hemogram, serum electrolytes, and troponin I and D-dimer levels) were all within normal limits. A chest radiograph showed no abnormality, and transthoracic echocardiography findings revealed normal left ventricular systolic function (ejection fraction, 60%). The electrocardiogram (ECG) tracing obtained on admission is shown in the Figure, A.
Electrocardiogram (ECG) Findings Before and After Correcting the Lead Placement
A, The initial ECG shows a negative P wave (magenta arrowheads) in lead I, a positive P wave (black arrowheads) in lead aVR, and a diminishing amplitude progression of QRS complex from V1 to V6. The tracing also reveals giant T waves in all leads except lead III. The prolonged corrected QT interval was 644 milliseconds (ms). B, A repeated ECG reveals a positive P wave in lead I and a negative P wave in lead aVR-characteristic of a P wave in sinus rhythm. In addition, the amplitude of the QRS complex in leads V1 to V6 returned to normal. T-wave inversion in leads I, II, aVL, and V2-V6 suggests anterior myocardial ischemia. The QTc interval was 437 ms (normal range).
Questions:
What is the most likely explanation for the ECG findings in the Figure, A? What would you do next?
Interpretation
The initial ECG tracing reveals a negative P wave (magenta arrowheads) in lead I, a positive P wave (black arrowheads) in lead aVR, and a diminishing QRS complex amplitude progression from V1 to V6. In addition, the ECG reveals giant T waves in all the leads except lead III. The prolonged corrected QT interval was 644 milliseconds (ms).
When we examined the placement of the leads on the patient’s body , we observed the following: (1) right-left arm lead reversal, (2) placement of electrodes of the precordial leads on the right side of the chest, and (3) placement of left arm electrode over the left radial artery, which produced artifacts (giant T waves) on the ECG tracing. Therefore, before proceeding with further patient care, we performed another ECG, ensuring that the precordial leads were placed on the left side of the chest and that the left and right arm electrodes were placed correctly and not clipped on the radial artery. The repeated ECG (Figure, B) with corrected lead placement revealed sinus rhythm with T-wave inversion in leads I, II, aVL, and V2 to V6.
Clinical Course
The patient was diagnosed with unstable angina pectoris. Results of a coronary angiography showed 90% stenosis in the proximal left anterior descending coronary artery. A drug-eluting stent was placed, and the patient was discharged from the hospital 4 days later.
Discussion
When electrodes are placed in the wrong anatomic locations or clipped on the radial artery, they can produce incorrect ECG diagnoses. If the electrodes of leads V1 to V6 are placed on the right side of the chest, the amplitude of the QRS complex will gradually decrease from lead V1 to V6. When the left and right arm leads are placed inversely, the ECG manifests as follows1: (1) the P-QRS-T waves are inverted in lead I, ie, lead I is flipped (P wave is negative); (2) lead aVR resembles a normal aVL (P wave of aVR is positive), and lead II resembles a normal lead III; and (3) the precordial leads and aVF are unaffected. When the 2 aforementioned electrode misplacements occur simultaneously, the ECG characteristics will be the same as those of mirror-image dextrocardia.2 No mirror-image dextrocardia was found after performing a physical examination and chest radiography of the patient; therefore, these ECG changes denoted an instance of electrode misplacement.
When a limb-lead electrode is placed over the radial pulse, the artifact is recorded on the ECG.3 Moreover, the pulsation of the radial artery may allow for poor electrode contact, which may produce sharp changes in electric impedance, thus distorting the electric signals.4 These distorted signals may manifest as phase shifts and produce ECG artifacts, such as giant T waves, ST-segment elevation, ST-segment depression, abnormal U waves, and prolonged QTU intervals.5,6 In this case, these artifacts appeared after the QRS complex. The QRS complex appears when the heart’s contraction is being initiated; therefore, these artifacts appeared when the contraction of the ventricles produced arterial pulsation. The initial ECG recorded pulse-tapping artifact (giant T waves) associated with the left radial arterial pulsation, and the giant T-wave, in turn, led to a prolonged corrected QT interval.
According to the Einthoven triangle theory,6 lead I compares the electrical differences between the right and left arms; lead II, between the right arm and left leg; and lead III, between the left arm and leg. Therefore, when the artifacts originate from the left arm, the lead between the right arm and left leg (lead II) remains normal. Similarly, when the artifacts originate from the right arm, the lead between the left arm and leg (lead III) remains normal. When the artifacts originate from the left leg, the lead between the left and right arms (lead I) remains normal. Artifacts associated with arterial pulsation also affect the precordial leads because the Wilson central terminal is produced by connecting the 3 limb electrodes.6 Therefore, only 1 limb lead (I, II, or III) will remain unaffected when a single limb arterial pulsation is the source of the artifacts.
In this patient’s initial ECG, only lead III remained unaffected (without giant T waves); therefore, according to the aforementioned analysis, it appeared that the artifacts originated from the right radial arterial pulsation. However, because the electrodes on the left and right arms were reversed, the artifacts actually originated from the left radial arterial pulsation.
Take-home Points
When electrodes for leads V1 to V6 are placed on the right side of the chest, the amplitude of the QRS complex will gradually decrease from lead V1 to V6.
When 1 limb lead electrode is placed over the radial pulse, the artifact is recorded on the ECG tracing.
Only 1 limb lead (I, II, or III) will remain unaffected when a single limb arterial pulsation is the source of the artifacts.
Artifacts associated with limb arterial pulsation appear after the QRS complex.
(28). Huei-Jing Wang, et al. Malignant acanthosis nigricans. N Engl J Med 2023; 388:1031
This is a paraneoplastic dermopathy involving the sudden onset of velvety plaques on cutaneous and mucosal surfaces. These changes are more extensive and rapidly worsening than those in benign acanthosis nigricans. The CT of the abdomen and pelvis showed thickening of the gastric body and a solid mass in the right ovary. A gastric biopsy showed mucin-rich signet-ring-cell gastric adenocarcinoma, confirming a diagnosis of gastric adenocarcinoma with ovarian metastasis.
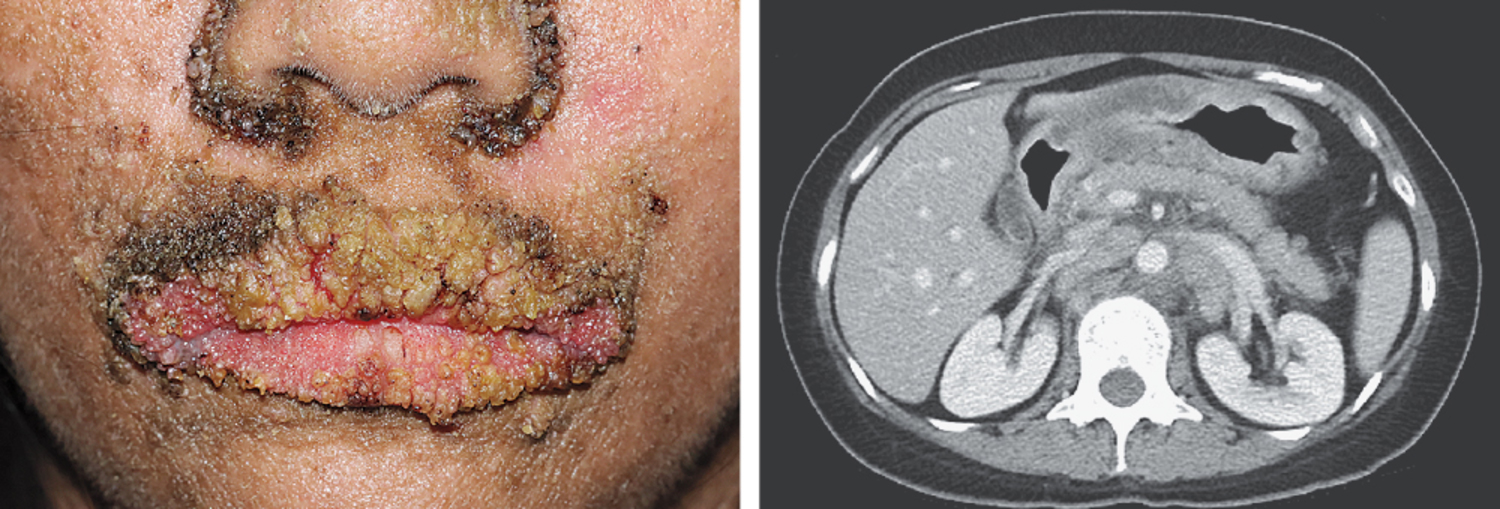
(29). Oliver T Mytton, et al. Approach to a child or young person with concerns about excess weight. BMJ 2023;380:e074255.
What you need to know
Excess weight can contribute to poor health in childhood or may be an indicator of other physical or emotional problems
Use child specific tools (eg, z-BMI) alongside clinical judgment to assess a child’s weight status and to identify children who may benefit from intervention
Use sensitive and appropriate language when discussing weight with parents and their children, and where possible offer practical strategies for changing eating habits, activity patterns, or sleeping behaviours
An increasing range of treatments and other interventions is available to support children with excess weight, although access to services varies by area
Excess weight (overweight or obesity) in childhood is common.1 In England, 22.2% of children in school reception year (age 4-5) have excess weight, and 37.7% in year 6 (age 10-11). Excess weight can contribute to substantial physical and emotional problems in childhood, as well as in later life, and may be an indicator of health problems.1
Discussing weight can be emotive, and raising the issue in a short consultation without implying blame or judgment can be challenging, particularly where a child’s weight is not perceived as a problem by the parents and is not the presenting issue.
Excess weight is a public health issue that needs to be addressed using public health measures,12 and genetic and environmental factors that contribute to its development may be outside the influence of doctors or parents, but doctors (particularly GPs and paediatricians) still have an important role in managing it.1 These clinicians are well placed to identify the issue and offer or signpost evidence informed support to families and children.123 Understanding and reflecting some of the challenges of managing excess weight can be important when raising the issue in consultations.
This article offers an approach to recognising and discussing excess weight. Full paper is NOT free to access
(30). Ka Yan Cheung, et al. Health and nutrition claims for infant formula: international cross-sectional survey. BMJ 2023;380:e071075. Objectives:
To review available health and nutrition claims for infant formula products in multiple countries and to evaluate the validity of the evidence used for substantiation of claims.
Design International cross sectional survey:
Setting Public facing and healthcare professional facing company owned or company managed formula industry websites providing information about products marketed for healthy infants delivered at full term in 15 countries: Australia, Canada, Germany, India, Italy, Japan, Nigeria, Norway, Pakistan, Russia, Saudi Arabia, South Africa, Spain, the United Kingdom, and the United States in 2020-22.
Main outcome measures:
Number and type of claims made for each product and ingredient. References cited were reviewed and risk of bias was assessed for registered clinical trials using the Cochrane risk of bias tool, and for systematic reviews using the Risk Of Bias in Systematic reviews tool.
Results
: 757 infant formula products were identified, each with a median of two claims (range from 1 (Australia) to 4 (US)), and 31 types of claims across all products. Of 608 products with ≥1 claims, the most common claim types were “helps/supports development of brain and/or eyes and/or nervous system” (323 (53%) products, 13 ingredients), “strengthens/supports a healthy immune system” (239 (39%) products, 12 ingredients), and “helps/supports growth and development” (224 (37%) products, 20 ingredients). 41 groups of ingredients were associated with ≥1claims, but many claims were made without reference to a specific ingredient (307 (50%) products). The most common groups of ingredients cited in claims were long chain polyunsaturated fatty acids (278 (46%) products, 9 different claims); prebiotics, probiotics, or synbiotics (225 (37%) products, 19 claims); and hydrolysed protein (120 (20%) products, 9 claims). 161/608 (26%) products with ≥1 claims provided a scientific reference to support the claim-266 unique references were cited for 24 different claim types for 161 products. The reference types most frequently cited were clinical trials (50%, 134/266) and reviews (20%, 52/266). 28% (38/134) of referenced clinical trials were registered, 14% (19/134) prospectively. 58 claims referred to 32 registered clinical trials, of which 51 claims (27 trials) related to a randomised comparison. 46 of 51 claims (90%) referenced registered clinical trial outcomes at high risk of bias, and all cited systematic reviews and pooled analyses, carried a high risk of bias.
Conclusions
: Most infant formula products had at least one health and nutrition claim. Multiple ingredients were claimed to achieve similar health or nutrition effects, multiple claims were made for the same ingredient type, most products did not provide scientific references to support claims, and referenced claims were not supported by robust clinical trial evidence.
(31). Mohammed D et al. The role of faecal calprotectin in the diagnosis of inflammatory bowel disease. BMJ 2023;380:e068947
What you need to know
Faecal calprotectin testing is recommended in patients <60 years old with lower gastrointestinal symptoms and normal initial workup to exclude causes of colonic inflammation
A normal faecal calprotectin result has a high negative predictive value for inflammatory bowel disease, and prevents unnecessary investigation when the most likely diagnosis is irritable bowel syndrome
Faecal calprotectin should not be used in patients older than 60 or if colorectal cancer is suspected
Faecal calprotectin is a sensitive marker of intestinal inflammation and may be elevated in conditions other than inflammatory bowel disease, such as diverticulitis and infectious gastroenteritis, or when patients take medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin
Gastrointestinal and abdominal symptoms are common in general practice, being recorded in up to 10% of consultations.1 The symptoms can be caused by a variety of conditions including inflammatory bowel disease and functional disorders such as irritable bowel syndrome. It is often difficult to distinguish between inflammatory bowel disease and irritable bowel syndrome on history and examination alone. Patients with irritable bowel syndrome may undergo costly, invasive, and unnecessary investigations (typically in the form of lower gastrointestinal endoscopy) in order to rule out other conditions
(32). Ute Eppinger. How to Recognize and Treat Hidden Inflammation. Medscape 2023.
Immunoglobulin G4 (IgG4) fights viruses and bacteria. However, sometimes it targets the body itself. “This then leads to inflammation, the healing of which the body is unable to keep under control,” explained Ulf Müller-Ladner, MD, PhD, chairperson of the German Society of Internal Medicine (DGIM).
At the DGIM annual press conference, Müller-Ladner, who is also director of the Department of Rheumatology and Clinical Immunology at the Kerckhoff Clinic in Bad Nauheim, explained how IgG4 inflammation is triggered throughout the body and what therapeutic options are available.
Many Manifestations
IgG4-associated inflammation can affect one or more organs or the surrounding connective tissue and cause fibrosis. As a result of fibrosis, the organ gradually loses function and is eventually transformed completely into scarred connective tissue.
“In the case of IgG4-associated inflammation, these fibroses have a histological structure, but extracting a sample is not possible from every affected organ,” said Müller-Ladner. Liver, bile ducts, blood vessels, skin, eyes, or even the central nervous system – practically every organ system can be affected by these inflammatory reactions.
IgG4-associated diseases have likely been around for some time, but it is only in the past 10 years that awareness has grown that, despite various manifestations, “they are all one and the same disease,” said Müller-Ladner.
IgG4-associated chronic, inflammatory, fibrosing diseases were only classified together as a single entity in the past few years. In terms of pathophysiology, B lymphocytes, IgG4-positive plasma cells, follicular T-helper cells, cytotoxic CD4-positive T cells, and macrophages work together and trigger an inflammatory reaction, which then encourages fibroblasts to overproduce connective tissue.
Beware Inexplicable Inflammation
It is estimated that 1 in 100,000 people suffer from the disease, but the number of incorrectly categorized patients may be significantly higher.
The diagnostic challenge lies in the fact that IgG4-associated inflammation occurs in almost every organ. It can cause different symptoms, depending on the organ affected.
Müller-Ladner provided the following take-home message: “Every inexplicable inflammation event and every organ dysfunction, especially if associated with an increase in connective tissue, could be an IgG4-associated disease. Keeping this in mind is the key to recovery.”
With most people, the inflammation persists for many years before any symptoms of the disease develop. Highly acute courses of progression are also possible.
Classic symptoms, such as fever, are not so characteristic of the latent inflammatory reaction, and according to classification criteria published by specialist rheumatology societies, they are an exclusion criterion. This is true with respect to the differential diagnosis for vasculitis, which also occurs throughout the body.
Histology Is Key
Blood levels of IgG4 and imaging are not always enough to confirm the diagnosis. In such cases, the histology is often a crucial factor in making a definitive diagnosis. Dominant organs in IgG4-associated diseases are the pancreas, the liver, the gallbladder, the intestines, the retroperitoneum, large blood vessels, the kidneys, the heart, the brain, saliva, tear ducts, as well all of the body’s connective tissue.
The kidneys play host to inflammation in the connective tissue and space-occupying masses in particular. “If the pancreas is affected, the signs can vary from diffuse swelling to the onset of diabetes mellitus. In contrast, if the aorta is affected, then the inflammation is characterized through a thickening of the vessel walls, aneurysms, and the corresponding circulation disorders,” said Müller-Ladner.
Because of the long period before the diagnosis is made, more than 50% of patients exhibit irreversible organ damage at the time of diagnosis, he added.
Glucocorticoids and Immunosuppressants
Despite therapeutic intervention, the disease can have a fatal outcome, even if the patient is young, said Müller-Ladner. Glucocorticoids are the current therapy of choice. The dose is more than 0.5 mg of prednisolone equivalent per kg of body weight. “This usually leads to a rapid improvement in the inflammation. Subsequently, every organ is thoroughly diagnosed to assess the severity of the disease and to plan further treatment steps.”
In the long term, proven immunosuppressants, such as azathioprine, mycophenolate, leflunomide, and methotrexate, can be used, just as for many other chronic inflammatory diseases. Cyclophosphamide or cyclosporine is used more rarely, owing to their side effect profiles.
Because of the B-cell dominance, B-cell-depleting therapy with rituximab is currently a highly effective therapeutic option but one that must be applied for, because such use is off label. “If the body responds well to the medication, organ function often recovers,” said Müller-Ladner.
(33). Zoe Kleinman. Can mind-controlled VR games help stroke patients? 2023
A system which can translate human brain activity into actions without any physical movement is being developed by a neurotech firm called Cogitat.
When wearing a prototype headset, basic actions in virtual reality can be carried out by thinking about them.
So for example, in a game where a VR jet ski is controlled by handles, you move by thinking about it, rather than squeezing your hands.
Elon Musk’s firm Neuralink is developing a similar concept.
It is called brain-computer interface and there are many neurotech companies exploring it.
One aim is that it could eventually allow people who have suffered a stroke, or have other brain injuries, to control phones or computers remotely.
Neuralink’s method requires a chip being placed into the brain itself. The firm has so far only worked with animals, and has been criticised for their treatment. It has released videos it says demonstrate a monkey playing the video game Pong with its mind, and the brain activity of a pig with a chip implanted in its brain.
Cogitat is one of the firms developing a system which works on top of the head rather than inside it.
It could one day take the form of a headband worn with a VR headset. Some companies are already creating their own hardware but, as a university spin-off, Cogitat is concentrating only on the tech behind it.
It is led by NHS consultant Allan Ponniah and computer scientist Dimitrios Adamos from Imperial College London.
The tech is in developmental stages, but has already been tried out on stroke patients, with positive results. The aim is to encourage them to continue with rehabilitation exercises by making them more engaging.
“When a person has had a stroke, and they can’t move their arm, they’re very demotivated to partake in rehabilitation. But our technology will allow them to imagine moving their hand and seeing a hand move on the screen, which we believe will motivate them to start their course of physiotherapy,” Mr Ponniah told BBC podcast Tech Tent.
Weird experience
I tried it out and it is a very weird experience. For starters, it is harder than it sounds to think about making a movement without actually making it. And you also have to try not to think about other things, which increases your brain activity and creates more noise for the tech to decode while it looks for the motor signal.
I had never seen my own brain activity laid out on a screen in front of me in real time before, like a complicated, multi-layered cardiogram. That was strange in itself – seeing the essence of my thoughts on a graph. But when you hear that VR jet ski engine roar, just because you have thought about doing it, it is an incredible feeling.
Of course the prototype device was not totally reading my mind. It was not translating my thoughts or looking deep into my soul. It was only focused on motor skill signals.
“If you don’t choose to interact with the system, nothing happens,” says Mr Adamos. “There’s nothing picked up from you if you stop using it.”
Other firms focus on different types of brain activity – visual signals for example, so you can focus on a number and press buttons on a screen. It is also possible – but controversial – to concentrate on more personal responses such as likes and dislikes.
Cogitat says it expects to have a working prototype of its technology within the next 12 months – but there are several challenges which still lie ahead for neurotech.
Experts are still learning about brain activity. It is individual to each of us and it is not constant. It changes throughout the day and may be affected by factors like tiredness and dehydration as well as ageing. This means any brain activity reading systems require continual recalibration.
Cogitat is training its tech on a database of hundreds of volunteers who have been testing it out, which speeds up the calibration process. I met some of the team – mostly students, who were very enthusiastic, not to mention patient, as they guided me through the demonstration.
Mr Adamos tells me proudly that in a recent global machine-learning competition, Cogitat not only took first place but also beat a team from the US Army.
He offered everybody some time off to celebrate – but nobody took it.
“They were all in the next day,” he says. “It’s really fascinating for us, and everybody who’s joined this journey.”
(34). Ana B Espinosa-Gonzalez et al. Orthostatic tachycardia after covid-19. BMJ 2023;380.
What you need to know
Tachycardia on standing or minimal exertion may occur after covid-19 and may cause substantial functional impairment
When assessing a patient with tachycardia, consider potential causes including autonomic dysfunction
Measures to reduce tachycardia can greatly improve function and ability to return to activities and work
Patients with long covid-defined by the National Institute for Health and Care Excellence (NICE) as signs and symptoms that persist for more than four weeks (and especially more than 12 weeks) following acute covid-1912-may present in primary care with symptoms of palpitations (tachycardia) triggered by standing or minimal exertion.3 These may be accompanied by dizziness, breathlessness, chest pain, sweating, bloating, fatigue, and other symptoms which may be caused by a dysfunction of the autonomic nervous system (dysautonomia).45678910111213 Patients can find these symptoms debilitating and they can affect function and mood. Limited evidence, variable diagnostic criteria, uncertainty around cause and pathogenesis, and the absence of licensed medications, have all contributed to making this a difficult condition to diagnose and manage.
(35). Kathy Leung, et al. Controlling avian influenza. BMJ 2023;380:p560.
A One Health approach that links human, animal, and environmental health is essential
Global reports of highly pathogenic avian influenza A(H5N1) in birds are increasing, with cases reported from every region except Australasia and Antarctica since 2020.1 The global spread of these avian influenza outbreaks is unprecedented, exacting large economic losses to poultry industries and tourism, and posing a substantial threat to global health security and animal ecology.
In Europe, 2520 H5N1 outbreaks were reported in poultry between October 2021 and September 2022, and the virus was also detected in 3867 dead wild birds.2 The US reported 131 mammalian H5N1 infections among bears, foxes, raccoons, skunks, and seals between May 2022 and February 2023.3 In October 2022, an H5N1 outbreak among Spanish farmed minks was reported for the first time,4 triggering concerns that the virus might soon become transmissible between humans (mink are physiologically similar to ferrets, the animal model used to study transmissibility of influenza viruses among humans).5
On 24 February 2023, an 11 year old girl died from an H5N1 avian flu infection in Cambodia
