Dilated cardiomyopathy
G. Vijayalakshmi1,*, T Ambika2, M Rajeshwari3
1Non Critical Ward Incharge, Kauvery Heartcity, Trichy, India
2Senior Staff Nurse, Kauvery Heartcity, Trichy, India
3Senior Staff Nurse, Kauvery Heartcity, Trichy, India
*Correspondence:+91 85086 98000 ;nursing.heartcity@kauveryhospital.com
Background
Cardiomyopathies are disorders of the cardiac muscle that cause mechanical and/or electrical dysfunction that result in dilated, hypertrophic or restrictive pathophysiology.
Dilated cardiomyopathy is a non-ischemic heart muscle disease with structural and functional myocardial abnormalities. It typically starts in the heartí¢€â„¢s main pumping chamber (left ventricle). Dilated cardiomyopathy makes it harder for the heart to pump blood to the rest of the body.
Dilated cardiomyopathy (DCM) is a clinical diagnosis characterized by left ventricular or biventricular dilation and impaired contraction that is not explained by abnormal loading conditions (for example hypertension and valvular heart disease) or coronary artery disease.
Mutations in several genes encoding structural components of the sarcomere and desmosome could be involved in the causation of idiopathic DCM. The heterogeneous aetiology and clinical presentation of DCM make a correct and timely diagnosis challenging.
Common Etiology
- Autoimmune diseases such as connective tissue disorders.
- Conditions that damage the heart such as Hemochromatosis or Sarcoidosis.
- Endocrine conditions such as diabetes or thyroid disease.
- Family history of cardiomyopathy or sudden cardiac arrest may suggest a genetic etiology.
- The most common secondary cause is coronary artery disease or myocardial infarction.
- Poorly controlled high blood pressure.
Case Presentation
A 45 years female, euglycemic and normotensive, had a history of chest pain one month back for which she was initially evaluated at an outside hospital and then came to Heartcity with chest pain and, shortness of breath on exertion. She was reviewed in OPD and relevant investigations were done.
On examination, vital signs were:
- BP: 100/80 mmHg, pulse: 72/mt regular, CVS: S1 S2, RS: BAE (+), P/A: soft, CNS: within normal limits.
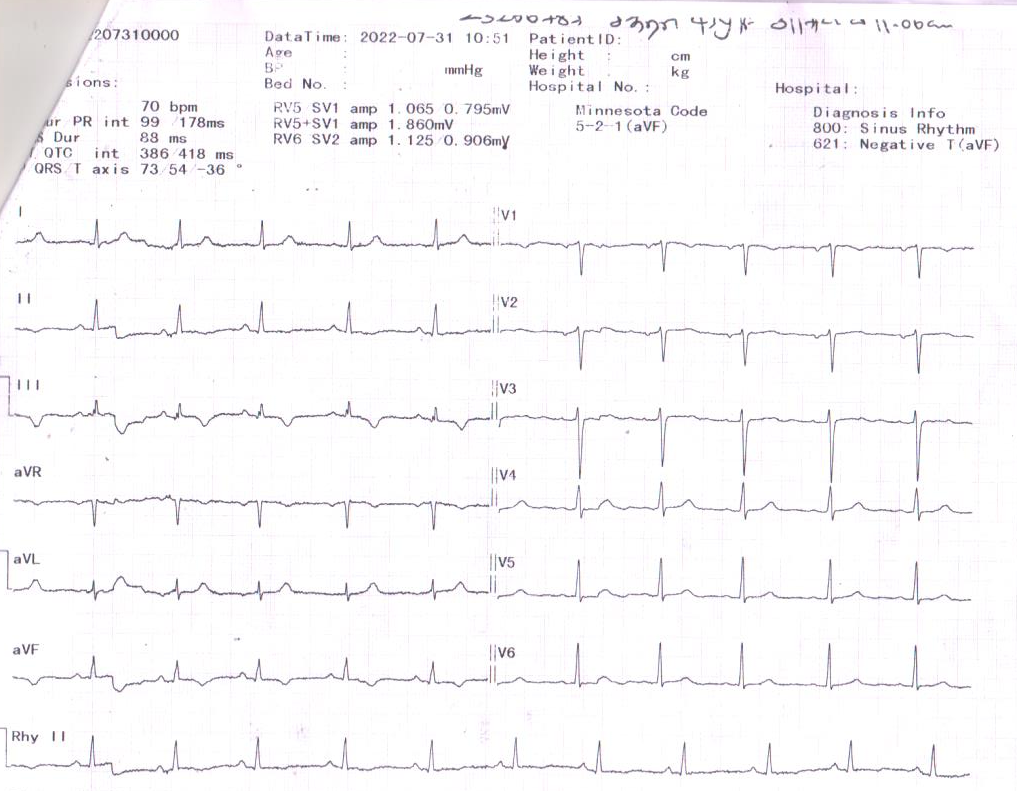
- ECG revealed right bundle branch block, left anterior fascicular block and ventricular premature contraction.
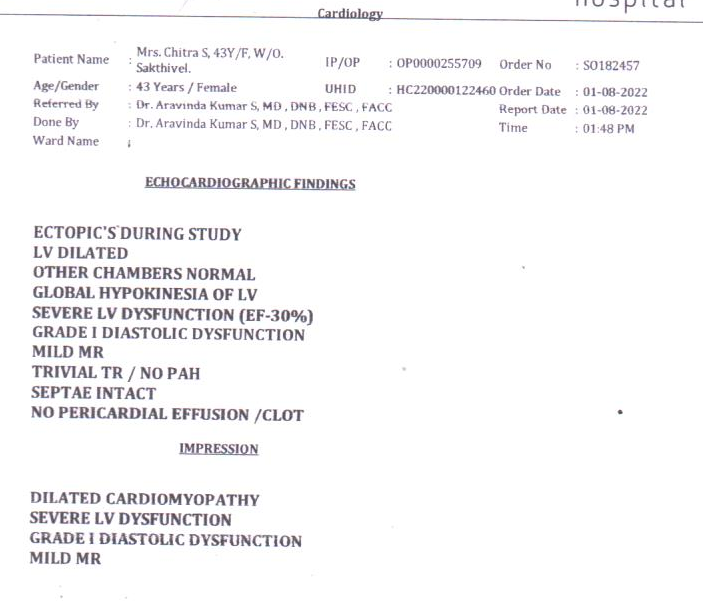
- ECHO revealed dilated cardiomyopathy with severe left ventricular dysfunction, grade I Diastolic dysfunction, and mild MR (See attached images. Dilated LV, increased LV internal diameters)
- Lab investigations revealed nothing significant. COVID RT-PCR í¢€â€œ Negative
ECHO
ECG
Diagnosis
- Dilated Cardiomyopathy
- Severe LV dysfunction
- Grade I diastolic dysfunction
- Mild Mitral regurgitation
She was advised coronary angiogram, and she got admitted on 08.09.2022.
After an informed consent patient was taken up for a coronary angiogram on 09.09.2022, which revealed normal coronaries and she was advised of medical management.
There were no procedural and post-procedural complications and her post-procedural period was uneventful.
Holter monitoring was done. It revealed a normal study with occasional VPCí¢€â„¢s.
Treatment
The patient was treated with beta-blockers, diuretics, and other supportive measures.
She was discharged in a stable state.
Nursing management of Dilated Cardiomyopathy
- Patient was shifted to Critical Care Unit 1 with a duty doctor and continuous cardiac monitoring.
- Nurses maintained an every 15minutess B.P chart. BP was stabilized with inotropes and IV fluids.
- Obtained vital signs every Q2H once stabilized after the procedure.
- Assessed the patient for changes in neurological function hourly and as clinically indicated. Assessed for skin warmth, colour and capillary refill time.
- Assessed for chest discomfort because myocardial ischemia may result from poor perfusion.
- Patient was managed with cardiac medications and diuretics as prescribed.
- Administered supplemental oxygen for the patient to relieve dyspnea.
- Evaluated the patientí¢€â„¢s chief complaints that were presented during admission that includes fever, syncope, general aches, fatigue, palpitations, and dyspnea.
- Auscultated lung sounds for crackles (pulmonary edema) or decreased sounds (Pleural effusion).
- Patient was under continuous monitoring.
- Nurses used the AIDET technique (Acknowledge, Introduce, Duration, Explanation and Thank you) while communicating with patients and attendees to gain their confidence and improve their satisfaction level.
Discharge advice
Frequent readmissions cause an immense burden on the individual the family and the healthcare system. Heart failure management programmes, in which patient education is an important component, have been shown to be effective in improving self-care and reducing readmissions.
- Limit canned, dried, packaged and fast foods.
- Don’t add salt to your food.
- Season foods with herbs instead of salt.
- Watch how much liquid you drink. Drinking too much can make heart failure worse.
- When you eat out ask that your meals have no added salt.
- Reduce alcohol consumption, weight loss, exercise, smoking cessation and a low sodium diet.
- Avoid stress.
- Review after 2 weeks.
Discharge medications
| Tab. Concor | 2.5 mg | 1-0-1 BD |
| Tab. Dytorplus | 10 mg | 0-1/2-0 |
| Tab. Dreamer | 0.5 mg | 0-0-1 |
Recovery
After a long stay in the hospital, the patient became stable with the efficient care of nurses and went home happily.
.jpg)
G. Vijayalakshmi
Non-Critical Ward Incharge

T. Ambika
Senior Staff Nurse

M. Rajeshwari
Senior Staff Nurse
