Cerebral malaria: Management with artesunate
N. Dharsshini
Pharm. D Intern, Kauvery Hospital Cantonment, Trichy
Background
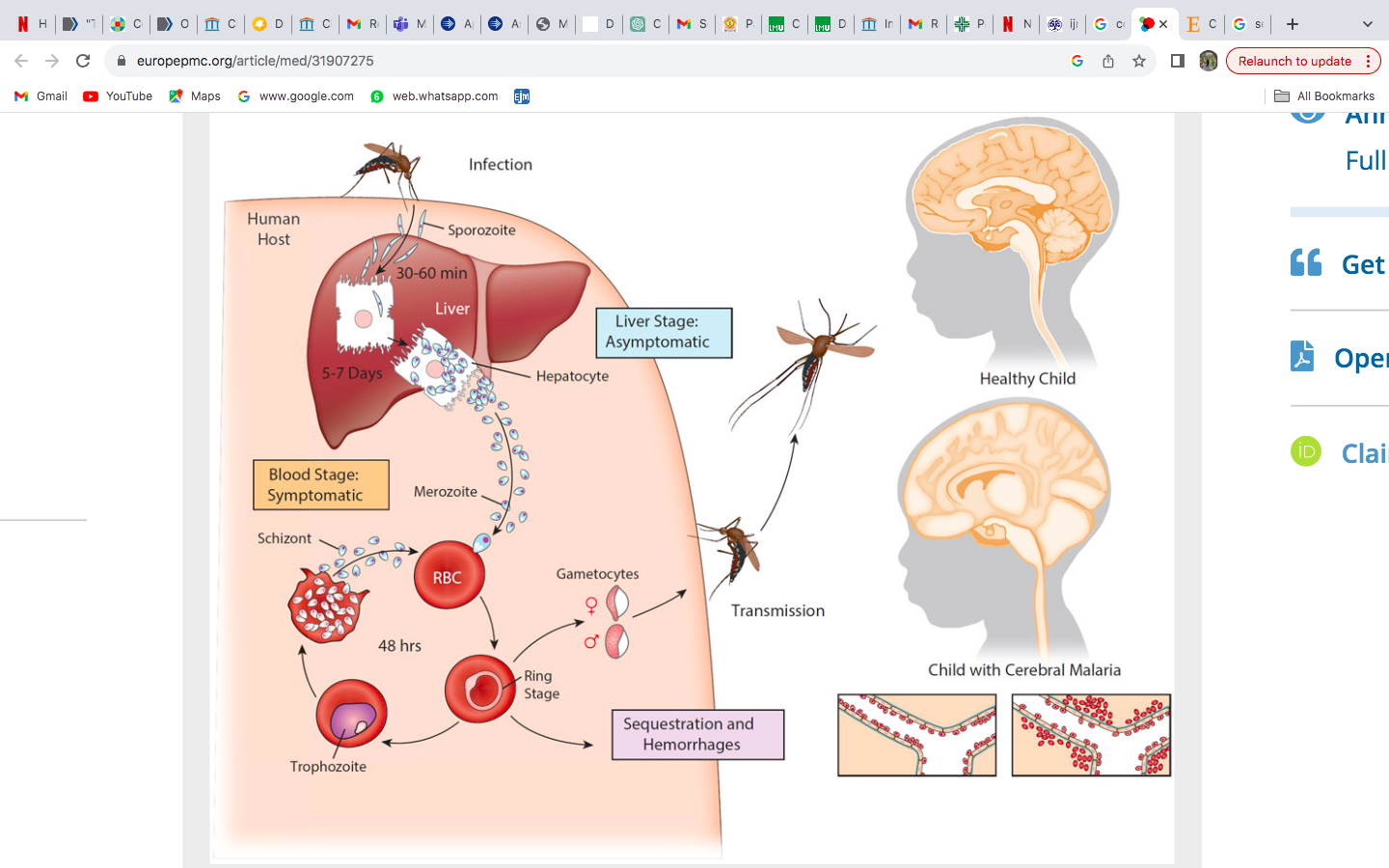
Malaria is a vector-borne infectious disease caused by Plasmodium parasites, transmitted through the bites of infected Anopheles mosquitoes. Plasmodium falciparum is a major species responsible for severe cases, including cerebral malaria. The parasite undergoes a complex life cycle involving both human and mosquito hosts. In humans, it infects liver cells (hepatocytes) and red blood cells, leading to recurrent cycles of fever and chills.
Cerebral malaria, a severe complication of Plasmodium falciparum infection, involves the sequestration of infected red blood cells in brain micro vessels. This leads to microvascular obstruction, triggering an inflammatory response and endothelial dysfunction. The resulting hypoxia, ischemia, and cerebral edema cause neurological symptoms and signs, including altered consciousness and seizures and also systemic complications. If untreated, cerebral malaria can progress to severe complications like multi-organ dysfunction, and death, emphasizing the need for prompt intervention.
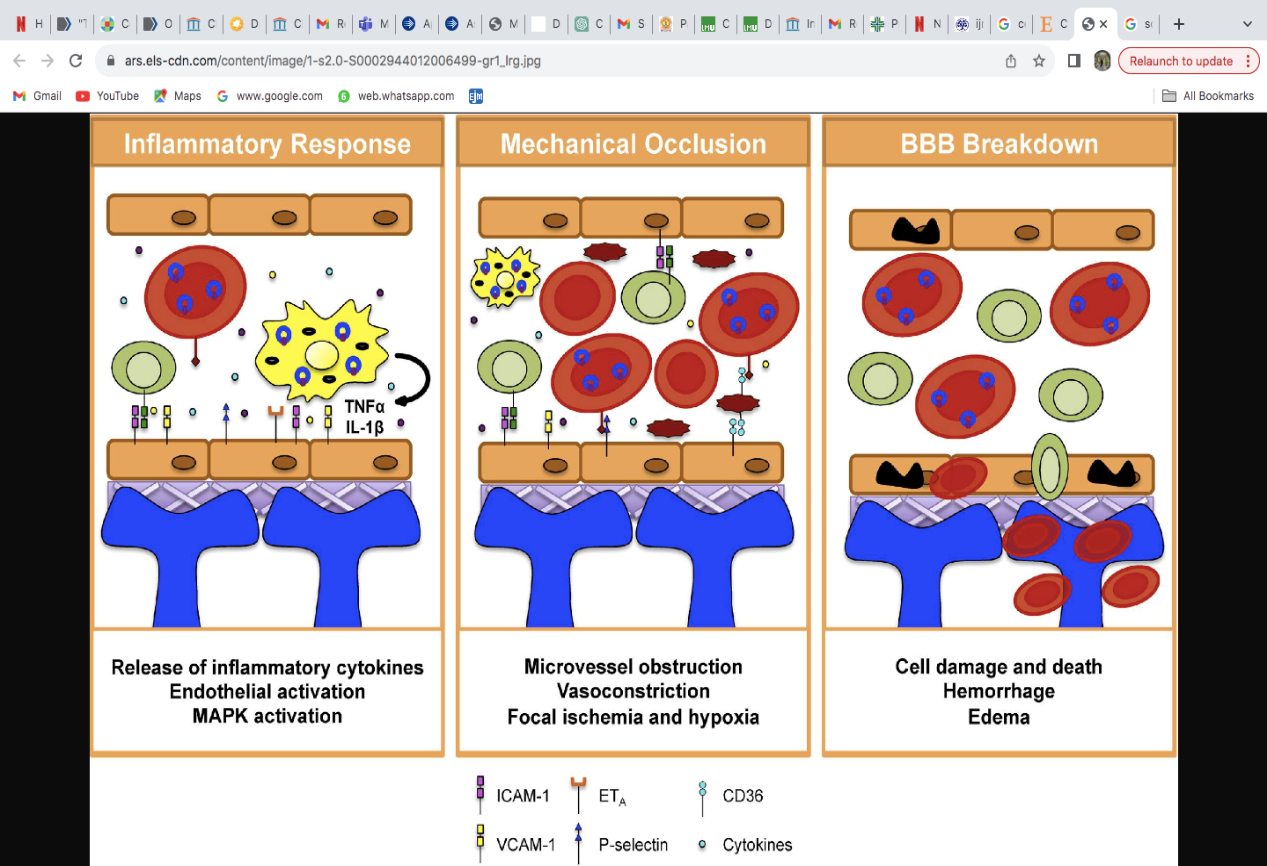
The pathophysiology is complex, involving intricate interactions between the parasite and the host immune response
- The key elements include the adherence of infected red blood cells to brain micro vessels, leading to microvascular obstruction and compromised blood flow.
- This triggers an inflammatory response, causing endothelial dysfunction and disrupting the blood-brain barrier. Vascular dysfunction with subsequent BBB damage is a major feature of Cerebral malaria [1],[2],[3]
- The hypoxia, apoptosis, ischemia, cerebral edema are disruptive, leading to haemorrhagic lesions and neurological signs such as altered consciousness and seizures.
Proposed mechanism of vascular damage and BBB dysfunction in Cerebral Malaria
Life Cycle of Plasmodium Falciparum and depicting cerebral malaria pathology
Case Presentation
A 26-year old male patient presented to hospital with intermittent fever, loss of weight, joint pain for one month, chills, vomiting, and high coloured urine for 3 days. He had recently returned from Africa where he went for work. Medical history included psoriasis for one and half year on medications. On examination he had neck stiffness, breathing was spontaneous and adequate, vocalized airway with no secretion. All peripheral pulses were fast.
Vitals and Lab Investigations
- Laboratory work was significant for hemoglobin – 11.9 g/dL, white blood cell count – 4100 cells/cumm, platelet count – 40000 cells/cum, lactate dehydrogenase – 478 (U/L), bilirubin – 2.71 mg/dl, C-reactive protein – 275 mg/dl, elevated Procalcitonin and mild metabolic acidosis. Scrub typhus IgM showed positive.
- Peripheral blood smear was positive for P. falciparum malarial rings with 9% parasitic load.
- Magnetic Resonance imaging scan of the head showed cerebral edema. Ultrasound abdomen showed hepatosplenomegaly and splenic infarct.
- The patient was admitted to the intensive care unit. He was disoriented and unresponsive. On physical examination, he was sedated and paralysed, with generalized edema. He was intubated, and was on mechanical ventilation.
- On day 4 of stay, he developed gasping breath on SIMV (synchronized Intermittent Mandatory Ventilation), high peak pressure and tube block was noted.
- Bradycardia was noted with heart rate of 45 b/m, and he had cardiac arrest. CPR was done, and patient was reverted with Inj. adrenaline 1 mg IV stat. Fever spikes were persisting patient being anemic and thrombocytopenic.
Management
He was started on IV Doxycycline and Artesunate .Other antibiotics like meropenem, ceftriaxone, and azithromycin were also started. The patient was on continuous infusion of Fentanyl and midazolam 3 ml/hr and vecuronium with normal saline. He was also treated with levetiracetam to control the seizure activities, as well as IV Fepanil sos, paracetamol and vitamin K.
Discussion
- This case entails the presentation of a severe form of cerebral malaria (CM) with acute brain edema in a young, immunocompetent adult.
- Despite ongoing research, the precise pathophysiology of CM and its associated brain edema remains elusive. Current theories propose that the sequestration of infected red blood cells within small cerebral blood vessels may lead to their occlusion, resulting in cerebral ischemia. It is posited that parasite-infected red blood cells contribute to endothelial cell dysfunction, triggering the release of tumour necrosis factor-α and nitric oxide. These molecular processes are thought to be implicated in the development of brain edema in cases of cerebral malaria.[4],]5]
- Thrombocytopenia, anemia, metabolic acidosis, acute respiratory distress syndrome (ARDS), and multi-organ dysfunction indicate an advanced and potentially life-threatening stage of severe malaria. In some cases quick progression to the multi-organ dysfunction was strictly connected to delayed malaria recognition. But specific antimalarial treatment with intravenous artemisinin inflow in appropriate dosages together with application of intensive general treatment prevented the patient from fatal complications.
- The patient was followed-up for several weeks and showed only long lasting anemia, probably as a result of artemisinin intake which was corrected.
Artesunate
It is an artemisinin derivative and belongs to the artemisinin class of antimalarial drugs. Artesunate’s primary action in malaria is rapidly reducing the parasite burden, alleviating systemic effects, and contributing to complication resolution. In cerebral malaria, its prompt action indirectly mitigates cerebral symptoms by improving endothelial function and reducing inflammation. While artesunate plays a crucial role in addressing the malaria infection, additional therapeutic measures are often needed for directly managing cerebral edema in severe cases. This includes supportive care, intracranial pressure control, fluid administration, and potentially other medications targeting brain swelling.
Reference
- Rénia L, Howland SW, Claser C, Gruner AC, Suwanarusk R, Teo TH, et.al. Cerebral malaria: mysteries at the blood-brain barrier. Virulence. 2012;3(2):193-201.
- Medana IM, Turner GD. Human cerebral malaria and the blood-brain barrier. International journal for parasitology. 2006;36(5):555-68.
- Medana IM, Turner GD. Human cerebral malaria and the blood-brain barrier. International journal for parasitology. 2006;36(5):555-68.
- Sahu PK, Satpathi S, Behera PK, Mishra SK, Mohanty S, Wassmer SC. Pathogenesis of cerebral malaria: new diagnostic tools, biomarkers, and therapeutic approaches. Frontiers in cellular and infection microbiology. 2015;5:75.
- Wassmer SC, Moxon CA, Taylor T, Grau GE, Molyneux ME, Craig AG. Vascular endothelial cells cultured from patients with cerebral or uncomplicated malaria exhibit differential reactivity to TNF. Cellular microbiology. 2011;13(2):198-209.

Dharsshini
Clinical Pharmacy – Intern
