Upper limb replantations at different anatomical levels: a short case series
Kiran Petkar*
Department of Plastic and Reconstructive Surgery, Kauvery Hospital, Bangalore, India
*Correspondence: Tel.: +91 87691 83863; email: drkiranpetkar2009@gmail.com
Abstract
Background: Limb trauma causing complete or near-complete amputations are surgical emergencies. Re-establishing blood supply within the critical period of ischemia can save the amputated part. It requires precise re-anastomosis of the severed artery and vein under adequate magnification often using an operating microscope. Prompt repair of other structures is also done to retain the functionality of the limb.
Case presentation: The author presents three consecutive cases presenting with such injuries at different anatomical levels that were managed at Kauvery Hospitals during the COVID-19 pandemic. Three cases were operated and in all the cases salvage of the part was possible and good recovery to functionality was seen.
Conclusion: Microsurgical replantation in upper limbs gives gratifying results when done at right time, with right skills and using right instruments.
Keywords: Replantation, Upper limb re-implantation, Microsurgical replantation
Background
Injuries to upper limb resulting in complete or near-complete amputation of digits or hand is not uncommon [1,2]. They often occur during industrial accidents, road traffic accidents or house-hold injuries. Unless the blood circulation is re-established within the critical ischemia time, the loss of the distal part is inevitable.
In strict technical terms, re-attachment of a completely severed and separated part by reestablishment of circulation is called ‘replantation’ or ‘re-implantation’. While similar process with an incompletely severed ischemic part is termed ‘re-vascularisation’. Conventionally though, the words are used interchangeably.
Success of replantation depends mainly on precise vascular anastomosis of arteries and veins. As we go distally in the limb, the size of the blood vessels decreases. Hence it requires more finesse in microsurgical skills and equipments as we deal with structures more distally in the limb. Different levels of the limb pose different requirements and challenges to the reconstructive microsurgeon.
The author reports in this article, the three consecutive cases of replantation/re-vascularisations at different levels in upper limb done during the testing times of COVID-19.
Case Presentation
These cases were managed at Kauvery hospitals of Bangalore and Hosur, India. They were a single surgeon experiences of the author who is a plastic surgeon with special expertise in hand and microsurgery. They were all done during peak COVID-19 times after screening for corona virus infection by biological and chest imaging methods. None of the patients was found to be affected by the virus during or after hospitalization. Custom-designed loupe and high-end (Carl Zeiss Pentero®) operating microscopes were used for magnification.
Case 1
A 26-year-old gentleman, a factory worker suffered injury to his left hand under a heavy cutting blade, resulting in complete severance of the hand across the palm. He was rushed to the hospital and the amputated part arrived in an ice-box later wrapped in a dry cloth (Fig. 1a and b). The patient reached the hospital within one hour of the incident with a dressing on the stump to control bleeding. On examination, it appeared to be a rather clean-cut injury with a sharp object, but with avulsion of volar skin on the stump until and beyond the wrist (Fig. 1c). The level of transaction was flexor zone 3. All five metatarsals were severed just distal to carpometacarpal joints except the first, which was severed near metacarpo-phalangeal joint. Wound contamination was modest, with husk and soil. Patient did not have any co-morbidities and his investigations including hematocrit was within normal limits.
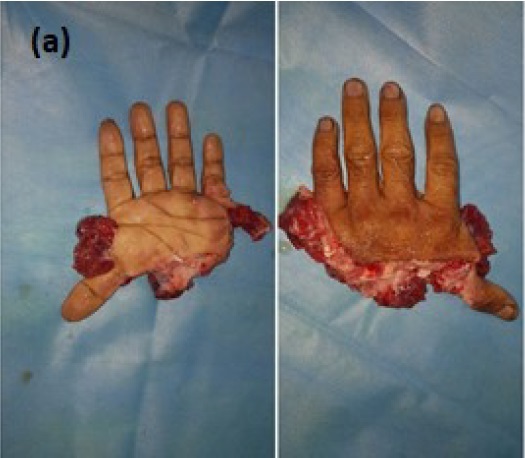


Fig 1a. Amputated hand, (b). Hand brought in ice box, (c). The stump with crush avulsion injury.
After obtaining informed consent, the patient was shifted to operation theatre. While a brachial plexus block was being administered, the amputated part was washed under running stream of normal saline over a waste basket. Bench-dissection of the part followed. Under loupe magnification, debridement of the contaminated and shredded tissues was done. Cut ends of superficial palmar arch, dorsal veins, median nerve, motor and sensory fascicles of ulnar nerve, and all flexor digitorum profundus (FDP) tendons and flexor pollicis longus (FPL) tendons were dissected out and identified. So were the extensor tendons over the dorsum. K-wires of 1.8 mm size were drilled from the thumb tip and 2nd to 4th metatarsal heads proximally in preparation of skeletal fixation (Fig. 2a).
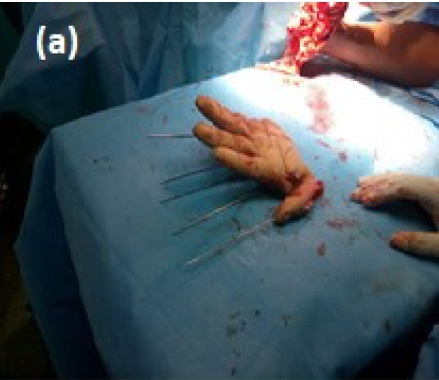
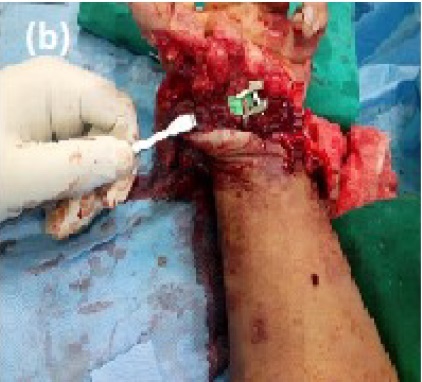

Fig. 2a. Replantation in progress. Ready for osteosynthesis, (b). Microvascular repair in progress, (c). Replanted hand.
By this time, the limb had been anesthetized, tourniquet applied and a thorough scrubbing had been done. The stump was then debrided. All the structures corresponding to those identified in the amputated part were dissected out. Crushed proximal ends of metatarsals were trimmed and shortened by about 5 mm. Vessels to be anastomosed were clamped and other bleeders were clipped. Tourniquet was release temporarily to ascertain good pulsatile flow from the arteries and easy flush into the dorsal veins.
The distal part was brought into the field. K-wires were driven into the corresponding proximal bones. FPL and FDP tendons were repaired using modified Kessler’s technique. Operative microscope was brought in. Median and ulnar nerve ends were trimmed and co-opted. Ulnar artery was repaired between double clamps using 9-0 nylon sutures. As the superficial continuation of radial artery was found to be crushed, deeper branch of radial artery was dissected out from the first web-space proximal to its branching into princeps polices. The same was transposed anteriorly and was anastomosed with the proximal cut end of radial artery thereby completing a palmar arch (Fig. 2b). The limb was then turned to prone position and all extensor tendons were repaired. Arterial flow was allowed temporarily to identify the veins having good flow from the distal part. As only two venous cut ends were available on proximal avulsed skin of the dorsum, two veins with good return were anastomosed to recipient veins on either ends of dorsal venous arch. After confirming the blood-flow through the venous anastomosis, the avulsed skin on the stump was pulled up and the wound was closed (Fig. 2c).
Case 2
A 55-year-old gentleman had a ring avulsion injury of his right ring finger. He was getting down from a vehicle when the ring he was wearing remained stuck on the holding bar avulsing the distal soft tissue. He had circumferential injury to the finger and the finger was found ischemic (Fig. 3a and b). He was immediately taken up for surgery. Under brachial plexus block, the wound was explored. His digital arteries were found to be in spasm due to stretch, dorsal veins were all found transected. However, the digital nerves and tendons were found to be intact.
 Fig 3 (a). Ring avulsion injury with ischemic finger, (b). Extent of injury to neurovascular structures, (c). Microvascular repair completed.
Fig 3 (a). Ring avulsion injury with ischemic finger, (b). Extent of injury to neurovascular structures, (c). Microvascular repair completed.
The digital arteries were teased out of the constricting connective tissue and pulled across. Xylocard was pushed into their adventitia. The vessels successfully were relieved of their spam and the flow was re-started. The dorsal vein was repaired under microscope using 9-0 nylon (Fig. 3c). As there was some skin loss due to crush injury, a split skin graft from the same forearm was used to cover the wound.
Case 3
A 45-year-old gentleman suffered injury to both hands with a power saw. Among other injuries, his left index finger had near-total amputation at a level just distal to distal interphalangeal joint. The distal part was hanging by a thin strip of dorsal skin. There was no demonstrable vascularity in the distal part (Fig. 4a).


Fig. 4a. Near total amputation at distal interphalangeal joint level with distal ischemia, (b). Good blood flow after microvascular repair of digital artery.
He was taken up for emergency surgery. Bony fixation was done by a K-wire passing through the fracture and the joint. Under tourniquet control and magnification under microscope, the wound was explored. Both the digital arteries were found to be transected. As the cut was oblique, the ulnar side digital artery was expected to be transected more proximally before it ended up in tiny branches. The assumption turned out to be correct and two cut ends of the said artery with lumen were detected under microscope. The ends were trimmed and prepared. Anastomosis was performed with 10-0 nylon. Blood flow was confirmed (Fig. 4b). Adequate venous drainage through the intact dorsal skin was confirmed. Cut ends of the digital nerve were too small and fibrous and were not amenable for suturing. Loose skin sutures were placed.
Results
All three replanted parts survived with demonstrable blood flow into the part. The first case had shock and unconsciousness on second postoperative day which was managed by emergency intubation and supportive measures. The replant survived through the event. However, the avulsed skin on the volar aspect of wrist necrosed after one week and needed a flap cover (Fig. 5). The ring avulsion finger had an extensor lag which later improved with continued physiotherapy (Fig. 6a and b). The third case is in recovery with good healing of suture-line in third postoperative week at the time of writing this paper (Fig. 7).
 Fig 5. Hand surviving with good blood flow on Day 10.
Fig 5. Hand surviving with good blood flow on Day 10.
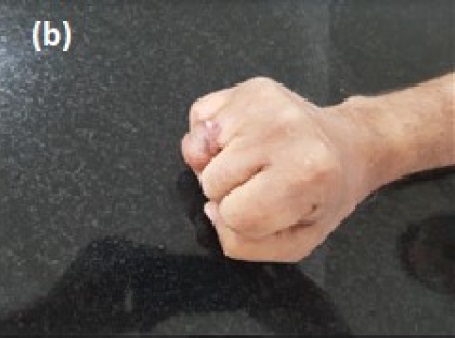
Fig. 6a. Useful hand with good functional range, (b). Useful hand with good functional range.
Discussion
Permanent loss of part of an upper limb often has a huge impact on the life of a person. Unlike in lower limb, prosthetics in upper limb fall too short of replacing the lost parts. That is because of the specialized and unique organ that upper limb has evolved into in humans. It is worthwhile to recall at this point that, along with the frontal cortex, it is the skill of the hand that has made humans the rulers of the world. All of the world’s technology is yet to manufacture an artificial hand that can merely pick up an egg consistently, without dropping it or crushing it into the yolk. Such a precious organ has all the reasons to be preserved at all costs.
 Fig 7. Fingertip surviving on Day 18.
Fig 7. Fingertip surviving on Day 18.The cases discussed here represent three different scenarios. Three men in different age groups, in different environments had limb injury by different mechanisms. The anatomical levels were also different. But the common factor was the imminent loss of the distal part. Only a successful re-establishment of blood flow could prevent the hitherto inevitable permanent handicap. It was attempted in each case and was achieved successfully.
Upper limb replantations or re-vascularisations yield fair to good results when performed by the right surgical team, using right equipments, within right ischemia time and on right indication. The microsurgeon should not only be well-trained and experienced, but also should have a consistent team to work with. A good quality operative microscope ergonomically designed for microvascular surgery is essential and so is a set of good quality microsurgical instruments. Their maintenance and upkeep is also equally important to get the best possible outcome. As it is a long and arduous surgery, it is very easy for the surgeon to get frustrated with sub-optimal conditions and lose concentration. It is said that success in microvascular surgery is a function of a cumulative adherence to good practices during each step.
Good referral practices with an awareness among all healthcare workers in the geographical region makes for patients reaching the right medical facility within the critical ischemia time. Advocacy of the good work is also essential to enjoy patronage of the society and take the medical advances to the common man.
Although only clean cut injuries are often picked up for replantation to reduce the number of failures, every piece of upper limb that is intact should be considered for replantation. That is unless the part is completely crushed and mangled beyond utility. Several scoring systems help us in decision-making. Only other concomitant life-threatening injuries pose relative or absolute contraindications to an attempt at salvage.
Major amputations like the first case expectedly require several secondary procedures to regain maximum functionality. All cases in general need prompt follow-ups and physiotherapy for best results. Hence it takes some commitment on the part of the society to invest sufficient resources in this endeavor. In turn it makes a worthy investment for the nation at large as it is often the working hand that gets injured. It illustrates one of the highest social and humanitarian compassion.
It also is a rather surrealistic depiction of the zenith of human evolution, as one skilled hand (surgeon’s) works on the other (patient’s) to reinstate the skill of the latter!
Conclusion
Microsurgical replantations in upper limb give gratifying results with salvage of the ischemic part and good functional recovery when performed at right time, with right skills and using right instruments.
Acknowledgements
The author acknowledges the orthopedic and anesthesia colleges for their referral and cooperation. Also acknowledgements to marketing, administrative and paramedical teams for their role in this team-work.
References
- Buncke HJ, Alpert BS, Johnson-Giebink R. Digital replantation. Surg Clin North Am. 1981; 61(2):383-394.
- Urbaniak JR, Evans JP, Bright DS. Microvascular management of ring avulsion injuries. J Hand Surg Am. 1981;6(1):25-30.
