Approach to cardiac arrest
Revathy1, Priya2, Ashwina3, Ramya Sri3, Vaishna Abi3
1Emergency Ward Nursing Incharge, Kauvery Heartcity, Trichy, India
2Emergency Ward Senior Staff Nurse, Kauvery Heartcity, Trichy, India
3Emergency Ward Staff Nurse, Kauvery Heartcity, Trichy, India
*Correspondence: nursing.heartcity@kauveryhospital.com
Abstract
Cardiac arrest is a medical emergency. Cardiac arrest occurs when the heart suddenly and unexpectedly stops pumping. If this happens, blood stops flowing to the brain and other vital organs. Certain types of arrhythmias that prevent the heart from pumping blood cause cardiac arrest.
Background
Cardiac arrest is a medical emergency. Cardiac arrest is the cessation of cardiac mechanical activity resulting in the absence of circulating blood flow. Cardiac arrest stops blood from flowing to the vital organs, depriving them of oxygen and, if left untreated, results in death. Certain types of arrhythmias that prevent the heart from pumping blood cause cardiac arrest.
Definition
It is a condition in which the heart suddenly and unexpectedly stop beating and the cessation of blood flow to the brain and other vital organ follows.
Risk Factors
- Abnormal heart rhythms
- Cardiomyopathy
- Congestive heart failure
- Coronary artery disease
- Previous myocardial infarction
- Excessive alcoholism and smoking
- Pulmonary embolism
- Hypertension
- Diabetes mellitus
- Obesity
- Dyslipidemia
Causes
- A heart attack ( acute coronary syndrome)
- A severe hemorrhage
- Hypoxia (a severe drop in oxygen levels)
- Electrocution.
- A drug over dose.
- Massive pulmonary embolism.
- Tension pneumothorax.
- Pericardial tamponade.
- Hyperkalemia or hypokalemia.
- Hypoglycemia.
In our patient, it was caused by coronary artery disease (Inferior- posterior wall myocardial infarction)
Case Presentation
A 56-year-old male, newly detected to have diabetes, normotensive, had a history of chest pain associated with sweating for 1 hour for which he came here for further management. He had developed cardiac arrest on the way to the hospital. On arrival at casualty, he was unresponsive and unconscious; blood pressure, heart rate and saturation were not recordable.
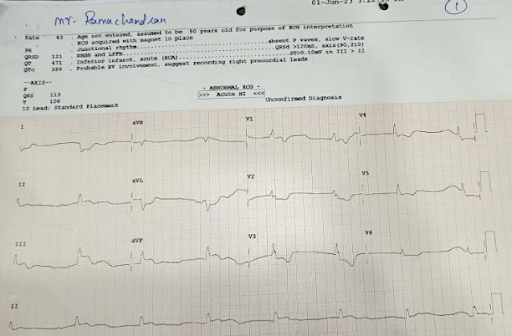
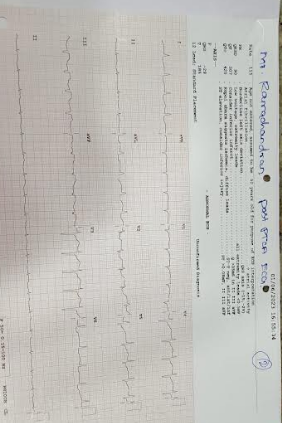
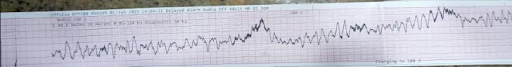
Summary of management
Immediate CPR was initiated as per ACLS protocol and emergency intubation was done by cardiac anesthetist and he was placed on mechanical ventilator. Following this he developed refractory VT and VF; hence multiple shocks were delivered. ECG revealed inferior-posterior wall myocardial infarction with complete heart block. ECHO revealed mild LV dysfunction. Emergency TPI insertion was done. He was started with IV anti-coagulants, inotropes, IV anti-biotic and other supportive measures. He was advised Primary PTCA for further management. After an informed high-risk consent, patient was taken up to Cath lab,emergency CAG was done followed by RCA stenting.
Details
Immediate Care
- Patient he was received from emergency department unresponsive and unconscious.
- Immediate start of CPR and ambu ventilation, then followed as per ACLS protocol.
- IV line secured, Inj.Adrenaline 1st dose given, CPR continued
- Emergency intubation done by 8.5 size tube with fixed 22cm, Fio2 100, PEEP 5 Pressure support 10 Respiration rate 22 Tidal val 450
- The monitor rhythm showed VF; DC shock 150ju given.
- Primary consultant saw the patient, ECHO done, history collected from attenders, poor prognosis explain to the attenders.
- Inj.Adrenaline 2nd dose give followed ACLS protocol.
- High-risk consent obtained.
- The monitor rhythm showed VF, DC shock 200ju given. Continued CPR.
- Inj.Adrenaline 3rd dose given followed ACLS protocol.
- Repeat VT, VF; 200ju DC Shock given.
- Dual inotropes started
- We continued CPR, as an extra mile, for 1 hour, hands changed at regular intervals.
- A rhythm with complete heart block and heart rate 25 b / minutes was achieved
- Inj.Atropine 2 doses given
- ECG and echo showed a ray of hope, with good myocardial contractions with bradycardia
- Temporary pace maker placement done.
- Immediately patient shifted to Cath lab for Primary PCI
- Patient to Cath lab and emergency CAG done with RCA stenting
- Patient was shifted to CCU
Coronary Angiography
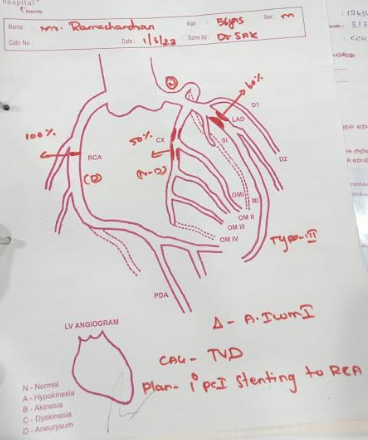
ECGs show: Infr-Postr Ac MI, Ventricular Tachycardia and Ventricular Fibrillation
Post PTCA ECG

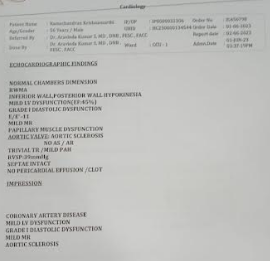
ECHO ReportInvestigation findings: Mild LV Dysfunction – EF-45%
Nursing Management
- Patient was shifted to CCU for further close monitoring
- Vital signs were constantly monitored and intake and output are maintained.
- Blood investigations were done. Investigations included ABG, CBC, ESR, Sodium potassium, RFT, blood grouping and typing and serology.
- Nurses followed AIDET techniques (knowledge, introduction duration, explanation and thanks) of communications and with patients, participants to gain their trust and improve the statistical level.
- Next, patient became conscious
- Inotropes were tapped and stopped.
- On third day patient was shifted to room and discharged.
Condition at discharge
General condition: patient conscious and oriented
Vital signs: PR 102 b/mts, BP 130/70 mm/Hg
CVS: S1, S2 (+)
P/A: Soft
CNS: Within normal limits
Advice on discharge
Diet: 1500 kcal low -fat and diabetic diet
Medications
Tab.Torplat 90mg 1-0-1
Tab.Ecosprin 75mg 0-1-0
Tab.Tonact 40mg 0-0-1
Tab.Pantocid 40mg 1-0-0 (Before Food)
Tab.Dreamer 0.5mg 0-0-1
Syp.Potklor 10ml 1-1-1
Nephrologist advice medications
Tab.Nodosis 500mg 1-0-1
Tab.Nefrosave 1-0-1
Diabetic Advice Medications:
Inj.Human Actrapid S/C 6U-6U-0
Inj.Lantus Solaster S/C 0-0-6U
Review
We scheduled a review two weeks from the discharge date and patient was advised to follow all the instructions at her home as well.
Outcome
The patient returned home happy. The family appreciated we saving the father.
Moral of story
- There is no time limit for CPR continue CPR in a dedicated way even for one hour if you have positive feel on patient’s outcome
- Attenders who witnessed the entire event in casualty profusely thanked and appreciated our team for quick response and successful CPR

Ms. Revathy
Emergency Ward Incharge

Ms. Priya
Emergency ward Senior Staff Nurse

Ms. Ashwina
Emergency Ward Staff Nurse

Ms. Ramya Sri
Emergency Ward Staff Nurse

Ms. Vaishna Abi
Emergency Ward Staff Nurse
