Last on the list: A diagnosis seldom considered in males
Stephy George1, RM. Subbaiah2, G. Dominic Rodriguez3
1PG Resident, Kauvery Hospital, Tennur, Trichy, India
2General Physician, Kauvery Hospital, Tennur, Trichy, India
3Consultant Hemato Oncology, Kauvery Hospital, Tennur, Trichy, India
*Correspondence: domappa1966@gmail.com
Abstract
Autoimmune diseases are generally more common in women than men. Sex hormones, especially oestrogen (but also prolactin and testosterone), play important roles in these diseases. Oestrogens are generally considered to enhance autoimmunity and have multiple effects on the immune system through various cell types and molecular pathways. There is much evidence supporting the role of oestrogen in the pathogenesis of systemic lupus erythematosus (SLE); the disease occurs much more frequently in women, especially during the years of child-bearing potential, and commonly flares up during pregnancy. We report a case of SLE in a young male who presented with pyrexia of unknown origin.
Case Presentation
An 18-years-aged male presented with a two months history of pain in the joints, both small and large joints, predominantly involving knees, ankles, metatarsals, wrist, elbows, and proximal interphalangeal joints. He also had intermittent fever and loss of weight of about 7 kg over 2 months.
He was evaluated elsewhere, found to have leukopenia, thrombocytopenia, and raised ESR (40 mm/hr). Urine and blood cultures were sterile. Chikungunya IgM and IgG were negative. Dengue NS1 and IgM were negative. Echocardiogram was normal. HRCT of the thorax revealed subpleural ground-glass opacities in the right lower lobe. RT-PCR for COVID was negative. He was treated with hydroxychloroquine, doxycycline, and low-dose steroids and was discharged on day 4.
Despite steroids, he continued to have fever. He presented to our hospital 3 weeks later with a cough and severe pain in the right lower chest along with polyarthralgia and fever.
On evaluation, he had oral ulcers, bilateral submandibular, posterior cervical, axillary and inguinal lymphadenopathy. He also had a right pleural effusion.
Investigations revealed Hb, 13.5 g%; total count, 3900 cells/mm3 (polymorphs, 39%; lymphocytes, 34%; monocytes, 33%); platelet, 8000 cells/mm3; ESR, 11; Creatinine, 0.86; CRP-2.2. Uric acid, 6.3; total protein, 6.7 (albumin 3.3, globulin 3.4); unremarkable urine analysis. Ultrasound abdomen revealed mild splenomegaly, minimal ascites and bilateral mild pleural effusion.
We found a febrile young male with polyarthralgia, oral ulcers, bilateral pleural effusions with ascites, generalised lymphadenopathy with leukopenia and severe thrombocytopenia.
Our differential diagnoses were
- lymphoma
- leukaemia
- disseminated tuberculosis
- auto immune disorder
We proceeded with a lymph node biopsy and obtained urgent consultation from haematologist for severe bicytopenia. He observed that the peripheral smear did not suggest any malignancy. Urgent bone marrow assessment showed a reactive marrow with normal cell lines. No evidence of leukaemia or lymphoma in the marrow. Autoimmune workup was suggested by him. However, we waited for biopsy report for the final conclusion to exclude lymphoma.
RA factor (<10) and anti-CCP (0.54) were negative. C3 and C4 levels were low. ANA by immunofluorescence was strongly positive +++, speckled pattern. Antibodies to PCNA (proliferative cell nuclear antigen) and antimitochondrial antibody were positive. The direct coombs test was negative.
Diagnosis of Systemic Lupus Erythematosus was made. He fulfilled the 6/11 criteria (ACR 1997), for SLE (serositis, oral ulcers, arthralgia, blood abnormalities, ANA positivity, and immunological criteria (By 2019 EULAR/ ACR criteria he had a score of 26 points.)
He was started on corticosteroids. He improved well and was discharged with prednisolone 60 mg/day and hydroxychloroquine 400 mg/day.
Discussion
Systemic lupus erythematosus (SLE) is a prototypic autoimmune disease characterised by the production of antibodies to components of the cell nucleus in association with a diverse array of clinical manifestations. It is substantially more common in females of childbearing age, where the reported female: male ratio is 8-15:1. Prepubertal and postmenopausal ratios are much lower at 2-6:1 and 3-8:1 respectively [1,2].
Patients present with variable clinical features ranging from mild joint and skin involvement to life-threatening kidney, hematologic, or central nervous system involvement. The clinical heterogeneity of SLE and the lack of pathognomonic features or tests pose a diagnostic challenge for the clinician. To complicate matters, patients may present with only a few clinical features of SLE, which can resemble other autoimmune, infectious, or hematologic diseases.
The diagnosis of SLE has been dependent on criteria developed by ACR in 1982 and revised in 1997. This carried a sensitivity of 82.8% and specificity of 93.4% and almost every physician knows it by heart and applies the same at the bedside [3,4]. Over the years new criteria have emerged to obtain more specificity and sensitivity and also to make the diagnosis early [5]. The following Table 1 summarises the criteria.
Table 1. Single criteria in the four SLE classification criteria sets since 1982.
ACR 1982 | ACR 1997 | SLICC 2012 | EULAR/ACR 2019 | |
Mucocutaneous |
||||
1. Malar rash | 1. Acute cutaneous LE* | Acute cutaneous LE | 6 |
|
or SCLE | SCLE | 4 |
||
2. Discoid rash | 2. Chronic cutaneous LE* | Discoid LE | 4 |
|
3. Photosensitivity | ||||
4. Oral ulcers | 3. Oral ulcers | Oral ulcers | 2 |
|
or nasal ulcers | ||||
4. Non-scarring alopecia | Non-scarring alopecia | 2 |
||
5. Arthritis | 5. Synovitis | Joint involvement | 6 |
|
6. Serositis | 6. Serositis | Serosal |
||
a) Pleuritis | Pleuritis | Effusion | 5 |
|
b) Pericarditis | or pericarditis | Acute pericarditis | 6 |
|
7. Renal disorder | 7. Renal | Renal |
||
a) Persistent proteinuria | Proteinuria | Proteinuria | 4 |
|
b) Cellular casts | or red cell casts | |||
Histology compatible with lupus nephritis | ISN/RPS II/V | 8 |
||
ISN/RPS III/IV | 10 |
|||
8.Neurologic disorder | 8. Neurologic | Neuropsychiatric |
||
a) Seizures | Seizures | Seizure | 5 |
|
b) Psychosis | Psychosis | Psychosis | 3 |
|
Mononeuritis multiplex | ||||
Myelitis | ||||
Peripheral or cranial neuropathy | ||||
Acute confusional state | Delirium | 2 |
||
9. Hematologic disorder | Hematologic |
|||
a) Hemolytic anemia | 9. Hemolytic anemia | Coombs+ hemolytic anemia | 4 |
|
b) Leukopenia | 10. Leukopenia | Leukopenia | 3 |
|
c) Lymphopenia | or lymphopenia | |||
d) Thrombocytopenia | 11. Thrombocytopenia | Thrombocytopenia | 4 |
|
10. Immunologic disorder | ||||
a) LE cell preparation | ||||
SLE-specific antibodies |
||||
b) Anti-DNA | a) Anti-DNA | 12. Anti-dsDNA | Anti-dsDNA | 6 |
c) Anti-Sm | b) Anti-Sm | 13. Anti-Sm | Anti-Sm | 6 |
d) False-positive syphilis serology | c) Anti-phospholipid | 14. Anti-phospholipid | Anti-phospholipid | 2 |
15. Low complements | Low complement |
|||
C3 or C4 low | 3 |
|||
C3 and C4 low | 4 |
|||
16. Coombs test without hemolytic anemia | ||||
11. ANA | 11. ANA | 17. ANA | Entry criterion ANA |
|
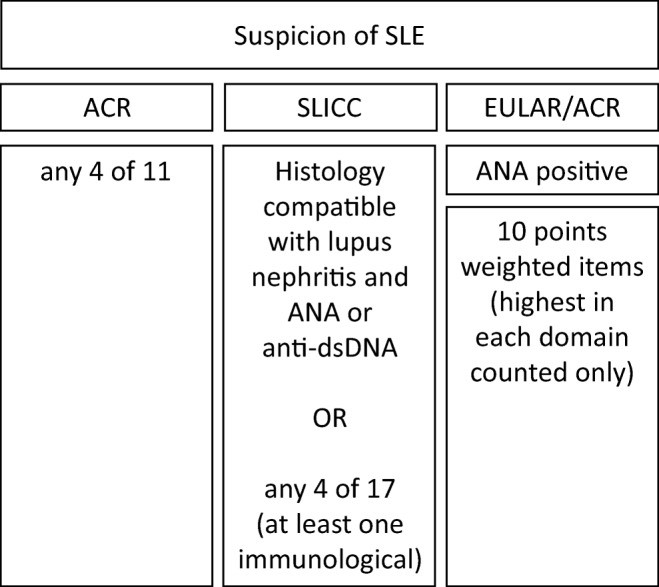
The criteria for the diagnosis of SLE have been built upon the original criteria developed by the ACR in 1982. Revisions of the original criteria have enabled a sensitivity of 94.1% and specificity of 97.4% (EULAR/ACR 2019).
Diagnostic criteria which are still used at the bedside and one that every physician knows goes by the mnemonic MD SOAP BRAIN – based on the older ACR criteria.
M-Malar rash; D- Discoid rash; S-Serositis; O-Oral ulcers; A-Arthralgia; P-Photosensitivity; B-Blood disorder; R-Renal involvement; A-ANA positivity; I-Immunological phenomena; N-Neurologic disorder.
The latest criteria require ANA positivity as an entry criterion plus 7 clinical and 3 immunological domains.
| Clinical domains | Immunological domains |
| 1. Constitutional | 1. ANA |
| 1. Hematological | 2. complement |
| 1. Neuropsychiatric | 3. SLE specific antibodies |
| 1. Mucocutaneous 2.Serosal 3. Musculoskeletal 4. Renal |
It is widely known that SLE is much more common in women than in men with a ratio close to 9:1 [6]. The increased frequency of SLE among women may be attributed to differences in the metabolism of sex hormones and/or GnRH [7].
SLE tends to run a more severe course in males than in females, with a worse prognosis [8]. Because of the predominance of women in most studies, little is known about the disease in men. Recent studies suggest that the impairment that occurs in older men has higher mortality in one year than women with SLE [9].
Table 2. SLE clinical phenotype differs between males and females
| Characteristic | Males | Females |
| Incidence [10] | Less compared to females | Higher in females of childbearing age with the ratio of 8-15:1 |
| Age of onset [11,12,13] | The mean age range was 26-38.4 years. | Median age range 26.3-31.9 years. |
| Clinical features [14,15,16] | Discoid rash, subacute cutaneous lesions, serositis more frequent. more severe renal involvement. | Arthritis, Raynaud's phenomenon, photosensitivity, malar rash, oral ulcers are more common |
| Neurologic manifestations [17] | More seizures and peripheral neuropathy | More neuropsychiatric manifestations and headaches |
| Hematologic manifestations [13,18] | More autoimmune hemolytic anemia and thrombocytopenia. lupus anticoagulant is more common. Thrombosis was more common. | More leukopenia |
| Flares [19] | Less frequent | More frequent |
| Relapses [19] | Less frequent | More frequent |
| Prognosis [9,20] | Worse prognosis. End organ damage is more common | Better prognosis than males. |
Conclusion
To conclude, the application of the old criteria is still practical at the bedside to make a diagnosis of SLE. The new criteria allow for an earlier diagnosis in certain situations.
There is a delay in the diagnosis of SLE in males because it is seldom considered in the differential diagnosis. A delay in diagnosis results in more organ damage.
SLE runs a more severe course in males. Partial treatment or steroid use without indications and a proper diagnosis, adds to the confusion and continued patient suffering.
Early diagnosis and disease categorization, patient education about the disease, and appropriate timely treatment are essential in treating all autoimmune disorders.
Reference
- Pons-Estel GJ, Wojdyla D, McGwin G Jr, et al. The American College of Rheumatology and the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus in two multiethnic cohorts: a commentary. Lupus 2014;23:3.
- Petri M, Orbai AM, Alarcón GS, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64:2677.
- Prete PE, Majlessi A, Gilman S, et al. Systemic lupus erythematosus in men: a retrospective analysis in a Veterans Administrations Healthcare System population. J Clin Rheum 2001;7:142-50.
- Lahita RG. The importance of estrogens in systemic lupus erythematosus. Clin Immunol Immunopathol. 1992;63:17-8.
- Aringer M, Luchten N, Johnson SR. New criteria for lupus. Curr Rheumatol Rep. 2020;22:18.
- Tan TC, Fang H, Magder L, et al. Differences between male and female systemic lupus erythematosus in a multiethnic population. J Rheumatol. 2012;39:759-69.
- Guillerimo J, Pons-Estel, Manual F, et al. Epidemiology of systemic LUPUS erythematosus. Exp Rev Clin Immunol. 13.8;799-814.
- Garcia MA, Marcos JC, Marcos AI, et al. Male systemic lupus erythematosus in a Latin-American inception cohort of 1214 patients. Lupus 2005;14:938-46.
- Murphy G, Isenberg D. Effect of gender on clinical presentation in systemic lupus erythematosus. Rheumatol. 2013;52:2108-15.
- Jacobsen S, Petersen J, Ullman S, et al. A multicentre study of 513 Danish patients with systemic lupus erythematosus. Disease manifestations and analyses of clinical subsets. Clin Rheumatol. 1998;17:468-77.
- Lu LJ, Wallace DJ, Ishimori ML, et al. Male systemic lupus erythematosus: a review of sex disparities in this disease. Lupus 2010;19:11929.
- Miller M, Urowitz M, Gladman D, et al. Systemic lupus erythematosus in males. Medicine 1983;62:32734.
- Mongkoltanatus J, Wangkaew S, Kasitanon N, et al. Clinical features of Thai male lupus:an age matched controlled study. Rheumatol Int. 2008;28:339-44.
- Sherif Z. Yacoub Wasef, gender medicine. 2004;1.
- Molina JF, Drenkard C, Molina J, et al. Systemic lupus erythematosus in males. A study of 107 Latin American patients. Medicine (Baltimore). 1996;75:124-30.
- Blum A, Rubinow A, Galun E. Predominance of renal involvement in male lupus with systemic lupus erythematosus. Clin Exp Rheumatol. 1991;9:206-7.
- Hochberg MC, Boyd RE, Ahearn JM, et al. Systemic lupus erythematosus: A review of clinico-laboratory features and immunogenetic markers in 150 patients with emphasis on demographic subsets. Medicine (Baltimore). 1985;64:285-95.
- Andrade R, Alarcon G, Fernandez M, et al. Accelerated damage accrual among men with systemic lupus erythematosus. XLIV. Results from a multiethnic US cohort. Arthritis Rheumatol. 2007;56:62230.
- Mok CC, Lau CS, Chan TM, et al. Clinical characteristics and outcome of southern Chinese males with systemic lupus erythematosus. Lupus. 1999;8:188-96.
- Wang YF, Xu YX, Tan Y, et al. Clinicopathological characteristics and outcomes of male lupus nephritis in China. Lupus 2012;21:147281.

Dr. Stephy George
PG Resident

Dr. R. M. Subbaih
Consultant Hemato Oncology

Dr. G. Dominic Rodriguez
General Physician
