Glycogen Storage Disease (GSD)
J Jane Abishak1,*, A. Mercy2, K. Priyadharshini3, Akshaya4
1Critical Ward Supervisor, Kauvery Heartcity, Trichy, India
2Critical Ward Incharge, Kauvery Heartcity, Trichy, India
3Critical Ward Senior Staff Nurse, Kauvery Heartcity, Trichy, India
4Critical Ward Staff Nurse, Kauvery Heartcity, Trichy, India
*Correspondence: nursing.heartcity@kauveryhospital.com
Background
Hypertrophic Cardiomyopathy (HCM)
A condition in which the heart muscle becomes abnormally thick. Most of the people with this condition have shortness of breath, chest pain or abnormal heart rhythms. An ECHO is a best method to diagnose Hypertrophic Cardiomyopathy. The treatment includes medication to slow or regulate the heart rate.
Glycogen Storage Disease (GSD)
GSD is a rare condition that changes the way the body uses and stores glycogen. It is a condition in which the body cannot break down glycogen. (GST Type I: Von gierke’s disease)
Case Presentation
A 24 years old male patient came with complaints of breathing difficulty and bilateral leg swelling for 3 days. He was diagnosed to have Hypertrophic Cardiomyopathy, GSD type I. S/P Right lateral mandibular surgery. Patient was on blockers earlier and had stopped it.
On Examination
SPO2: 80% on room air, HR: 100bpm and BP:140/80mmHg, RR:30b\min
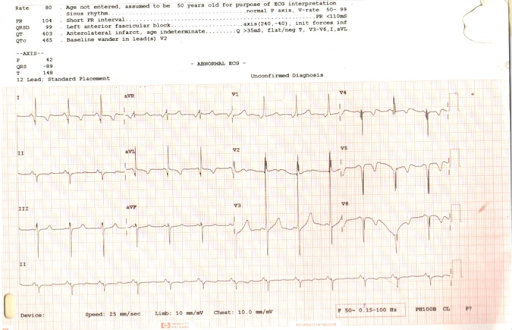
ECG
ECHO
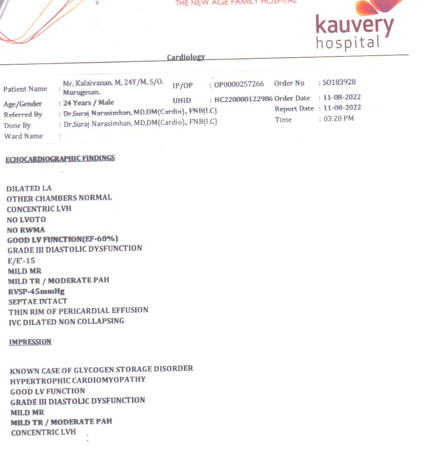
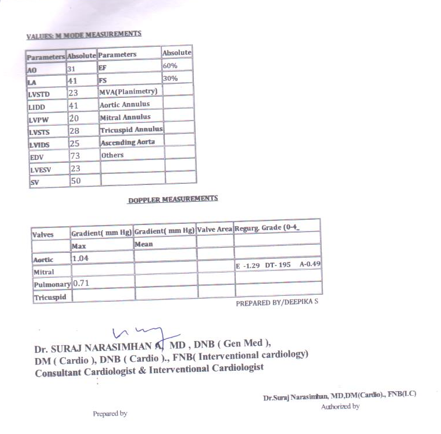
Shows Hypertrophic Cardiomyopathy good LV function, grade III diastolic dysfunction Mild MR, Mild TR / Moderate PAH, Concentric LVH.
USG
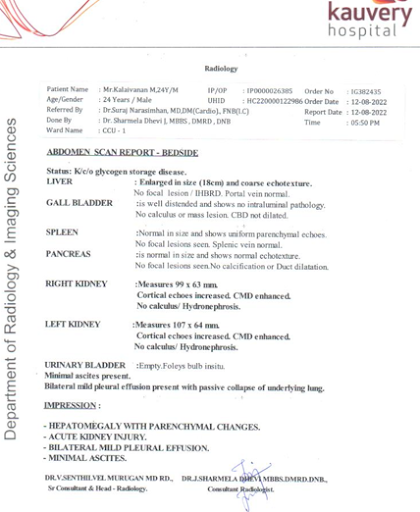
Shows hepatomegaly with parenchymal changes. Acute kidney injury bilateral mild pleural effusion, minimal Ascites.
Lab Reports
Shows elevated urea and creatinine.
As advised by the doctor, the nurse placed the patient on CPAP, started with inotropic drugs and stabilized. The family was explained about the critical condition of the patient and an informed consent was obtained for admission in CCU. As urea and creatinine level were increased doctor advised to start dialysis and patient underwent 2 cycles of dialysis.
Brief Discussion
Usual symptoms of GSD:
- Not growing fast enough
- Bruising too easily
- An enlarged liver
- Weak muscles
- GSD evaluation includes checking blood glucose levels and how the liver, kidneys and muscles are functioning.
The GSD is caused by genetic enzyme defect.
Medical Management:
The main treatment for a treated with anti-hypertensive, diuretics, antibiotics, PPI and other supportive measures. Patient symptomatically improved, tapered off from O2 and observed in ward. To maintained and monitored the vital signs. He is being discharged in a stable state.
Nursing Care
- Maintain interpersonal relationships with the patient and family members
- CPAP was maintained with adequate precaution to prevent device associated pressure effects on the skin.
- The nurses assessed the skin integrity of the patient on a daily basis to prevent dehydration skin tear and pressure points for bedsore.
- Necessary investigations were done on a daily basis to monitor his health improvement.
- The assigned nurses communicated with the patient reassuring him about his health status and gave him orientation to time place and person.
- Nurses coordinated with other health care professionals for care while doing X-Ray, arranging diet at the appropriate time and for other timely investigations.
- Nurses positioned him two hourly round the clock and provided back care and back massage like effleurage, petrissage, tapping and friction, for prevention of bed sore. Each nurse communicated effectively and developed a good rapport with the patient and attender and he cooperated well in his care.
- Nurses developed a home like environment for him to relax and encouraged him to sit on the chair with O2 support every day.
- Opinions were obtained from Nephrologist and orders were carried out respectively.
- Adequate hydration was maintained with oral liquids and IV fluids.
- Protein rich diet like raw egg white and crushed pulses were fed to him.
Discharge Medication:
Tab. Nicardia 10MG 1-1-1
Tab. Prazopress XL 5MG 0-0-1
Tab. Starpress XL 50MG 1-0-0
Tab. Dytor 10MG 1-0-1
Tab. Pantocid 40MG 1-0-0 (Before Food)
Syp. Cremaffin 15ML 0-0-1 (SOS)
Tab. Ursocol 300MG 1-0-1
Tab. Nodosis GST 500MG 1-1-1
Recovery
After a long stay in the hospital, patient became stable with the efficient care of nurses and went home happily with good prognosis

Ms. Jane Abishak Jz
Critical Ward Supervisorz

Ms. Mercy
Critical care ward Incharge

Ms. Priyadharshini
Critical Care Senior Staff Nurse

Ms. Akshaya
Critical Care Staff Nurse
