Spontaneous Pneumomediastinum in COVID 19- Tertiary Care Centre Experience in South India
Saranya Manickavasagam1,*, Senthilvelmurugan1, Ivan Jones2, Dominic Rodriguez2
1Department of Diagnostic and Interventional Radiology, Kauvery Hospital, Trichy, Tamilnadu, India
2Department of Internal Medicine, Kauvery Hospital, Trichy, Tamilnadu, India
*Correspondence: drsaranyamvs@gmail.com
Abstract
Background: Radiological imaging plays a vital role not only in the diagnosis but also in the surveillance of patients and guides the physician in the management of patients with COVID-19 infection. The presence of spontaneous pneumomediastinum (SPM) among the varied presentations has been reported rarely as a case series. In this article, we reported our experience in spontaneous pneumomediastinum related to COVID-19 pneumonia.
Case presentation: This is a retrospective study of COVID-19 database in a single tertiary care center. The inclusion criteria were patients with pneumomediastinum at admission or who developed it subsequently during inpatient stay, with microbiological confirmation of COVID-19 by RT-PCR or documentation of COVID-19 pneumonia with CT scan and without invasive ventilation. Exclusion criteria were those who developed pneumomediastinum on invasive ventilation and those with isolated pneumothorax.
Conclusion: Developing spontaneous pneumomediastinum is a rare imaging finding in COVID-19 pneumonia. We would like to conclude that one has to be watchful for this complication during the third week of illness especially if there is a clinical worsening. Once developed it is a negative prognostic indicator with high mortality.
Keywords: Spontaneous pneumomediastinum, COVID-19
Background
The outbreak of novel coronavirus infection began in Wuhan, China in December 2019 [1]. Since then the infection has spread worldwide with more than 95 million people infected. Radiological imaging plays a vital role not only in the diagnosis but also in the surveillance of patients and guides the physician in the management of patients with COVID-19 infection [2]. The common radiological features of COVID 19 has been widely published in literature: Bilateral multifocal ground glass densities with peripheral distribution with or without consolidation, predominantly involving lower lobes and posterior segments, interlobular septal thickening and bronchiectasis. The presence of spontaneous pneumo-mediastinum (SPM) among the varied presentations has been reported rarely as a case series [3].
In this article, we would like to share our experience in spontaneous pneumomediastinum related to COVID 19 pneumonia.
Materials and methods:
This is a retrospective study of COVID-19 database in a single tertiary care center. The patients included in the study were admitted in Kauvery hospital, Trichy, India from the period of April 2020 to December 2020.The inclusion criteria was patients with pneumomediastinum at admission or who developed it subsequently during inpatient stay, with microbiological confirmation of COVID-19 by RT PCR or documentation of COVID-19 pneumonia with CT scan and without invasive ventilation. Exclusion Criteria were those who developed pneumomediastinum on invasive Ventilation and those with isolated pneumothorax. The demographic parameters included were age, gender, co-morbid conditions and smoking status. Symptoms such as fever, cough, dyspnea, myalgia and loss of smell were noted along with the date of onset of symptoms. Clinical parameters such as peripheral oxygen saturation (SPO2) and laboratory parameters of the patients like C-reactive protein, lactate dehydrogenase, ferritin, D-dimer and Interleukin -6 were also collected. Details about hospitalization including noninvasive ventilation (NIV) and invasive ventilation were obtained.
The chest radiographs and CT scans were done at varied intervals for the patients based on the clinical indications. The images were interpreted by Radiologists with more than 10 years of experience. The CT images were analyzed for the presence of spontaneous pneumomediastinum, spontaneous pneumothorax and subcutaneous emphysema. The extent and severity of the parenchymal changes were also noted before and at the time of development of spontaneous pneumomediastinum. Severity score was given based on the extent of lobar involvement of both lungs. Each segment was assigned a score of 0/1/2 based on the involvement of 0% / <50% / >50% of its area.
The demographic, clinical, laboratory and imaging features were formulated and provided in the table below (Table 1).
Table 1. Demographic,clinical,labaratory and imaging parameters of patient cohort.
Case No | Age/gender | Preexisting-Pulmonary disease | Co-morbid conditions | Smoking status | SPO2 at admission | Inflammatory markers LDH (U/L); CRP (mg/L); Ferritin (ng/ml) | CT severity score | Day of onset of SP | SPM/pneumothorax/SE |
1 | 56/Male | No | DM / HTN | Non smoker | 90% | LDH - 344 ; CRP - 18; Ferritin - 322 | 25/40 | 20 | SPM/ SE |
2 | 65/Male | No | DM / HTN | Non smoker | 86% | LDH - 221 ; CRP - 61 Ferritin - 350 | 37/40 | 19 | SPM/bilateral pneumothorax |
3 | 53/Male | Emphysema | DM / HTN | Smoker | 80% | LDH - 412 ; CRP - 68 Ferritin - 669 | 38/40 | 24 | SPM / SE |
4 | 59/Male | No | DM / HTN | Non smoker | 80% | LDH - 598; CRP - 9 Ferritin - 681 | 39/40 | 18 | SPM/SE/Right pneumothorax |
5 | 74/Male | No | HTN | Non smoker | 88% | LDH - 400 ; CRP - 35 Ferritin - 445 | 24/40 | 25 | SPM/ SE |
6 | 62/Male | No | DM / HTN | Non smoker | 80% | LDH -540 ; CRP - 30 Ferritin - 593 | 37/40 | 20 | SPM / SE |
7 | 67/Male | No | HTN | Non smoker | 84% | LDH - 674 ; CRP - 6 Ferritin - 110 | 38/40 | 27 | SPM |
8 | 63/Male | No | DM / HTN | Non smoker | 60% | LDH - 425 ; CRP - 63 Ferritin - 379 | 33/40 | 16 | SPM |
9 | 73/Female | No | DM / HTN | Non smoker | 82% | LDH - 463 ; CRP- 143 Ferritin - 405 | 30/40 | 17 | SPM |
10 | 58/Male | No | None | Non smoker | 84% | LDH - 425 ; CRP- 100 Ferritin - 513 | 30/40 | 20 | SPM / SE |
11 | 69/Male | No | DM/HTN | Non smoker | 90% | LDH - 400 ; CRP- 50 Ferritin - 763 | 25/40 | 24 | SPM |
Abbreviations: Spontaneous pneumomediastinum (SPM); spontaneous pneumothorax (SP);
Lactate dehydrogenase (LDH); C-reactive protein (CRP). Noninvasive ventilation (NIV).
 (a)
(a)
 (b)
(b)
 (c)
(c)
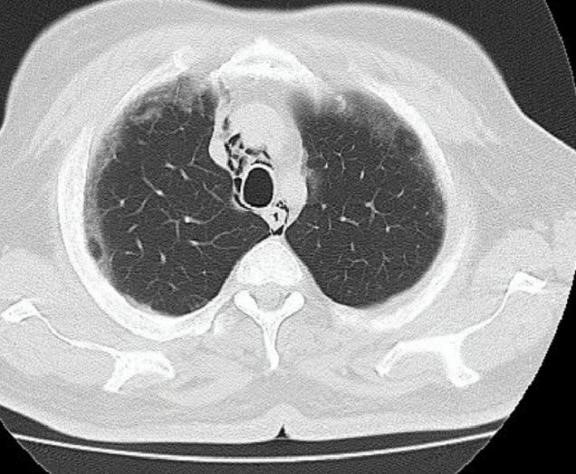
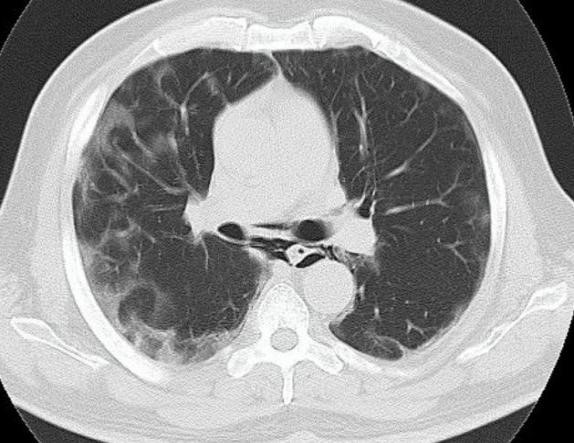
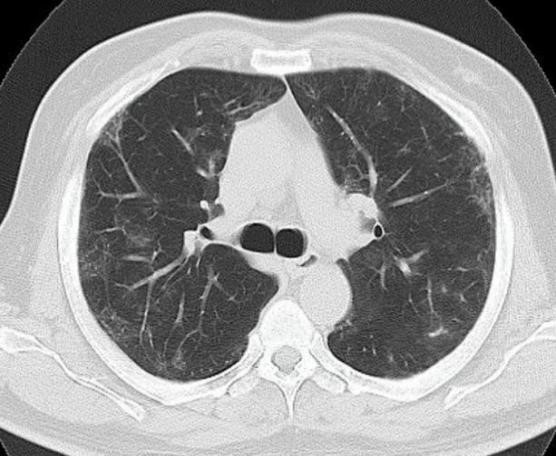
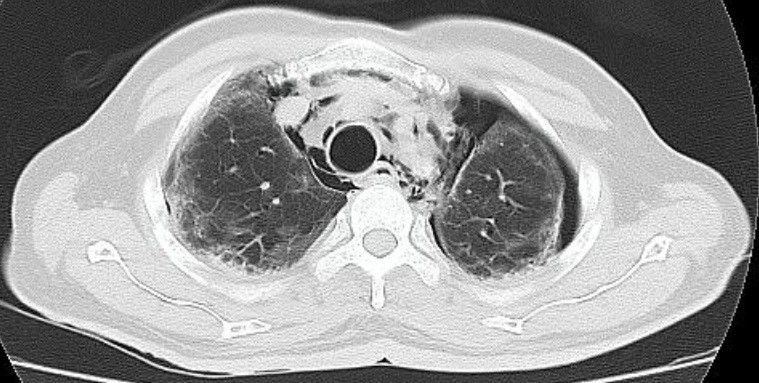
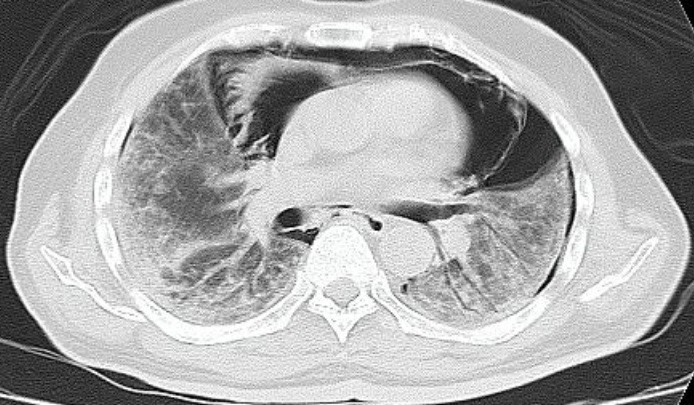
Fig. 1. Axial chest CT images of a 56-year-old male patient hospitalized for COVID-19 pneumonia. Fig. 1a and 1b showed mild pneumomediastinum along with ground glass densities in sub pleural regions of both lungs. Fig. 1c follow up image of the patient obtained 1 month later showed complete resolution of pneumomediastinum with patchy resolving ground glass densities in bilateral lungs.
Results:
2440 cases were admitted for COVID-19, out of which 11 patients were found to have spontaneous pneumomediastinum without invasive ventilation. 10 patients were male and 1 patient was female. Ten (90%) out of 11 patients had co-morbid conditions like diabetes mellitus, hypertension. Only one patient gave a history of smoking. All the patients presented with common manifestations like fever, cough, dyspnea while some had history of loss of smell and taste. Their mean SPO2 was 82%. Almost all had elevated inflammatory markers like C-reactive protein(CRP), Lactate dehyrogenase (LDH) and ferritin during their course of illness.
Out of the eleven cases of spontaneous pneumomediastinum (Fig. 1), six had concurrent subcutaneous emphysema, one had unilateral pneumothorax and one had bilateral pneumothorax. The onset of pneumomediastinum was between 16th to 25th day after the development of symptoms. Seven out of eleven patients were on non-invasive ventilation (BiPAP/CPAP) prior to the onset of spontaneous pneumomediastinum. Six (54.5%) patients succumbed to the infection during the period of their hospitalization. Those who survived didn’t have any sequelae secondary to spontaneous pneumomediastinum. Five patients got discharged and 4 patients on follow up are doing well clinically. One was lost to follow up. Only 2 patients underwent follow up CT chest which revealed complete resolution of spontaneous pneumomediastinum.
Selected cases
Case 1
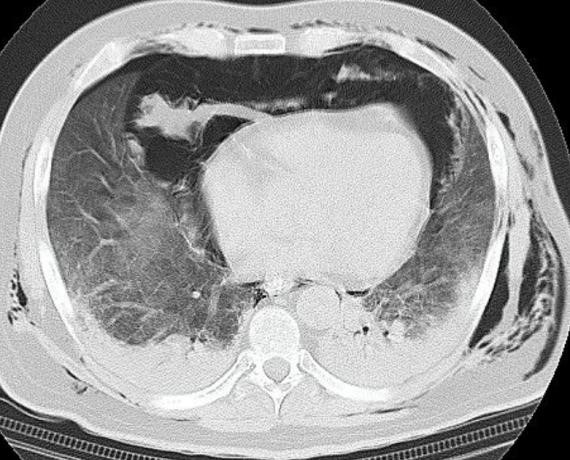
A 59-year-old patient who got admitted for the management of SARS-COVID. The patient had contact history with COVID-19 positive patient and had tested positive on the basis of RT PCR analysis. The patient was asymptomatic at the time of admission and his vitals were stable. Blood tests showed white cells count of 9000 with neutrophils 71% and lymphocytes 15% and Neutrophils/Lymphocytes ratio (NLR) 4.4. Non contrast chest CT showed focal ground glass density in the right upper lobe. He was treated according to our hospital protocol. The patient’s serum inflammatory markers gradually elevated along with increasing supplemental oxygen requirement. His Interleukin-6 was elevated. The patient shifted to was shifted to ICU and put on Noninvasive ventilation (NIV). As he developed chest pain and became acutely hypoxic, chest x-ray taken bedside and follow up CT chest done (Fig. 2) which showed extensive pneumomediastinum, subcutaneous emphysema along with mild right pneumothorax. There were diffuse ground glass densities with basal consolidation of bilateral lungs. The patient was intubated, ICD done on the right side and the he was closely monitored. In spite of the medical support, the patient succumbed to the infection the following day.
 (a)
(a)
 (b)
(b)
 (c)
(c)
 (d)
(d)
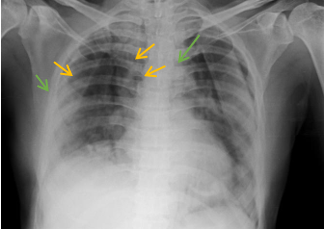
Fig. 2. Chest radiograph of a 59-year-old man admitted for COVID-19 who developed neck and chest swelling with worsening of dyspnea showed subcutaneous emphysema, pneumomediastinum (red arrows). Axial CT scan of the patient showed (a) extensive subcutaneous emphysema in lower neck and chest (b and c) pneumomediastinum with minimal right pneumothorax (yellow arrow) in addition to diffuse ground glass opacities with basal consolidation in both lungs.
Case 2
A 65-year-old man who was a known diabetic and hypertensive presented with the history of fever for 10 days, cough and dyspnea for 1 week. He has temperature of 99-degree F, respiratory rate of 26/min and his SPO2 was 92% in room air at the time of admission. His RT PCR status was positive. Initial CT chest showed bilateral patchy peripheral ground glass densities. The laboratory investigations showed elevated neutrophils, D-dimer, CRP (61 mg/L) and LDH (221 U/L). The patient was treated with hydroxychloroquine, steroids, antiviral, antibacterial drugs and anticoagulants. The patient was desaturating and hence shifted to Intensive care unit (ICU) and started on NRBM mask. In due course, the patient developed progressive respiratory failure and was put on Noninvasive ventilation (NIV). On day 22, his follow up CT chest showed bilateral extensive ground glass densities and mild pneumomediastinum. The patient was closely monitored. As there was increase in interleukin-6 (>65.2), a provisional diagnosis of cytokine storm was made and given Injection Toclizumab 400mg intravenously. On day 33 after the onset of his symptom he had worsening of dyspnea. X-ray chest showed pneumomediastinum with bilateral mild pneumothorax and bilateral lung infiltrates. Following CT chest (Figure 3) showed severe pneumomediastinum, bilateral pneumothorax and diffuse ground glass densities with sub pleural consolidation. The patient developed cardiac arrest and could not be resuscitated.
 (a)
(a)
 (b)
(b)
 (c)
(c)
Fig. 3a Chest radiograph of a 65-year-old hospitalized patient showed pneumomediastinum (yellow arrows) and bilateral pneumothorax (green arrows). b) Follow up axial CT images of the patient depicts diffuse ground glass densities, sub pleural consolidation along with the pneumomediastinum and bilateral pneumothorax.
Discussion
Spontaneous pneumomediastinum represents the presence of free air in the mediastinum. It is usually associated with bronchial asthma, forceful straining like coughing or vomiting and inhalation of drugs followed by Valsalva maneuver and infections like Pneumocystis carnii pneumonia, SARS etc., As known, it occurs when there is pressure gradient between the alveoli and interstitium and following air leak into the interstitium. This interstitial air then dissects into the mediastinum, pleural spaces and subcutaneous tissues. In COVID-19 pneumonia, the spontaneous pneumomediastinum is considered to be due to damage of alveolar membrane caused by the virus. Even though it is a self-limiting condition, the presence of spontaneous pneumomediastinum can be considered as the potential indicator for disease worsening.
Only a small fraction of patients with COVID-19 pneumonia develop spontaneous pneumomediastinum. In our study 11 out of 2440 (0.004%) had spontaneous pneumomediastinum. Majority of our patient cohort had comorbidities (90%), most common being diabetes mellitus and Hypertension. Only 1 patient had a history of smoking and preexisting lung disease evident on CT scan. From the study it is also clearly evident that preexisting pulmonary disease is not a risk factor for development of spontaneous pneumomediastinum. The patients had elevated inflammatory markers like LDH, CRP and ferritin. The presence of high LDH indicates cellular damage. All the patients had progressive clinical and radiological worsening with development of pneumomediastinum with or without pneumothorax and subcutaneous emphysema. These 11 patients developed spontaneous pneumomediastinum around the 3rd week of illness (the average was on 21st day), thereby showing that it is a delayed presentation. Among 11 patients, 7 patients were on noninvasive ventilation and 4 were managed without mechanical ventilation.
In our subset of patients, the mortality was 54.5% which was correlated with clinical worsening. Those patients who expired died within 10 days of onset of spontaneous pneumomediastinum.
Therefore, we would like to propose that developing spontaneous pneumomediastinum in the course of COVID-19 illness is a strong negative prognostic factor with significant increased mortality.
Conclusion
Developing Spontaneous pneumomediastinum is a rare imaging finding in COVID 19 pneumonia. We would like to conclude that one has to be watchful for this complication during the 3rd week of illness especially if there is a clinical worsening. Once developed it is a negative prognostic indicator with high mortality.
Acknowledgements
Thankful to Department of Diagnostic and Interventional Radiology, and the Department of Internal Medicine, Kauvery Hospital, Trichy.
References
[1]. Pan A, Liu L, Wang C, et al. Association of Public Health Interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323(19):1915 – 1923.
[2]. Wasilewsk PG, Mruk B, Mazur S, et al. COVID-19 severity scoring systems in radiological imaging – a review. Pol J Radiol. 2020;85:e361 – e368.
[3]. Zhou C, Gao C, Xie Y, Xu M. COVID-19 with spontaneous pneumomediastinum. Lancet Infect Dis. 2020;20:510.

Dr. Saranya Manickavasagam
Radiologist

Dr. V. Senthilvelmurugan
Radiologist

Dr. Ivan A. Jones
Critical Care specialist
Dr. G. Dominic Rodriguez
General Physician
