What is Aspiration Pneumonia?
A lung infection that occurs after food, vomit, blood or stomach acid is inhaled into the lungs.
Risk Factors for Aspiration Pneumonia
Elderly people are at a higher risk of aspiration than younger individuals. This is due to age-related factors and disease conditions. Some of them are mentioned below:

- Altered consciousness due to drugs, falls, seizures and alcohol intake.
- Neurological disorders like stroke, Parkinson’s disease and dementia because of impaired swallowing mechanisms.
- Issues related to mechanical tubes/procedures like blockage of nasogastric (feeding) tubes, during endoscopy, endotracheal intubation, feeding too early post bronchoscopy procedure, etc.
- Feeding-related issues like protracted vomiting, intestinal obstruction, large volume nasogastric tube feedings, feeding in recumbent (lying down) position, reduced gastric emptying/gastroparesis, etc.
- Poor oral hygiene
- Post cardiac arrest
Causes Specific to the Elderly in Nursing Home
- Inappropriate food being given to a patient with an impaired swallowing mechanism
- Food given in large pieces
- Patient trying to feed himself without supervision
- Food given while the patient is lying down
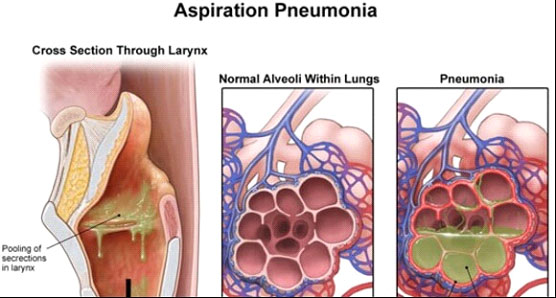
Pathophysiology
The above conditions lead to the pooling of secretions in the throat which leads to aspiration of gastric contents into the lungs causing an inflammatory reaction because of the acidity of the contents thereby causing respiratory distress. Usually, it is chemical pneumonitis and resolves with conservative management. However, risk factors for bacterial pneumonia include patients with neurological conditions, poor oral hygiene, intestinal obstruction and aspiration in hospital/nursing home settings.
Specific Mechanisms in Elderly
- Impaired gag reflex in neurological conditions
- Difficulty in swallowing due to strictures in esophagus or neurological conditions
- Impaired cough effort due to old age or sedation
- Presence of a feeding tube
- Compromised immune response due to old age, disease or drugs
Aspiration Pneumonia Symptoms
Fever, bouts of cough, sputum, breathing difficulty, hypoxia and confusion.
Investigations
- Complete Blood Count – Increased WBC count
- X-ray Chest – Infiltrates especially in the lower zones
- Bronchoscopy – Pooling of secretions in the airway
Aspiration Pneumonia Treatment
Chemical pneumonitis usually responds to conservative management. However, if any of the risk factors mentioned above for bacterial infection are present, then antibiotics are started. This along with supportive measures usually suffice. Some patients can develop low blood pressure/hypotension and worsening breathlessness inspite of the above measures. In such cases, patients might need medications to maintain blood pressure and ventilator support with the placement of an endotracheal tube.
Preventive Measures
Swallowing assessment should be done by a trained expert in patients at risk of aspiration. This can include endoscopic assessment of swallowing. There are certain measures which can be taken by the attendants to reduce the risk of aspiration. These include the following:
- Make sure the person to be fed is brisk and responsive to verbal commands, especially for oral feeding.
- Ensure proper oral and dental hygiene.
- If the person is on dentures, make sure they are properly fitted.
- Feeding should be done by a person who is adequately trained by an expert.
- Make sure the individual is adequately rested before feeding. A tired individual has higher chance of aspiration.
- Don’t try to feed a person who has abdominal distension and hasn’t passed stools for a few days especially if associated with nausea and vomiting. In such cases, consult the treating physician.
- Maintain an upright posture (90 degrees) of the individual while feeding.
- Feed slowly and in small pieces.
- Give food bolus only when the previous bolus has been completely swallowed by the patient and the mouth is empty.
- Ask the individual about feelings of nausea, fullness or abdominal pain between food boluses.
- Alternate between solid and liquid boluses.
- Don’t continue feeding food boluses if the individual coughs during swallowing attempts. Coughing in such a scenario could be due to aspiration.
- Always seek the help of a speech and swallow therapist in case of difficulties.
- After the feeding is complete, make the individual stay in an upright position for at least 30 minutes.
- For those on tube feeding, make sure the tube is in the proper position and there is no blockage before initiating feeding.
- Avoid giving increased volume of feeds via the feeding tube than what was advised by the treating physician.
- Aspirate the feeding tube with a syringe before feeding to look for residual contents from the previous feeding session. If a significant amount could be aspirated, don’t feed – seek expert advice.
- If the patient is on a tracheostomy tube, reduce cuff pressure during feeds to allow for easy swallowing. However, if the patient coughs during feeding, stop further feeding and reinflate the tracheostomy cuff.
- If the patient is on PEG (percutaneous gastrostomy) feeding, the patient can still aspirate and hence all preventive measures have to be followed as in other modes of feeding.
- Always watch for symptoms of aspiration as mentioned above and seek timely medical advice. Meanwhile, keep the patient upright, check his/her vital signs and supplement oxygen if necessary.

Dr. R. Nithiyanandan
Associate Consultant Pulmonary and Critical care
Kauvery Hospital Chennai
