Journal scan
From the desk of the Editor-in-Chief
(1). Presha Kardile. Learning to live in a body at war with itself. BMJ 2022;377:o784.
Presha Kardile explains how health professionals could have better helped her prepare for life ahead after a diagnosis of lupus
I started having symptoms in my early 20s that were initially dismissed as irritable bowel syndrome. My health worsened over the course of a year, with hair loss, severe fatigue, and joint pain adding to an ever-increasing list of strange symptoms. As a last resort I had several antibody tests which eventually led to a diagnosis of systemic lupus erythematosus (“lupus”). This brought with it a sense of relief after years of misdiagnoses, but also filled me with dread about the future in equal measure.
After starting treatment, I focused on beating the disease so I could get back to normal. It took a while for me to realize that this approach did not make sense, as there was nothing external attacking my body. By trying to beat my condition, I was fighting against my own overactive immune system. This helped me accept my diagnosis and focus on moving forward.
Learning to adjust
I experienced a profound grief while letting go of the life I had lived. I tried to find the courage to face the tsunami of changes to come. These included learning to adjust to new medications that would leave me immunocompromised, and living in social isolation with an increased dependency on my care giver. These unwelcome changes deeply affected my mental health.
Support for my mental health was, and still is, crucial in ensuring a smoother transition to my new normal. A psychologist helped me manage my fear of taking the hoard of medications that I was suddenly expected to take every day. They helped me cope with the devastating realisation, as a young person, that I would potentially need to be on medication for the rest of my life.
Finding support
Daily mindfulness practices help me manage my pain. These practices are tailored to the needs of people who experience chronic pain, and they are practically achievable, considering that the intensity of the pain varies each day and can manifest itself in different parts of the body. I found a support group for people with chronic pain, which focused on acknowledging pain and the suffering that comes with it, rather than trying to put a positive spin on it. This helped me cope with my isolation and added to my existing support network. I also attended several online alternative therapy workshops that used art, dance, movement, and music as forms of expression. These introduced me to practices and resources that used my existing hobbies to help me cope with my new reality and support my mental wellbeing.
It took an incredible amount of research to find these groups and the courage to take the first step to seek help. It would have helped if, early on in my diagnosis, my healthcare professionals had shared the types of mental health support available. Being given a list of vetted resources would have helped me and my caregivers navigate the uncertainty without the additional pressure of finding groups and individuals I could trust.
What you need to know
Coming to terms with the diagnosis of a chronic illness and learning to live with it are ongoing processes that can bring relief as well as dread
One-to-one counselling, support groups, and alternative therapies can help patients adjust to their new normal
Having mental health support, where both patients and their caregivers can voice concerns and address misconceptions, is important in helping accept the changes brought on by a chronic illness diagnosis
Education into practice
How could you ensure that your patients feel supported during diagnosis of a chronic illness?
How might you incorporate an ongoing conversation about mental wellbeing into long term management of a condition?
How can you inform and educate your patients on the types of mental health support available during a new diagnosis?
(2). Boris Decourt, et al. The importance of genomics in advancing the diagnosis and treatment of dementia. 2022.
The incidence and prevalence of Alzheimer’s disease and related dementias continue to rise as life expectancy increases worldwide. If these diseases could be diagnosed accurately before symptom onset, strategies could be developed to protect brain neurodegeneration and enable endogenous and exogenous neuroplastic repair mechanisms to continue to maintain a sufficient level of cognitive function. However, a major hindrance to improving the diagnosis of Alzheimer’s disease is that the aetiology remains unclear. Pathological mechanisms of genetic origin have been proposed (eg, mechanisms involving the APOE ε4 allele). However, genetic mutations that could lead to disease in non-hereditary forms of Alzheimer’s disease and related dementias (ie, sporadic cases) are rare and diverse in the general population, requiring highly advanced analyses of multiple genetic datasets to link rare variants to clinically confirmed cases. The best method to accomplish this genetic linkage is use of genome-wide association studies (GWAS). Previous GWAS in transgenic mice and individuals with Alzheimer’s disease have indicated the involvement of genes associated with inflammation (such as TNF) and microglia (such as CD33 and TREM2) in Alzheimer’s disease and related dementias. However, novel loci have been reported in two new studies.
(3). Joel M. Palefsky. Treatment of anal high-grade squamous intraepithelial lesions to prevent anal cancer. N Engl J Med. 2022;386:2273-82.
Abstract
Background: The incidence of anal cancer is substantially higher among persons living with the human immunodeficiency virus (HIV) than in the general population. Similar to cervical cancer, anal cancer is preceded by high-grade squamous intraepithelial lesions (HSILs). Treatment for cervical HSIL reduces progression to cervical cancer; however, data from prospective studies of treatment for anal HSIL to prevent anal cancer are lacking.
Methods: We conducted a phase 3 trial at 25 U.S. sites. Persons living with HIV who were 35 years of age or older and who had biopsy-proven anal HSIL were randomly assigned, in a 1:1 ratio, to receive either HSIL treatment or active monitoring without treatment. Treatment included office-based ablative procedures, ablation or excision under anesthesia, or the administration of topical fluorouracil or imiquimod. The primary outcome was progression to anal cancer in a time-to-event analysis. Participants in the treatment group were treated until HSIL was completely resolved. All the participants underwent high-resolution anoscopy at least every 6 months; biopsy was also performed for suspected ongoing HSIL in the treatment group, annually in the active-monitoring group, or any time there was concern for cancer.
Results: Of 4459 participants who underwent randomization, 4446 (99.7%) were included in the analysis of the time to progression to cancer. With a median follow-up of 25.8 months, 9 cases were diagnosed in the treatment group (173 per 100,000 person-years; 95% confidence interval [CI], 90 to 332) and 21 cases in the active-monitoring group (402 per 100,000 person-years; 95% CI, 262 to 616). The rate of progression to anal cancer was lower in the treatment group than in the active-monitoring group by 57% (95% CI, 6 to 80; P=0.03 by log-rank test).
Conclusions: Among participants with biopsy-proven anal HSIL, the risk of anal cancer was significantly lower with treatment for anal HSIL than with active monitoring.
(4). Phoebe Wing-Lam Ho. Continuous glucose monitoring device causes consternation on chest x-ray. Lancet 2022;399(10344):P2412.
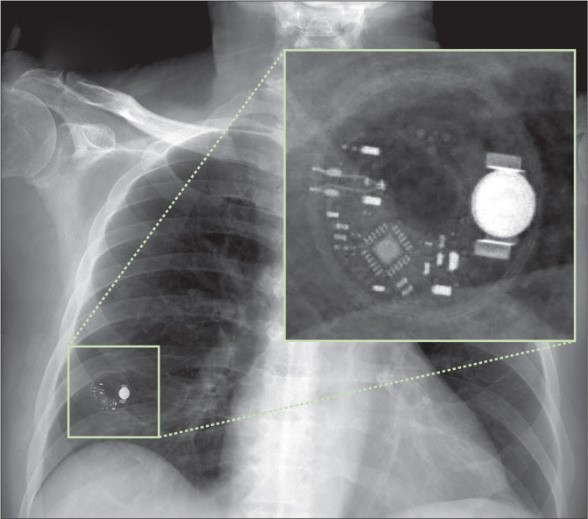
An 80-year-old man was admitted to our hospital with chest pain and shortness of breath.
The patient had a long medical history of diabetes, ischaemic heart disease, and end-stage kidney disease requiring regular haemodialysis.
On examination we found him to be in acute distress, with bilateral ankle oedema, and basal lung crackles. An electrocardiogram showed ST segment depression over leads V2-V6 and a Q wave in lead III. Laboratory investigations showed a serum cardiac troponin T concentration of 1297 ng/L (normal <14) with an unaffected creatinine phosphate kinase level.
We made a diagnosis of an acute non-ST elevation myocardial infarction.
1 day after a percutaneous coronary intervention with drug-eluting stent insertion into the right coronary artery and mid-left anterior descending artery, he began to repeatedly vomit; he also developed a low-grade fever with a temperature of 37.8oC. An urgent chest x-ray (figure) showed a radio-opaque nodule-not seen in previous x-rays-in the right lower lung field. We initially wondered whether the patient had aspirated his denture but on review of the lesion we were unconvinced. However, on closer inspection using magnification, we found the radio-opaque object had a complex internal structure consisting of a microchip, a battery, and an electronic circuit (figure). Before the film was sent for reporting, our physician examined the patient and found a subcutaneous continuous glucose monitoring (CGM) transmitter device (FreeStyle Libre Flash Glucose Monitoring System, Abbott Laboratories, Chicago, IL) which had been displaced from deltoid muscle to the patient’s back. We treated the patient as if he had a diagnosis of a nosocomial infection and his condition improved with intravenous piperacillin and tazobactam.
He was allowed home after 14 days and at follow-up 2 weeks later the patient was well with no angina or chest symptoms. However, the patient died 6 months later with a recurrent myocardial infarction.
In patients with a history of heart disease, unidentified electronic gadgets seen on chest x-ray might well be cardiac related-specifically pacemakers. Although CGM devices are typically located on the upper arm, they may slip-especially in semiconscious patients and those requiring frequent transfers-to other body parts. CGM devices may look like unexpected foreign objects on limited resolution x-rays. As CGM gains in popularity, health-care professionals should be able to identify CGM devices and be aware of their potential to move to unexpected positions where they may cause consternation on x-ray interpretation. Using appropriate magnification of x-rays may be necessary for recognising CGM devices.
(5). Pavel Strnad, et al. Fazirsiran for Liver Disease Associated with Alpha1-Antitrypsin Deficiency. 2022.
Abstract
Background: Alpha1-antitrypsin (AAT) deficiency results from carriage of a homozygous SERPINA1 “Z” mutation (proteinase inhibitor [PI] ZZ). The Z allele produces a mutant AAT protein called Z-AAT, which accumulates in hepatocytes and can lead to progressive liver disease and fibrosis. This open-label, phase 2 trial investigated the safety and efficacy of fazirsiran, an RNA interference therapeutic, in patients with liver disease associated with AAT deficiency.
Methods: We assigned adults with the PI ZZ genotype and liver fibrosis to receive fazirsiran at a dose of 200 mg (cohorts 1 [4 patients] and 2 [8 patients]) or 100 mg (cohort 1b [4 patients]) subcutaneously on day 1 and week 4 and then every 12 weeks. The primary end point was the change from baseline to week 24 (cohorts 1 and 1b) or week 48 (cohort 2) in liver Z-AAT concentrations, which were measured by means of liquid chromatography-mass spectrometry.
Results: All the patients had reduced accumulation of Z-AAT in the liver (median reduction, 83% at week 24 or 48). The nadir in serum was a reduction of approximately 90%, and treatment was also associated with a reduction in histologic globule burden (from a mean score of 7.4 [scores range from 0 to 9, with higher scores indicating a greater globule burden] at baseline to 2.3 at week 24 or 48). All cohorts had reductions in liver enzyme concentrations. Fibrosis regression was observed in 7 of 15 patients and fibrosis progression in 2 of 15 patients after 24 or 48 weeks. There were no adverse events leading to trial or drug discontinuation. Four serious adverse events (viral myocarditis, diverticulitis, dyspnea, and vestibular neuronitis) resolved.
Conclusions: In this small trial, fazirsiran was associated with a strong reduction of Z-AAT concentrations in the serum and liver and concurrent improvements in liver enzyme concentrations.
(6). Bartley P. Griffith, et al. Genetically Modified Porcine-to-Human Cardiac Xenotransplantation. 2022.
Summary
A 57-year-old man with nonischemic cardiomyopathy who was dependent on venoarterial extracorporeal membrane oxygenation (ECMO) and was not a candidate for standard therapeutics, including a traditional allograft, received a heart from a genetically modified pig source animal that had 10 individual gene edits. Immunosuppression was based on CD40 blockade. The patient was weaned from ECMO, and the xenograft functioned normally without apparent rejection. Sudden diastolic thickening and failure of the xenograft occurred on day 49 after transplantation, and life support was withdrawn on day 60. On autopsy, the xenograft was found to be edematous, having nearly doubled in weight. Histologic examination revealed scattered myocyte necrosis, interstitial edema, and red-cell extravasation, without evidence of microvascular thrombosis – findings that were not consistent with typical rejection. Studies are under way to identify the mechanisms responsible for these changes. (Funded by the University of Maryland Medical Center and School of Medicine.)
(7). Andrea Cercek, et al. PD-1 Blockade in Mismatch Repair-Deficient, Locally Advanced Rectal Cancer. N Engl J Med. 2022;386:2363-76.
Abstract
Background: Neoadjuvant chemotherapy and radiation followed by surgical resection of the rectum is a standard treatment for locally advanced rectal cancer. A subset of rectal cancer is caused by a deficiency in mismatch repair. Because mismatch repair-deficient colorectal cancer is responsive to programmed death 1 (PD-1) blockade in the context of metastatic disease, it was hypothesized that checkpoint blockade could be effective in patients with mismatch repair-deficient, locally advanced rectal cancer.
Methods: We initiated a prospective phase 2 study in which single-agent dostarlimab, an anti-PD-1 monoclonal antibody, was administered every 3 weeks for 6 months in patients with mismatch repair-deficient stage II or III rectal adenocarcinoma. This treatment was to be followed by standard chemoradiotherapy and surgery. Patients who had a clinical complete response after completion of dostarlimab therapy would proceed without chemoradiotherapy and surgery. The primary end points are sustained clinical complete response 12 months after completion of dostarlimab therapy or pathological complete response after completion of dostarlimab therapy with or without chemoradiotherapy and overall response to neoadjuvant dostarlimab therapy with or without chemoradiotherapy.
Results: A total of 12 patients have completed treatment with dostarlimab and have undergone at least 6 months of follow-up. All 12 patients (100%; 95% confidence interval, 74 to 100) had a clinical complete response, with no evidence of tumor on magnetic resonance imaging, 18F-fluorodeoxyglucose-positron-emission tomography, endoscopic evaluation, digital rectal examination, or biopsy. At the time of this report, no patients had received chemoradiotherapy or undergone surgery, and no cases of progression or recurrence had been reported during follow-up (range, 6 to 25 months). No adverse events of grade 3 or higher have been reported.
Conclusions: Mismatch repair-deficient, locally advanced rectal cancer was highly sensitive to single-agent PD-1 blockade. Longer follow-up is needed to assess the duration of response.
(8). Akhaddar, et al. Chalk-Stick Fracture. 2022.
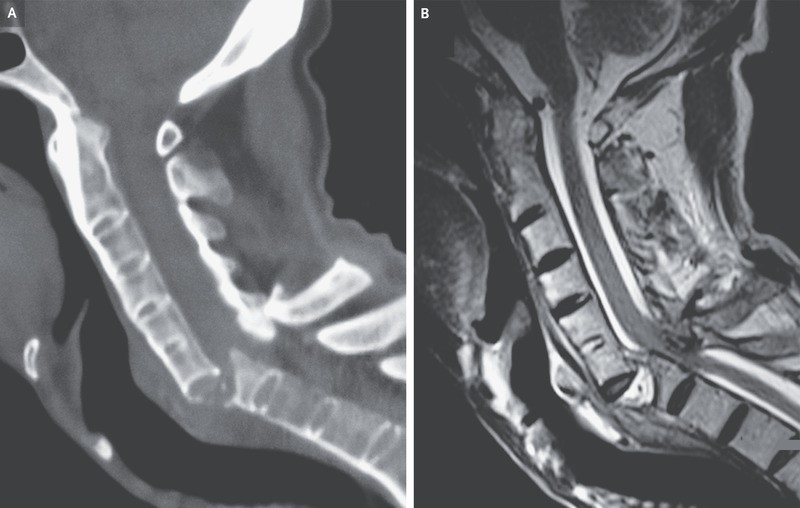
A 60-year-old man with a history of ankylosing spondylitis presented to the emergency department with neck pain and paralysis of the arms and legs after a fall. During the previous 5 years, he had not received treatment for the ankylosing spondylitis. At presentation, the blood pressure was 80/40 mm Hg and the heart rate was 56 beats per minute. Findings on physical examination were consistent with acute compression of the lower cervical spinal cord. Vasopressors were infused to treat neurogenic shock, and bladder catheterization was performed to treat acute urinary retention. Computed tomography of the cervical spine showed fused vertebrae with a displaced fracture – also known as a chalk-stick fracture – at the level of C6-C7 (Panel A). Magnetic resonance imaging of the cervical spine confirmed spinal cord compression at that level (Panel B). Ankylosis of the vertebrae results in increased bone fragility and risk of pathologic fracture. Neck or back pain after even minor trauma should prompt cross-sectional imaging to evaluate for serious injury. Surgical decompression and fusion of the spine were performed. Postoperatively, the patient regained function of his upper limbs but died from pneumonia 5 weeks later.
(9). Chris Stokel-Walker. How long does SARS-CoV-2 stay in the body? BMJ. 2022;377:o1555
What happens to SARS-CoV-2 when it enters the body, and how long does it linger? Nearly three years since the virus was first discovered, this is still a mystery. Chris Stokel-Walker asks what science has learnt so far
How long does SARS-CoV-2 stay in the body?
There is no definitive answer. The reality of 6.2 million deaths with covid-19 means that many people die from the effects of the virus within their body before the virus itself does, so it’s difficult to know how long they would have continued to shed the virus if they’d survived.
Also, different people clear viruses quicker than others, depending on underlying health conditions. For example, says Paul Hunter, professor in medicine at the University of East Anglia, “Even before covid, we’ve known that people who have certain immune deficiencies can struggle to clear viruses.”
What are the longest bouts of covid-19 infection recorded to date?
One patient tested positive for covid-19 for 505 days until they died, according to a case presented at the European Congress of Clinical Microbiology and Infectious Diseases in April 2022. Another report by Spanish researchers describes a 52 year old man undergoing chemotherapy who was still shedding virus after 189 days. Elsewhere, Chinese researchers reported a 64 year old man shedding the virus for 169 days after infection
That’s all recorded through the mouth and nose-which is normal for a respiratory virus. But what’s unusual with SARS-CoV-2 is where else in the body it has been showing up, and for how long.
Two studies found that the virus was present in a patient’s faeces seven months after diagnosis, indicating that the virus stays in the body longer than first thought. It creates a conundrum for researchers, who are now probing the potential links between SARS-CoV-2 in the gut and long covid.
A meta-analysis looking at the amount of time those infected with SARS-CoV-2 continue to shed the virus found that the average person continued to shed for roughly a month. Some people, however, are super shedders, with prolonged release of virus from their bodies. One 22 year old healthcare worker, for example, was continuing to shed the virus 110 days after infection.
Where does the virus persist?
As indicated above, it doesn’t just stay lodged in the respiratory tract-autopsies have found traces in the appendix eyes, heart, and brain. However, those traces have not been infectious, says Nathan Bartlett, associate professor in viral immunology at the University of Newcastle, Australia. “No one has actually isolated infectious virus from tissues outside of the respiratory tract,” he says. “There is no evidence-and people have looked very hard for infectious virus persisting outside it.”
Even in the respiratory tract, the virus is often not infectious. One autopsy by Italian researchers of an exhumed patient who died from covid found traces of the viral gene targets in her lungs and heart a month after her death, but the virus itself was not alive-which would be expected, as the virus relies on live cells. Maria Grazia Cusi, associate professor in the virology unit of the University of Siena, who conducted the study, says she found the presence of the bionucleic acids in the lung and the heart. “It was interesting to see the organs were still conserved in a good way,” she says, expressing amazement that the viral RNA could exist for so long within a dead body. (That said, traces of avian influenza have been shown to last up to 240 days at room temperature.)
“The behaviour of SARS-CoV-2 is strange,” says Cusi. “It’s difficult to understand how this virus can stay in the body for so long.”
Does SARS-CoV-2 stay in the body longer than other infections, like the flu and colds?
All three are RNA viruses, but covid-19 appears to stay in the body for longer than either influenza or the common cold. Cusi says SARS-CoV-2 appears to burrow itself in parts of the body that are difficult for the immune system to reach.
In influenza viruses there is the acute phase of the disease, then the clearance of the virus from the body-usually within days or weeks. For SARS-CoV-2, the number of variants makes it more difficult to say definitively how long it lasts, but it appears to persist for far longer.
Does the length of time the virus stays in the body increase the risk of long covid?
“We don’t really understand that link,” says Bartlett. It’s something that has been suggested in academic literature, but hasn’t been definitively proven. “It’s conceivable that if there are pockets of viral RNA that are making a little bit of viral protein, that could be triggering localised immune responses,” he says. That could make inflammation which, if it happens in the body’s central nervous system, could develop symptoms like brain fog and fatigue. There is research that shows a rise in antibody titres after patients begin symptoms, Bartlett says, however, that the numbers involved are quite low. “One needs to be cautious,” he advises.
Hunter says that while it’s plausible that there’s a link between the length of time the virus stays in the body and the risk of contracting long covid, caution must be taken when talking about post-infection syndromes. After all, long covid is not a single condition but a term encompassing a wide range of symptoms that last for more than 12 weeks after infection and are believed to have been triggered by the novel coronavirus.
For some people who caught covid, there is almost certainly some residual damage to the gas exchange membranes in the lung, or microvascular damage that affects cognition in the brain-both of which have been cited as problems for those with long covid. For others this may not be the case.
(10). Sohil Pothiawala. Not all post-traumatic swellings are haematomas: be alert to a Morel-Lavallée lesion. Lancet 2022;400(10345).
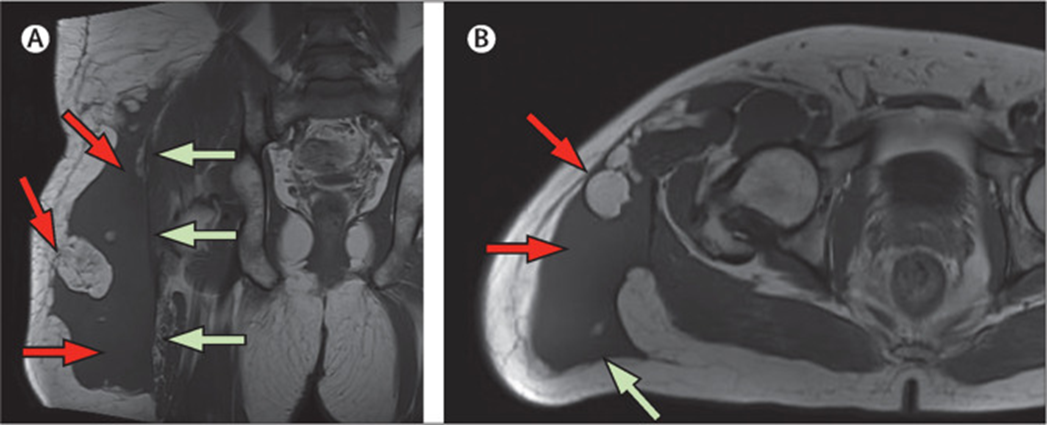
A 34-year-old man was brought to our Emergency Department after a truck ran over the right side of his body while he was out walking. He had no medical history.
On examination, the patient’s vital signs were stable; he had tenderness over his right shoulder, mild tenderness and bruising over the right hip, and abrasions over the right side of his arm, chest, abdomen, and right flank. His pelvis was stable, and movements of the right hip joint were unaffected.
Laboratory investigations were within normal range. No fractures were seen on x-rays of the patient’s chest, pelvis, right shoulder, and right femur. A whole-body CT scan showed subcutaneous haematomas about 3.5 cmx3.0 cm in the right infra-axillary region, right lateral abdominal wall, and pelvis.
We admitted the patient under the trauma service; an MRI of his right shoulder showed an acute contusion of the right supraspinatus muscle and right acromioclavicular joint. The patient was allowed home after an orthopaedic review with a plan of conservative treatment: analgesia and outpatient physiotherapy.
At follow-up with his general practitioner, 3 weeks later, the patient had an ill-defined soft, fluctuant swelling over his right flank and a fluctuant, non-tender swelling around the right hip with no abnormalities of the overlying skin.
At further assessment, 5 weeks after the accident, the swelling over the patient’s right flank had resolved, but the one over his right hip area had grown larger. An MRI of the right hip showed a large 14 cmx9.5 cmx26 cm fluid signal collection with multiple fat locules within the deep subcutaneous tissue of the right posterolateral proximal thigh and hip, immediately superficial to the intact deep fascia (figure). The findings were consistent with a diagnosis of a Morel-Lavallée lesion.
(11). The virtual wards aiming to ease hospital pressures. BMJ 2022;378:o1603.
Health services in England have been tasked with treating more patients at home, to cope with growing demand for beds.
In some NHS Hospitals every specialty is being encouraged to create its own virtual ward, a system whereby a patient can avoid time in hospital by being monitored or cared for at home.
“The model for our [virtual] ward here was that this was to be an extension of the hospital,” says a medical lead of virtual wards. “The aim was to completely mirror a hospital ward as much as possible, with a view to-now and in the future-it becoming a part of hospital life.” The number of virtual wards is set to grow.
Frailty and acute respiratory infection virtual wards take priority in the UK.
(12). Urs Fischer, et al. Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: an open-label, blinded-outcome, randomised non-inferiority trial. Lancet 2022;400(10346):P104-115.
Summary
Background: Whether thrombectomy alone is equally as effective as intravenous alteplase plus thrombectomy remains controversial. We aimed to determine whether thrombectomy alone would be non-inferior to intravenous alteplase plus thrombectomy in patients presenting with acute ischaemic stroke.
Methods: In this multicentre, randomised, open-label, blinded-outcome trial in Europe and Canada, we recruited patients with stroke due to large vessel occlusion confirmed with CT or magnetic resonance angiography admitted to endovascular centres. Patients were randomly assigned (1:1) via a centralised web server using a deterministic minimisation method to receive stent-retriever thrombectomy alone or intravenous alteplase plus stent-retriever thrombectomy. In both groups, thrombectomy was initiated as fast as possible with any commercially available Solitaire stent-retriever revascularisation device (Medtronic, Irvine, CA, USA). In the combined treatment group, intravenous alteplase (0.9 mg/kg bodyweight, maximum dose 90 mg per patient) was administered as early as possible after randomisation for 60 min with 10% of the calculated dose given as an initial bolus. Personnel assessing the primary outcome were masked to group allocation; patients and treating physicians were not. The primary binary outcome was a score of 2 or less on the modified Rankin scale at 90 days. We assessed the non-inferiority of thrombectomy alone versus intravenous alteplase plus thrombectomy in all randomly assigned and consenting patients using the one-sided lower 95% confidence limit of the Mantel-Haenszel risk difference, with a prespecified non-inferiority margin of 12%. The main safety endpoint was symptomatic intracranial haemorrhage assessed in all randomly assigned and consenting participants. This trial is registered with ClinicalTrials.gov, NCT03192332, and is closed to new participants.
Findings: Between Nov 29, 2017, and May 7, 2021, 5215 patients were screened and 423 were randomly assigned, of whom 408 (201 thrombectomy alone, 207 intravenous alteplase plus thrombectomy) were included in the primary efficacy analysis. A modified Rankin scale score of 0-2 at 90 days was reached by 114 (57%) of 201 patients assigned to thrombectomy alone and 135 (65%) of 207 patients assigned to intravenous alteplase plus thrombectomy (adjusted risk difference -7.3%, 95% CI -16.6 to 2.1, lower limit of one-sided 95% CI -15.1%, crossing the non-inferiority margin of -12%). Symptomatic intracranial haemorrhage occurred in five (2%) of 201 patients undergoing thrombectomy alone and seven (3%) of 202 patients receiving intravenous alteplase plus thrombectomy (risk difference -1.0%, 95% CI -4.8 to 2.7). Successful reperfusion was less common in patients assigned to thrombectomy alone (182 [91%] of 201 vs 199 [96%] of 207, risk difference -5.1%, 95% CI -10.2 to 0.0, p=0.047).
Interpretation: Thrombectomy alone was not shown to be non-inferior to intravenous alteplase plus thrombectomy and resulted in decreased reperfusion rates. These results do not support omitting intravenous alteplase before thrombectomy in eligible patients.
(13). Peter J Mitchell, et al. Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4.5 h of stroke onset: an open-label, blinded-endpoint, randomised non-inferiority trial. Lancet 2022;400(10346):P116-25.
Summary
Background: The benefit of combined treatment with intravenous thrombolysis before endovascular thrombectomy in patients with acute ischaemic stroke caused by large vessel occlusion remains unclear. We hypothesised that the clinical outcomes of patients with stroke with large vessel occlusion treated with direct endovascular thrombectomy within 4.5 h would be non-inferior compared with the outcomes of those treated with standard bridging therapy (intravenous thrombolysis before endovascular thrombectomy).
DIRECT-SAFE was an international, multicentre, prospective, randomised, open-label, blinded-endpoint trial. Adult patients with stroke and large vessel occlusion in the intracranial internal carotid artery, middle cerebral artery (M1 or M2), or basilar artery, confirmed by non-contrast CT and vascular imaging, and who presented within 4.5 h of stroke onset were recruited from 25 acute-care hospitals in Australia, New Zealand, China, and Vietnam. Eligible patients were randomly assigned (1:1) via a web-based, computer-generated randomisation procedure stratified by site of baseline arterial occlusion and by geographic region to direct endovascular thrombectomy or bridging therapy. Patients assigned to bridging therapy received intravenous thrombolytic (alteplase or tenecteplase) as per standard care at each site; endovascular thrombectomy was also per standard of care, using the Trevo device (Stryker Neurovascular, Fremont, CA, USA) as first-line intervention. Personnel assessing outcomes were masked to group allocation; patients and treating physicians were not. The primary efficacy endpoint was functional independence defined as modified Rankin Scale score 0-2 or return to baseline at 90 days, with a non-inferiority margin of -0.1, analysed by intention to treat (including all randomly assigned and consenting patients) and per protocol. The intention-to-treat population was included in the safety analyses. The trial is registered with ClinicalTrials.gov, NCT03494920, and is closed to new participants.
Findings: Between June 2, 2018, and July 8, 2021, 295 patients were randomly assigned to direct endovascular thrombectomy (n=148) or bridging therapy (n=147). Functional independence occurred in 80 (55%) of 146 patients in the direct thrombectomy group and 89 (61%) of 147 patients in the bridging therapy group (intention-to-treat risk difference -0.051, two-sided 95% CI -0.160 to 0.059; per-protocol risk difference -0.062, two-sided 95% CI -0.173 to 0.049). Safety outcomes were similar between groups, with symptomatic intracerebral haemorrhage occurring in two (1%) of 146 patients in the direct group and one (1%) of 147 patients in the bridging group (adjusted odds ratio 1.70, 95% CI 0.22-13.04) and death in 22 (15%) of 146 patients in the direct group and 24 (16%) of 147 patients in the bridging group (adjusted odds ratio 0.92, 95% CI 0.46-1.84).
Interpretation: We did not show non-inferiority of direct endovascular thrombectomy compared with bridging therapy. The additional information from our study should inform guidelines to recommend bridging therapy as standard treatment.
(14). Pierre Galere and Allison Gilbert. Eosinophilic gastroenteritis with ascites: an enigmatic diagnosis. Lancet 2022;400(10346):P126.
A 41-year-old woman presented to the emergency department with a 1-month history of worsening abdominal pain, nausea, and vomiting. The patient gave no history of recent travel, previous abdominal surgery, or adverse reactions to any allergens. She had no past medical problems. However, 2 days before we saw her, the patient had a gastrointestinal endoscopy which found no abnormalities; gastroduodenal and colonic mucosal biopsies had also been reported as healthy.
On examination we found the patient to be generally well; heart rate was 92 beats per min, blood pressure 110/60 mm Hg, oxygen saturation 98%. She was afebrile. Her abdomen was tender and distended with bulging flanks and shifting dullness: indicative of ascites.
Laboratory investigations showed leukocytosis (19.54×109 per L; normal 4.5-11.0) associated with a significant eosinophilia of 8.94×109 per L (normal 0-0.5), a raised IgE concentration (208 IU/mL; normal 1.5-144), and a slightly elevated C-reactive protein concentration (43 mg/L; normal <3.1). CA125 concentration was elevated (83 units/mL; normal 0-35); no other tumour marker was positive. Serum tryptase concentration was normal and tests screening for autoimmune diseases-including antinuclear antibodies for systemic lupus erythematosus or scleroderma-found nothing abnormal.
A CT scan excluded any visceral lesions. A diagnostic paracentesis showed eosinophilic ascites (figure). Blood, stool, and ascites analyses, including specific serological examinations and cultures, excluded viral, bacterial, and parasitic infections. That some parasitic infections, such as Strongyloides stercoralis, can be hard to diagnose based on one stool sample, led us to do repeated parasitological examinations of different stool samples, which all showed no positive results.
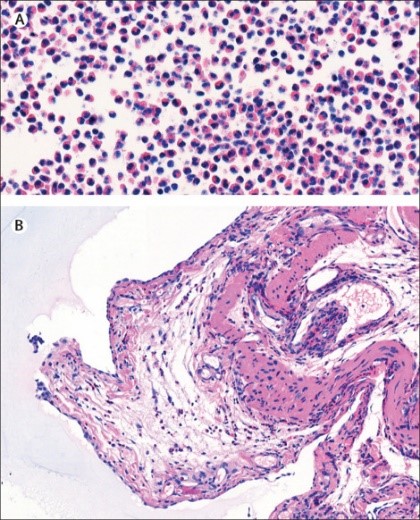
Lymphocytic and myeloproliferative forms of hypereosinophilic syndrome were excluded: a bone marrow biopsy showed no abnormalities. Using RT-PCR, no FIP1L1-PDGFRA fusion gene was found, and T-cell-receptor gene rearrangement testing of the patient’s peripheral blood was negative. A QuantiFERON-TB test was also negative.
We suspected a case of eosinophilic gastroenteritis, but to rule out any intra-abdominal neoplasm and to collect biopsies from the caecum serosa, we did a laparoscopy. Histopathological analysis of biopsy specimens confirmed our suspicions: significant eosinophilic infiltration with greater than 20 eosinophiles per high-power field; the small vessels were not involved, ruling out an associated vasculitis (figure). The patient was started on oral methylprednisolone and her symptoms rapidly improved; the serum eosinophilia returned to a typical level.
Three patterns of eosinophilic gastroenteritis are described: mucosal, mural, and serosal. Diagnosis of the serosal form is often considered a challenge as clinical and radiological presentations can be atypical. Likewise, histological findings can be misleading, as mucosal biopsies in the serosal form of eosinophilic gastroenteritis may appear normal, unlike those of the serosal layers which can confirm the diagnosis.
The diagnosis is usually made based on the combined biological, radiological, and histological findings. Finally, a good response to oral corticosteroids-as happened in our patient-adds weight to making a correct diagnosis of eosinophilic gastroenteritis.
(15). Tiernan Surlis, et al. Infantile haemangiomas. BMJ. 2022;378:e068734.
What you need to know
Most infantile haemangiomas are small, harmless, and resolve without treatment
Treatment is indicated for lesions that have potential to cause functional impairment (to vision, breathing, feeding, or by compression of internal organs), ulceration, or cosmetic disfigurement
Refer children with high risk haemangiomas promptly, as most rapid growth occurs in the first two months of life
Oral propranolol is recommended to treat problematic infantile haemangiomas
Infantile haemangiomas are the commonest vascular tumour of childhood. They occur in 5% to 10% of babies.1 Most require no treatment; however, referral to secondary care may be indicated depending on the clinical scenario. This article offers an approach to assessing a child with an infantile haemangioma in primary care.
Characteristics
Infantile haemangiomas generally follow a very predictable course. They are usually not present at birth (although precursor lesions may be present), and develop in the first weeks of life.2 Lesions grow rapidly in the first three months of life, especially at 5-8 weeks. Growth is usually complete by time the infant is 6 months. This is followed by a plateau period of no growth and then gradual involution usually after the child is 1. Most haemangiomas will have completed regression by the time the child is 4. Deep haemangiomas, however, may have a prolonged growth phase and take longer to regress.23 Infantile haemangiomas occur more frequently in female and premature infants, and those of low birth weight (<1 kg).234 The risk is increased during pregnancy in women who have pre-eclampsia, advanced maternal age, multiple gestation pregnancies, progesterone therapy in pregnancy, amniocentesis, and chorionic villus sampling.567891011
Most infantile haemangiomas are small and harmless, but approximately 11% have some complications, including functional impairment, cosmetic disfigurement, and potentially serious visceral abnormalities
(16). Stephen H Bradley et al. Investigating suspected lung cancer in primary care. BMJ 2022;378:e068384.
What you need to know
Up to a quarter of lung cancers are diagnosed in people who have never smoked
Consider chest radiography and urgent specialist referral or advice for unusual presentations that are not explicitly listed in local referral pathways
Unexplained haemoptysis warrants urgent referral (within 14 days) for computed tomography imaging
Inform patients when you anticipate that negative radiography and/or blood tests might provide insufficient reassurance to exclude lung cancer/other serious illness and advise that further investigations may be needed.
Globally, an estimated 10-25% of lung cancer cases occur in people who have never smoked; additionally, if lung cancer in non-smokers were considered a separate disease, estimates suggest that it would be the seventh most prevalent cancer worldwide. Nonetheless, increasing age and tobacco exposure are still the most important risk factors, and lung cancer (irrespective of smoking status) is the leading cause of cancer death worldwide.
Outcome is closely correlated to stage at diagnosis, but the high prevalence of common lung cancer symptoms (such as cough) presenting in primary care can make timely diagnosis difficult
(17). Valentijn M T de Jong, et al. Clinical prediction models for mortality in patients with covid-19. BMJ 2022;378.
Abstract
Objective: To externally validate various prognostic models and scoring rules for predicting short term mortality in patients admitted to hospital for covid-19.
Design: Two stage individual participant data meta-analysis.
Setting: Secondary and tertiary care.
Participants: 46914 patients across 18 countries, admitted to a hospital with polymerase chain reaction confirmed covid-19 from November 2019 to April 2021
Conclusion: The prognostic value of the included models varied greatly between the data sources. Although the Knight 4C Mortality Score and Wang clinical model appeared most promising, recalibration (intercept and slope updates) is needed before implementation in routine care.
Covid-19 has had a major impact on global health and continues to disrupt healthcare systems and social life. Millions of deaths have been reported worldwide since the start of the pandemic in 2019.1 Although vaccines are now widely deployed, the incidence of SARS-CoV-2 infection and the burden of covid-19 remain extremely high. Many countries do not have adequate resources to effectively implement vaccination strategies. Also, the timing and sequence of vaccination schedules are still debatable, and virus mutations could yet hamper the future effectiveness of vaccines.2
Covid-19 is a clinically heterogeneous disease of varying severity and prognosis.3 Risk stratification tools have been developed to target prevention and management or treatment strategies, or both, for people at highest risk of a poor outcome.4 Risk stratification can be improved by the estimation of the absolute risk of unfavourable outcomes in individual patients. This involves the implementation of prediction models that combine information from multiple variables (predictors). Predicting the risk of mortality with covid-19 could help to identify those patients who require the most urgent help or those who would benefit most from treatment. This would facilitate the efficient use of limited medical resources, and reduce the impact on the healthcare system-especially intensive care units. Furthermore, if a patient’s risk of a poor outcome is known at hospital admission, predicting the risk of mortality could help with planning the use of scarce resources. In a living systematic review (update 3, 12 January 2021; www.covprecise.org), 39 prognostic models for predicting short term (mostly in-hospital) mortality in patients with a diagnosis of covid-19 have been identified.5
Despite many ongoing efforts to develop covid-19 related prediction models, evidence on their performance when validated in external cohorts or countries is largely unknown. Prediction models often perform worse than anticipated and are prone to poor calibration when applied to new individuals.678 Clinical implementation of poorly performing models leads to incorrect predictions and could lead to unnecessary interventions, or to the withholding of important interventions. Both result in potential harm to patients and inappropriate use of medical resources. Therefore, prediction models should always be externally validated before clinical implementation.9 These validation studies are performed to quantify the performance of a prediction model across different settings and populations and can thus be used to identify the potential usefulness and effectiveness of these models for medical decision making.78101112 We performed a large scale international individual participant data meta-analysis to externally validate the most promising prognostic models for predicting short term mortality in patients admitted to hospital with covid-19.
(18). Helen Saul. People of all ages benefit from drugs to lower blood pressure. BMJ 2022;378.
People of all ages who have even slightly raised blood pressure should be offered treatment with antihypertensive drugs (to lower blood pressure). New research found that the drugs reduce the risk of cardiovascular events, such as heart attack or stroke, in all ages up to 85. The trend continued in the over 85s but was less certain because there were fewer people of this age in the study.
High blood pressure (hypertension) is common. In the UK and Europe, the treatment target (the blood pressure level that treatment aims for) is higher in older age groups. Before this review, it was uncertain whether people over 70 benefit from starting, or continuing, with antihypertensives if their blood pressure is not markedly high.
This large analysis investigated whether antihypertensives protect against cardiovascular diseases in adults of different ages. Researchers pooled data from studies including more than 350,000 people, and found that these drugs reduced the risk of cardiovascular events – regardless of age – in people with blood pressure that was even slightly raised.
The review concluded that antihypertensives benefit adults of all ages with even slightly raised blood pressure. Age-based thresholds should be removed from European and UK guidance, the researchers say. However, more research is needed in people over 85.
What’s the issue?
High blood pressure increases the risk of cardiovascular events such as stroke and heart attack. Drugs that lower blood pressure (antihypertensives) reduce the risk. Around 1 in 3 adults in the UK has high blood pressure. Many are unaware of their condition because symptoms are rarely noticeable; most people only find out when they have their blood pressure checked.
Ideal blood pressure is generally between 90/60 and 120/80 mmHg. The higher number (systolic pressure) is the force at which the heart pumps blood around the body – and is the number considered in this research. The lower number (diastolic pressure) is the resistance to blood flow in the vessels.
Different age groups have different blood pressure targets. For example, UK guidance recommends treatment for people older than 80 years only if they have markedly increased blood pressure, of 150/90 mmHg or higher.
Researchers showed recently that even small reductions (of 5 mmHg) in systolic blood pressure reduced cardiovascular risk, regardless of whether blood pressure was normal or high. In this analysis, the same team explored whether antihypertensive drugs protect against cardiovascular diseases in people of all ages.
What’s new?
Data was collected from more than 50 studies that randomly allocated people to receive various antihypertensive treatments or dummy (placebo). The studies included 358,707 people aged 21 – 105 (65 years on average).
The researchers looked at people’s age and their blood pressure (which ranged from less than 120/70 mmHg to 170/110 mmHg) at the beginning of a study. They looked at the link with cardiovascular events (stroke, heart attack, heart disease or heart failure) and whether the person died.
The researchers found that, in all age groups, reducing blood pressure reduced cardiovascular events. The reductions did not depend on blood pressure before treatment. Whatever the initial blood pressure, the risk of cardiovascular events was reduced as the systolic blood pressure was lowered.
For each 5 mmHg reduction in systolic blood pressure, cardiovascular events were reduced by:
18% in the under 55s
9% in groups aged 55-64, 65-74, and 75-84 years
1% in those aged 85 and older.
These figures show that the percentage reduction in cardiovascular events was highest in the under 55s. But these events are rare in younger people, which means this percentage reduction translates into fewer events prevented. Older people are generally at higher risk of cardiovascular events. With 4 years’ treatment (on average) in this analysis, despite the smaller percentage reduction, more events were prevented in older people.
Why is this important?
Experts around the world disagree on whether people over 70 should be prescribed antihypertensives. Guidelines differ; in Europe blood pressure targets vary by age, while in the United States, they do not. This research shows that age should not determine whether treatment with antihypertensives is started.
The researchers say that antihypertensives are effective into old age. Currently, blood pressure of 120/80 mmHg is considered normal. This analysis suggests that anyone whose blood pressure is above 120/70 mmHg should consider treatmentto reduce their cardiovascular risk. Age-related blood pressure thresholds should be removed from guidelines, the researchers say. As long as the drugs are well tolerated, older people should take them to prevent cardiovascular events.
Cardiovascular events are more common in older people. This means that, even though reducing blood pressure in older people prevented a smaller fraction of events, more were prevented in older than in younger people.
What’s next?
This study included fewer over 85s than in the younger age groups. The findings suggest that people over 85 with slightly raised blood pressure also benefit from antihypertensives but the evidence in this age group is less robust.
More research is needed in people aged 85 and older, the researchers say, and in some other groups such as people with multiple long-term conditions, and those who are frail. These populations could respond differently to antihypertensives or have different risks of cardiovascular events.
The researchers hope that their work will be used as a basis for discussion around whether people should take antihypertensives. They hope that UK guidance will change in the next few years to reflect their findings.
(19). The video game prescribed by doctors to treat ADHD.
https://www.bbc.com/news/business-62060542
While many parents worry that their children spend too much time playing computer games, Kelcey Sihanourath is pleased to see her son Owain pick up his tablet.
Now aged 13, he was diagnosed with ADHD (attention deficit hyperactivity disorder) in pre-school.
Since then, the family, who live in the US city of Savannah, Georgia, have taken Owain to see occupational therapists to help him better cope with everyday life tasks.
They also tried the medication route, but had to stop after the prescribed drugs exacerbated the boy’s regular migraines, and made him sick.
With ADHD continuing to affect Owain’s school performance over the years, Kelcey says she was “hoping for something more, for any other option”.
“I could see him struggling to understand why he was not able to focus, and the frustration he had when he tried so hard and would still get distracted,” she says. “It broke my heart, but I felt trapped and completely useless.”
Help came in the end from what initially seems very incongruous – a computer game called EndeavorRx.
In 2020 it became the first such game to be approved by the US Food and Drug Administration (FDA) for use in the treatment of ADHD in children.
Currently only available on prescription from doctors in the US, EndeavorRx at first glance looks very similar to countless other games. You control a little alien that races on a spaceship through different worlds having to collect things.
But the app-based game was developed in conjunction with neuroscientists, and is designed to stimulate and improve areas of the brain that play a key role in attention function.
The idea is that it trains a child with ADHD to both better multitask and ignore distractions, with a computer algorithm measuring his or her performance and customising the difficulty of the game in real time.
When doctors prescribe it, the child’s parents get sent an activation link that is needed before the game will play.
Kelcey says she was “a little sceptical”, but at the end of 2020 Owain started a three-month programme, playing the game for 25 minutes a day. He then did another round last year.
“He admitted it was a little harder than he expected,” she says. “But he understood that he was doing it to help improve his focus. He remained super motivated despite the difficulties and frustrations that came along with it.”
After each of Owain’s sessions she noted his daily behaviour in the app, and tracked his progress.
Soon she started to see small, positive changes in his behaviour. For example, getting ready for school had become smoother, and there were no negative messages from teachers.
And after failing fifth grade, Owain subsequently shot up to getting As and Bs for his work.
“It has been amazing to see my son so successful, but more so, seeing him have confidence in himself,” Kelcey says. “He is no longer upset and confused about why he just does not get it.”
Eddie Martucci, chief executive of Akili, the Boston-based tech firm behind EndeavorRx, says the game has been designed to boost cognitive progressing.
“It is something that’s very difficult to get through molecular means, like taking a pill. But it turns out that sensory stimuli can actually directly stimulate parts of the brain controlling cognitive function.”
His company now plans to launch the game in Europe in the next few years.
In London, UK app Thymia is using computer games to help doctors and other medical professionals detect and diagnose mental health issues, particularly depression.
One game sees the user have to try to memorise moving objects, while another is a card game that also tests his or her memory.
In addition to how well the patient performs in the game, their comments and facial expressions are also monitored and evaluated by the app, which accesses their computer or mobile phone’s camera and microphone.
Thymia has been launched by Dr Emilia Molimpakis, who has a doctorate in linguistics, cognitive neuroscience and experimental psychology from University College London (UCL). She runs the business with co-founder Dr Stefano Goria, who has a doctorate in theoretical physics from the University of Turin.
Dr Goria says the app “gathers and extracts biomarkers that are relevant for understanding depression symptoms… in a useable and engaging way”.
Both Akili and Thymia say that their apps should be used in addition to existing doctor-led monitoring and treatments, and not as a replacement. UK-based adolescent psychologist Angela Karanja agrees.
“While these are… effective inventions, they should be used alongside current existing [patient evaluation] questionnaires, which have been tested and accepted for reliability and validity, as well as doctors’ input, and also alongside other treatments, not in isolation,” says Ms Karanja.
Fellow UK psychologist Lee Chambers says that while the use of such video games in the diagnosis, monitoring and treatment of mental health conditions is still in the early stages, it appears to have “potential”.
“Engaging with a game has the ability to remove aspects of feeling like we are being tested and measured,” he says. “These types of mental health games have an ability to widen access, and track variations in the baseline data that they collect over time.
“Given this, it has the potential to be an early indicator and show patterns in a way we don’t currently have access to.”
(20). Tim Sanborn. Passing the Stethoscope. JAMA Cardiol. 2022;7(7):665-666.
Tim, I’m feeling very short of breath. Can you get your stethoscope and listen to my lungs?”
This was the appeal from my father one evening while we were watching television after dinner. At the time, I was a first-year medical student and was just learning physical diagnosis. My father’s request led to an experience I will never forget.
When I was growing up, I remember my father being a very driven, extremely hard-working general surgeon. He would often tell my siblings and me stories of how he grew up in the Great Depression and worked 3 jobs to put himself through college and medical school. For his room, he was responsible for keeping coal burning in the furnace. For his books, he worked in the library. For his meals, he served food at a sorority house. Besides studying and working hard, dad would also tell us stories of how he kept himself in good shape, running track and playing football.
To support our family in his solo practice, he put in long days and nights sharing emergency department surgical call 24/7 at several hospitals. In an era before cell phones, on the occasions when our parents went to a friend’s house for dinner, they would leave a telephone number with us so we could contact Dad if a hospital called. All too often, he would need to break off these evenings with friends to head to the hospital. Despite this hectic work schedule, he would always strive to be present for our family dinners. There, he would instill his work ethic in all of us. On rare instances, he would lighten up with a big smile on his face and share a joke that he heard from one of his patients. For the most part, however, he was extremely devoted to his work and never complained about the long hours he spent caring for patients. Considering my father’s usual stoic demeanor, his plea for help immediately set off an alarm. I was worried and sensed that something serious must be causing my father’s difficulty breathing.
Dad had recently been discharged from the hospital after having a partial gastrectomy to remove the upper portion of his stomach that contained a bleeding ulcer near the junction with his esophagus. In the early 1970s, this surgery was the standard treatment for uncontrolled gastric bleeding. This was before the use of proton pump inhibitors to reduce gastric acid secretion and erosion of the stomach lining or the use of a flexible endoscope to clip and stop the bleeding. Concerned for my father’s health and anxious to demonstrate what I had learned in my physical diagnosis class, I quickly complied and went to get my black bag.
After recently retiring from surgical practice, my father had passed on his black bag to me so that I could use it in my introduction to physical diagnosis class. This well-worn, 40-year-old black bag had lost some of its luster on the seams since my father’s medical school days in the 1930s. Inside, however, it contained a Littmann stethoscope, a Welch Allyn ophthalmoscope and otoscope kit, a portable blood pressure cuff, tuning fork, reflex hammer, and other first aid items neatly arranged in an orderly manner. Like the microscope my father also passed on to me for my histology class, this black bag was now serving a second-generation physician.
As I proudly retrieved what was now my stethoscope, I asked my father to remove his shirt so I could listen to his lungs more clearly. As he struggled to remove his arms from the sleeves of his shirt owing to discomfort from his surgical incision, I noticed the pale, pallor of his skin and a recently stapled, well-healed, midline abdominal scar running from his breastbone to his navel. I asked myself whether my father was anemic from postoperative blood loss. Was anemia the cause of his shortness of breath?
Up until this time, I had only listened to audio cassette tape recordings of normal and abnormal heart and lung sounds in our physical diagnosis class and had the opportunity to examine the lungs of only a few patients in the hospital under the mentorship of one of our internists. It was no wonder that I approached this examination with a feeling of trepidation and anxiety. Here I was, a novice in performing a physical examination and using a stethoscope, examining my own father who was experiencing significant respiratory distress after major surgery!
With his shirt removed, I observed my father in respiratory distress using rapid, shallow breaths while sitting on the couch. Examining his lungs on his right side, I moved the stethoscope from the upper lung fields all the way down to his diaphragm along his hunched-over back. I was pleased that I could detect breath sounds, loud and clear, throughout his entire right lung. I wondered if my father was limited in his ability to take a deep breath from the pain of his recent surgery. Moving to his left side, however, I quickly noticed-for the first time in my limited clinical experience-that his breath sounds were completely absent on the lower half of his left lung. As a newly taught, diligent medical student, I next tested for dullness to percussion by tapping 1 finger on another moving down my father’s back. Once again, I was shocked to hear-for the first time-a lack of drumlike resonance and a flat dullness when I percussed the lower half of his left lung. Earlier in the month, I heard the harsh, crackling sounds of pneumonia on a patient during physical diagnosis rounds. This was the very first time I had heard the lack of breath sounds and dullness to percussion on a real live patient.
Hearing stories from my father’s surgical experience, I knew bleeding was a known complication of gastric surgery. With my findings on his lung examination, I now thought to myself that my father’s respiratory distress must be due to fluid accumulation in his lower left lung. Was this fluid due to a hemothorax, postoperative bleeding into his left pleural space from an operation near the junction of his stomach and his esophagus? If so, this must be serious! My mother and I quickly helped my father get into the car and drove him to the hospital.
Looking back on this experience, I remember the satisfaction I felt when my dad’s intern showed me my father’s chest radiograph, which confirmed what I had suspected. There was opacification of his left lung field due to fluid filling up the entire lower left half of my father’s chest. To relieve my father’s symptoms of shortness of breath, the intern told me this fluid needed to be removed. Later, when I checked on my father, the intern described how the pulmonologist used a needle and a catheter to perform a thoracentesis and drain a liter of blood from the left side of my father’s chest.
I still recall the intern congratulating me with a smile for making the clinical diagnosis of a postoperative hemothorax using my stethoscope. This compliment gave me a great sense of pride and confidence at this early stage of my medical training. Little did the intern realize, it was my father’s stethoscope, passed on to me, that helped make the diagnosis.
As caring physicians, we always strive to teach the next generation of physicians and other health care professionals. Remembering this sequence of events from many years ago, I now wonder, did my father, as a surgeon himself, suspect all along what was causing his difficulty breathing? Was he testing me to see if I could demonstrate what I had learned in physical diagnosis class and confirm his suspicion?
This incident also brought home to me how my father, in his own nurturing way, had the confidence and trust in me to examine him, listen to his lungs, and diagnose what was causing his breathing problem. Like the track athlete my father was in school, dad was now passing the baton, or in his case, passing the stethoscope to me.
(21). Stephen Holgate. Air pollution is a public health emergency. BMJ 2022;378:o1664.
Summary
Air pollution continues to be a major and growing public health challenge.
However, it is invisible to the eye. Air pollution today comes from many sources, one important source is traffic
Fine particulate matter (PM2.5) passes through the lungs into the circulation along with toxic gases such as NO2, and together these initiate, accelerate, and exacerbate non-communicable diseases.
The contribution of air pollution to non-communicable diseases has greatly increased, while also having a negative effect on pregnancy outcomes and early life development.
Greater efforts to reduce this key driver of adverse health are needed.
PM2.5 is undoubtedly an invisible killer, but its effects are clear to see: increased risk of asthma attacks on high pollution days and more hospital admissions for heart and lung diseases.
Polluted air triggers strokes and heart attacks, exacerbates respiratory illnesses, such as chronic obstructive pulmonary disease, and can stunt children’s lung growth.
The result is not just premature deaths, but more years spent in ill health, and more avoidable pressure on the health system.
Air pollution, both outside and indoors, is a major driver of health inequalities, with the most deprived communities more likely to live in polluted areas.
The adverse effects of air pollution on health are not being sufficiently communicated to patients and their carers by medical and nursing professionals.
Conversations to help patients understand how pollution might worsen health or exacerbate their conditions are vital.
There are key touch points-during asthma assessments and reviews, in cardiovascular and maternity checks-for these conversations to take place. But do healthcare professionals know enough about air pollution and its impacts?
Health professionals need to be confident to have these conversations.
All health professionals have an important role in understanding the serious adverse effects of air pollution and communicating them clearly and effectively to patients at risk. Equally importantly, they can be influential advocates for cleaner air and can push for government intervention to achieve that.
Air pollution is one of the greatest environmental and public health threats of our time. Government must commit to reducing PM2.5 to 10μg/m3 by 2030, with the ultimate objective of reducing annual mean concentration to 5μg/m-3 in line with the latest WHO health based air quality guideline values.Nations’ health depends on it.
(22). Roshini Claire Anthony. Dulaglutide: A new horizon for T2D treatment in the very young. 2022.
https://specialty.mims.com/topic/dulaglutide–a-new-horizon-for-t2d-treatment-in-kids
A once-weekly subcutaneous dose of the GLP-1* receptor agonist dulaglutide successfully controlled glycaemic levels in youths with type 2 diabetes (T2D) being treated with lifestyle modification with or without metformin or insulin, results of the multinational, phase III AWARD-PEDS** study showed.
“These findings are a potential breakthrough in the paediatric diabetes space and can help address the unmet need for additional treatments available to young people with diabetes, particularly pharmacotherapeutic options,” said Professor Silva Arslanian, director at the Center for Pediatric Research in Obesity and Metabolism, University of Pittsburgh, UPMC Children’s Hospital of Pittsburgh, Pittsburgh, Pennsylvania, US, who presented the results at ADA 2022.
Participants were 154 individuals aged 10 to <18 years (mean age 14.5 years, 71 percent female) with BMI >85th percentile*** (mean 34.1 kg/m2) and T2D (HbA1C >6.5 to ≤9 or ≤11 percent#; mean 8.1 percent) treated with lifestyle modification with/without metformin or basal insulin. They were randomized, double-blind, 1:1:1 to receive subcutaneous dulaglutide (1.5 mg or 0.75 mg) or placebo once weekly for 26 weeks. Patients in the placebo group then received dulaglutide 0.75 mg/week in a 26-week open-label extension study, while those initially randomized to dulaglutide continued their assigned trial medications (n=139). Self-monitoring of blood glucose levels was done at fasting state and again at another time point and when experiencing hypoglycaemia symptoms.
At 26 weeks, dulaglutide was superior to placebo, with a significant reduction in mean HbA1c levels from baseline in the pooled dulaglutide group compared with an increase in the placebo group (least squares [LS] mean change -0.8 vs 0.6 percentage points; p<0.001). [ADA 2022, abstract 5-LB; N Engl J Med 2022;doi:10.1056/NEJMoa2204601]
The HbA1c benefits with dulaglutide were consistent across multiple subgroups including age, sex, race, ethnicity, diabetes duration or medication use, baseline HbA1c, BMI, and body weight.
While the glycaemic control benefits with dulaglutide were observed through 52 weeks, the authors noted an increase in HbA1c during the open-label phase which they suggested could be attributed to “rapid underlying disease progression” in this age group.
More patients on dulaglutide than placebo achieved HbA1c <7 percent at 26 weeks (51 percent vs 14 percent; p<0.001). Fasting plasma glucose levels increased from baseline in the placebo group (LS mean change 17.1 mg/dL) and decreased in the dulaglutide groups (LS mean change -18.9 mg/dL; p<0.001).
The change in BMI from baseline was comparable between the dulaglutide and placebo groups (LS mean change -0.1 vs 0 kg/m2; p=0.55). There were no significant differences in the change from baseline in body weight or waist circumference within each group.
This contrasts with the weight loss effects of dulaglutide at these same doses in adults with T2D, the reason for which remains uncertain, the authors said.
At week 26, mean total and low-density lipoprotein cholesterol and serum triglyceride concentrations increased in the placebo group and decreased in the dulaglutide groups. However, changes in blood pressure and heart rate from baseline did not differ between the dulaglutide and placebo groups.
No additional safety concerns
Adverse events (AEs) at 26 weeks occurred in 69, 75, and 73 percent of placebo, dulaglutide 0.75 mg, and dulaglutide 1.5 mg recipients, respectively, and serious AEs in 6, 2, and 2 percent, respectively. One patient each in the placebo and dulaglutide 0.75 mg group and two in the dulaglutide 1.5 mg group experienced an AE leading to treatment discontinuation.
Gastrointestinal (GI) events were among the most common AEs in the first 26 weeks, affecting more dulaglutide than placebo recipients, though 80, 69, and 89 percent of nausea, vomiting, and diarrhoea cases in the dulaglutide groups were mild. Most cases also occurred in the first 2 weeks of dulaglutide treatment. There was one GI event-related discontinuation in the dulaglutide 1.5 mg group. Allergy or hypersensitivity incidence was similar across groups (n=2, 3, and 2 in the placebo, dulaglutide 0.75 mg, and dulaglutide 1.5 mg groups, respectively), as were injection-site reactions (n=5, 5, and 4, respectively).
Hypoglycaemia incidence was also comparable across groups, with no severe hypoglycaemia events. More placebo than dulaglutide recipients received rescue medication for persistent hyperglycaemia in the first 26 weeks (18, 4, and 2 percent in the placebo, dulaglutide 0.75 mg, and dulaglutide 1.5 mg groups, respectively). There were no pancreatitis or thyroid neoplasms.
“Overall, most AEs were reported during the first 26 weeks, with a similar AE profile through 52 weeks,” the authors noted. The safety profile in this population was consistent with that in adults and there were no deaths during the trial.
A step forward for long-term treatment
While adults with T2D have a wide range of therapeutic options, the choices are limited for youths. Moreover, younger patients with T2D have greater severity of insulin resistance and β-cell dysfunction and high therapeutic failure rates with metformin, the authors pointed out.
“We are encouraged by the strong HbA1c improvements achieved and are hopeful that a [once/weekly] medication could be a step forward for how young people are treated,” stated Arslanian.
If approved for use in youths, in addition to the benefits on glycaemic control, dulaglutide also offers a convenient mode and frequency of administration which is particularly important for long-term 24. treatment of T2D in this population, said the authors.
(23). Emily Claire Rudd. Facial lymphoedema, viral warts, and myelodysplastic syndrome: the protean condition of GATA2 deficiency. Lancet 2022;400(10347):P236.
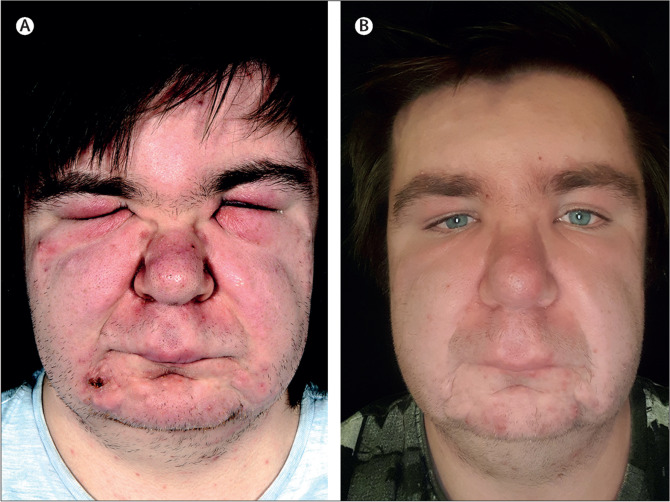
A 17-year-old man reporting a 3-year history of an acneiform eruption and a 4-month history of worsening swelling of his face, was referred to our specialist joint haematology-dermatology clinic. The patient had been found to have a monocytopenia of 0.2×109 per L (normal 0.2-1.0); he had no other past medical problems.
On examination he was generally well and vital signs were within normal limits. He had inflammatory papules and pustules without comedones on both cheeks, forehead, and chin. He also had severe facial lymphoedema extending from the jawline to the anterior hairline with debilitating periorbital swelling that limited eye opening (figure). Additionally, numerous cutaneous viral warts were noted on his hands and knees.
Laboratory investigations showed mild macrocytosis and the monocytopenia: haemoglobin concentration was 150 g/L (normal 130-165), mean corpuscular volume 99.7 fL (normal 77-95), neutrophils 3.08×109 per L (normal 2.2-6.3), platelets 180×109 per L (normal 150-450). Thyroid function, anti-nuclear antibodies, immunoglobulins, and inflammatory markers were unremarkable.
Histopathological analysis of samples of skin biopsies from the chin and lower eyelid showed superficial and deep perifollicular and periadenexal lymphocytic inflammation as well as ectatic blood vessels in the superficial dermis: indicative of the clinical diagnosis of rosacea. No organisms were seen on periodic-acid-Schiff with diastase, Grocott, and Ziehl-Neelsen stains. Prolonged tissue culture did not isolate bacteria, mycobacterium, or fungi.
Notably, the patient had a family history of both myelodysplastic syndrome (MDS) and acute myeloid leukaemia (AML): his mother was diagnosed with MDS aged 27 years, AML aged 36 years, and she died aged 37 years; a maternal aunt was diagnosed with MDS aged 26 years and had an allogeneic transplant; his maternal grandmother was diagnosed with AML aged 24 and died one year later; and a maternal great aunt, who was diagnosed at an unknown age, with AML.
Putting the findings together-monocytopenia, human papilloma viral infection, lymphoedema, and family history of myelodysplastic syndromes-we suspected the patient had GATA2 deficiency.
Bone marrow studies confirmed MDS: refractory cytopenia of multilineage dysplasia and normal cytogenetics. Genetic testing showed a heterozygous pathogenic GATA2 variant (c.1061 C>T; p.Thr354Met).
The patient was started on low dose oral isotretinoin, vigilant monitoring of his full blood count, and regular manual lymphatic drainage of his face which after one year had significantly improved the rosacea and lymphoedema (figure). The response was sustained 2 years after completion of the therapy.
GATA2 is a zinc finger transcription factor required for haematopoiesis and lymphatic angiogenesis; several pathogenic mutations leading to GATA2 deficiency have been described. The syndrome segregates as an autosomal dominant trait with incomplete penetrance. Clinical manifestations are heterogeneous, and patients usually present in adolescence or early adulthood. Cutaneous infections, panniculitis, and lymphoedema in the setting of cytopenia, especially monocytopenia, should trigger suspicion of GATA2 deficiency. Lymphoedema associated with GATA2 deficiency is usually confined to the lower limbs and genitalia-known as Emberger syndrome-and marked facial lymphoedema, as seen in our patient, has not previously been reported. Most patients with GATA2 haploinsufficiency develop myeloid neoplasms before the age of 50 years and may require haematopoietic stem-cell transplantation which can be curative.
(24). Myrto T Samara. What is the right drug for insomnia disorder? Lancet 2022;400(10347):P139-141.
Cognitive behavioural therapy (CBT) is considered a first-line treatment for chronic insomnia disorder;1 nevertheless, few clinicians are trained to deliver this treatment, and exploring other options seems imperative. In The Lancet, Franco De Crescenzo and colleagues2 report a large and comprehensive data synthesis on pharmacological treatments for insomnia disorder in which they assessed 154 double-blind trials of 30 different drugs or placebo with 44089 adult participants (mean age 51.7 [SD 12.2] years, 62.8% women), conducted across a range of international settings. They included almost all available medications as monotherapy, licensed or not, and analysed a substantial number of outcomes for the acute (preferably at 4 weeks) but also long-term (>3 months) treatment of insomnia. Most trials were placebo-controlled; thus comparative efficacy between competing treatments was assessed through network meta-analysis that synthesises both direct and indirect evidence, resulting in more precise estimates. The study produced drug hierarchies for sleep quality, subjective total sleep time, and other efficacy outcomes.
The result that benzodiazepines were the most effective treatments for the short term was not surprising; unfortunately, no data were available for the long-term treatment, but we should keep in mind the well recognised potential for misuse and dependence.3 Moreover, this class of psychotropic drugs was shown to cause more side-effects than placebo at the study endpoint.2 Except for zaleplon, the so-called Z-drugs-namely, zopiclone, eszopiclone, and zolpidem-were shown to be effective for insomnia disorder and, although initially thought a safe alternative to benzodiazepines, were also not free from safety concerns2 and seem to share a similar risk of misuse and dependence.3 Dual orexin receptor antagonists constitute a newer class of sleep drugs that includes daridorexant, lemborexant, seltorexant, and suvorexant. Lemborexant and seltorexant were shown to improve sleep quality with no more side-effects than placebo.2
Concerns over the possible side-effects of benzodiazepines and Z-drugs have led to frequent off-patent use of other agents such as antidepressants, antipsychotics, and antihistamines. Given the complex relationship between other psychiatric disorders and insomnia, antidepressants or antipsychotics might represent a reasonable choice, especially for a group of patients with concurrent psychiatric symptoms. Nevertheless, for these drugs, data were too scarce to guide clinical practice and more research is warranted before safe conclusions are made.
Several other issues limit the robustness of the findings. Long-term data were available for few drugs. Based on a maximum of nine studies, network plots were not so well connected, which casts doubts on the transitivity assumption, and specific side-effects were not reported consistently in original studies. Currently there is a gap of evidence for these important outcomes; thus, the Article2 provided information mainly about the short-term comparative efficacy and tolerability of drug treatments. Furthermore, insomnia is a cross-diagnosis symptom, and the evidence of this study cannot be directly applied to all patients or specific age groups (eg, children or older adults) and treatment-resistant cases. For example, De Crescenzo and colleagues2 did not find melatonin effective, but this drug has shown some positive results in older adults (aged 65 or older)4 and, in its prolonged-release formulation, is approved by the European Medicines Agency in adults aged 55 years or older. Melatonin is also the only drug currently available for insomnia in children and adolescents with autism spectrum disorders. Furthermore, as in other psychiatric disorders,5 publication year might have biased the efficacy results by favouring older drugs. Benzodiazepines were compared in older trials (median publication year 1990), followed by Z-drugs (median 2003), and then dual orexin receptor antagonists (median 2017), which was the same as the order if ranked for sleep quality. Older trials might show exaggerated results due to poorer quality of randomisation or blinding and publication bias. Another explanation could be that design characteristics of modern, industry-sponsored trials lead to increased placebo response rates and decreased effect sizes.5
Non-pharmacological treatments, such as CBT, lifestyle modifications, exercise or dietary interventions, and their combinations with pharmacotherapy were not included. A recently published comprehensive overview of systematic reviews compared the effectiveness and safety of pharmacological and non-pharmacological interventions for insomnia disorder.6 This study confirmed that CBT is a first-line treatment because of its consistent and robust evidence of effectiveness across many outcomes, as well as the fact that it is expected to have few or no major side-effects. Thus, pharmacological interventions for insomnia could be considered as second-line treatments.6
De Crescenzo and colleagues,2 have succeeded in depicting all available evidence in sleep medications for insomnia disorder; they concluded that eszopiclone and lemborexant had the best profile, although might cause substantial adverse events. Data on most other drugs, longer-term data, and data for side-effects were sparse. In future research, other sources of evidence, especially about the side-effect profiles of these medications, should be considered. Moreover, trials with a duration longer than 3 months that directly compare active drug treatments and non-pharmacological interventions are warranted to provide clear answers to clinicians and patients. For insomnia treatment, patient-physician shared decision making is crucial to decide when a pharmacological intervention is deemed necessary and which drug to be given by considering the trade-offs for efficacy and side-effects.
(25). Suzanne O’Sullivan. Navigating recovery: the healing power of patients’ narratives. Lancet 2022;400(10347):P154-155.
The Miskito are Indigenous people of Nicaragua. They come from the Mosquito coast where remote villages nestle between the Caribbean Sea and lush jungle. Their communities are affected by a disorder called grisi siknis that manifests as highly contagious convulsions. It predominantly affects young women and sweeps through villages in sporadic outbreaks. The Miskito believe that grisi siknis is caused by a spirit called the duende. Traditional healers cure it with ritual and herbal potions.
Krasnogorsk, a small town in Kazakhstan’s vast northern steppe that is now nearly deserted, is another place said to have a unique illness. Between 2010 and 2015 more than 130 residents fell into a prolonged sleep that could not be explained by medical testing. The local people attribute the outbreak to environmental poisoning, although there is no scientific evidence for that. The sleeping sickness only affects residents of Krasnogorsk. Even visitors who spend a long time in the region are not affected. Like grisi siknis, this illness has a cure. Residents who move away from Krasnogorsk usually recover.
Grisi siknis is well documented and listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition as a cultural concept of distress-a way in which a cultural group experience, understand, and communicate suffering and troubling emotions. Krasnogorsk’s sleeping sickness has been described as mass psychogenic illness, although it has never officially been given that label within Kazakhstan. In western biomedical taxonomy both disorders sit on a wide spectrum of conditions that are thought to arise through psychosomatic mechanisms.
In 2019 I visited these communities and gathered testimonials of local people’s experiences. I looked at their test results and watched videos of their seizures. What struck me most as I listened to the stories was how familiar they were to me. Dizziness, tiredness, stomach upset, and brain fog; lots of symptoms commonly described by patients I encounter who have psychosomatic and functional neurological disorders.
Watching videos of the seizures caused by grisi siknis, I saw the same dissociative (non-epileptic) seizures that I see in my neurology practice in London, UK. Of course, I should have expected these similarities. Biology and the physiological stress pathways are the same in everyone. Dissociation is a ubiquitous experience. The type of cognitive mistakes and prediction errors to which the brain is prone, and which lead to psychosomatic and functional symptoms, are the same whether you live in Nicaragua or Kazakhstan or the UK.
That is not to say that the Nicaraguan and Kazakhstani people’s stories were like my patients’ in every aspect. The Miskito live in a remote, rural location with limited access to health-care services. They are a deeply spiritual people who have a great respect for traditional healing methods.
Meanwhile, in post-Soviet era Krasnogorsk, many inhabitants’ homes do not have running water or heating. It was probably inevitable therefore that there were considerable differences in the way each group accounted for their symptoms. The Miskito blamed grisi siknis on an attack by a malign spirit. The people of Krasnogorsk held fast to a belief that the government was forcing them from their homes by deliberately poisoning the town. Then there is the matter of the high recovery rate for both groups. Traditional healers can cure most cases of grisi siknis. Similarly, the sleeping sickness in Krasnogorsk eventually abated. Everyone woke up and there have been no new cases since 2016. People with similar problems in high-income countries do not always fare so well. My patients with dissociative (non-epileptic) seizures only have about a 30% cure rate. Functional and psychosomatic symptoms of the severity of Krasnogorsk’s sleeping sickness often lead to chronic ill-health.
Medicine is a culture-bound practice. Societies explain bodily changes differently and subscribe to treatments that make sense within their belief systems. Everybody thinks their approach is the right one. So, is it possible that western medicine is so circumscribed by its convoluted classification systems, diagnostic categories, and technology that it cannot see where it could do better?
Observing how well these two communities negotiated their way from illness to full recovery was a stark reminder for me that the way a person explains and responds to psychosomatic illness can be fundamental to recovery. I was reminded that much of the research in psychological and psychosomatic illness is done on educated, affluent populations in industrialised countries. That means that the experiences of the vast majority of the world’s populations are not represented. By failing to give adequate heed to the work of sociologists and anthropologists who have long made this point, western medical practitioners could be missing out on vital perspectives.
Many name changes and waves of theories have swept through western biomedicine’s understanding of psychosomatic and functional neurological disorders. The concept of conversion disorder provided a psychodynamic explanation for this type of suffering and, as such, psychosomatic symptoms were treated by purely psychological interventions. That view is now considered reductionist. Psychological processes are functions of the brain, which means that all psychological, psychosomatic, and functional symptoms must come with corresponding brain changes. Brain-mind dualism is no longer tolerated. Labels like hysteria and psychosomatic have been replaced by the word functional to emphasise the biology rather than the psychology of the condition. But have these changes made people better? I would argue that they have benefited the few but not the majority. I fear that heavily medicalised formulations overlook the purpose that these disorders may serve and block a route to recovery. Explanations dependent on brain mechanisms draw attention away from patients’ social and environmental contexts.
One common cause for psychosomatic and functional neurological disorders is social stress. Grisi siknis is an example of this. It typically occurs due to psychogenic and social triggers with a common example being unwanted sexual attention directed at young women. Grisi siknis and its attribution to the duende is a sophisticated process used by the Miskito people to express distress and ask for help when faced by particular social pressures. It is effective because it elicits a community response and it is a story that comes with a prescribed treatment that points to recovery. Since the cause is external-the duende-the illness is not blamed on the individual. Grisi siknis is a language of distress understood by the people who speak that language.
The people of Krasnogorsk have a unique social history that is pertinent to the sleeping sickness. In Soviet times the uranium mines of the region gave the town a special status and relative affluence. The break-up of the Soviet Union had a devastating effect on the town. It lost its special status and its privileges. Over the following two decades buildings crumbled and amenities were withdrawn. Many people left, although some remained living there, perhaps with the hope that the mines would reopen and the place would return to its previous splendour. That did not happen. By 2010 few people remained, the population was getting old, and amenities were being withdrawn. I suggest that the sleeping sickness came to give the remaining residents the push that was needed to help them leave the beloved home that had once served them so well. The sleeping sickness served a social purpose. Neither of these groups were interested in a diagnosis of a psychosomatic disorder in either a psychologised or biologised form. They understood what was happening to them through a framework that made sense within their own social circumstance. They followed the narrative that they wrote around their symptoms to a place of recovery.
Sometimes functional neurological disorders and psychosomatic disorders evolve through the attention a person pays to their body, through a maladaptive response to injury, or through the unreliability of the unconscious mechanisms that the brain uses to make sense of a confusing world. But other times, psychosomatic symptoms are a signal to let us know that something in our life is not right. They are a means by which our body alerts us to the need to take a break or the need for help. Not every problem can be fixed with a list of pros and cons and not every problem is easy to meet head on. That is when psychosomatic disorders can be of value and when an overmedicalised explanation for them can be detrimental.
Western medical doctors like myself may be missing out on opportunities to help patients recover because we are so fixated on our own biomedical models and so reluctant to work with the formulations that patients use to explain their own suffering. Overly biological explanations for psychological and psychosomatic illness risk being fatalistic. They give a sense of permanency to symptoms, rob people of agency, and fail to address wider determinants of health and the need for social change. Psychological explanations can be problematic too. They often rely too heavily on the Freudian concept of hidden stress that needs only be forced out into the open for the problem to be cured. Such explanations are rejected because they are too confronting. Failing to appreciate the symptom as metaphor can mean failing to appreciate the problem the symptom has come to solve. It ignores the narrative that drives symptoms.
The Miskito and people in Krasnogorsk both did a much better job of approaching psychosomatic phenomena than I have ever done. The communities came together to support the affected individuals without judgement. They listened to the need the symptoms had come to address. Psychological and psychosomatic disorders in western medical formulations are more likely to lead to isolation. A doctor’s temptation to challenge a patient’s view of their own illness can force the patient to reinforce their symptoms. Western medicine’s diagnostic labels can result in embodiment of an illness identity from which people cannot recover. For all these reasons, western medicine might do well to look at the ways that other cultures approach such disorders.
If we could find a way to communicate through the patient’s narrative and rely less on the legitimising through biologising perhaps we could help patients navigate to recovery. But that would require considerable humility.
