Left mediastinal tumor excision
A Kanimozhi1,*, Cesilipriya2, V. Yuvasri3, Ramya4
1Assistant manager Operation Theater, Kauvery Heartcity, Trichy, India
2Critical Ward Incharge, Kauvery Heartcity, Trichy, India
3Senior Scrub Nurse, Kauvery Heartcity, Trichy, India
4Staff Nurse, Kauvery Heartcity, Trichy, India
*Correspondence: +91 85086 98000; E-mail: nursing.heartcity@kauveryhospital.com
Background
Large mediastinal masses are rare, and encompass a wide variety of diseases. Regardless of the diagnosis, all large mediastinal masses may cause compression or invasion of vital structures, resulting in respiratory insufficiency or hemodynamic decompensation. Detailed preoperative preparation is a prerequisite for favorable surgical outcomes and should include preoperative multimodality imaging, with emphasis on vascular anatomy and invasive characteristics of the tumor. A multidisciplinary team should decide whether neoadjuvant therapy can be beneficial. Furthermore, the anesthesiologist has to evaluate the risk of intraoperative mediastinal mass syndrome (MMS). With adequate preoperative team planning, a safe anesthesiological and surgical strategy can be accomplished.
Various surgical approaches are available to access the mediastinal and thoracic cavity. In the surgical management of large mediastinal tumors, a midline approach through a sternotomy, or a lateral approach through a thoracotomy are most often utilized.
Case Presentation
A 45-year aged woman, euglycemic and normotensive, had complaints of dyspnea for the past 3 months. She had a history of prior admissions to Thanjavur Medical College and Rohini hospital for the same. She was admitted to Kauvery Hospital where she underwent thorough investigations.
Past History
There is no significant past history like TB, Asthma, HTN, and DM.
On Examination
CVS: S1, S2+
Temp: 98.6 °F, Pulse: 116 bts/min, RR: 8 breaths/min, SpO2: 98%
Pre-op erative investigations
| Investigation | Valves |
| Hemoglobin | 14.2 g/dl |
| PCV | 43 % |
| Total WBC count | 9400 cells/cumm |
| Urea serum | 13.2 mg/dl |
| Creatinine serum | 0.477 mg/dl |
| Sodium Serum | 140.1 mEq/L |
| Potassium | 4.07 mEq/L |
| Neutrophils | 60.1 % |
| Lymphocytes | 32.7 % |
| Monocytes | 6.5 % |
| Esonophils | 0 % |
| Basophil | 0.7 % |
| RBC | 5.03 ml/10^9 |
| MCV | 85.2 Fi |
| MCH | 28.3 pg |
| MCHC | 33.1 g/dl |
| Platelet count | 268000 cells /cumm |
| MPV | 8.0 |
| RDW | 12.9 |
| Bicarbonate | 28 mmol/L |
| HBs Ag and HCV Antibody | Negative |
| Bilirubin Total | 0.559 mg/dl |
| Bilirubin Direct | 0.234 mg/dl |
| Bilirubin Indirect | 0.324 mg/dl |
| SGOT | 26.4 U/L |
| SGPT | 22.9 U/L |
| Total Protein | 7.20 g/dl |
| Albumin Serum | 4.04 g/dl |
| A/G Ratio | 1.28 |
| Alkaline Phosphate | 103 |
| Gamma-Glutamyl transfer (GGT) | 13.2 U/L |
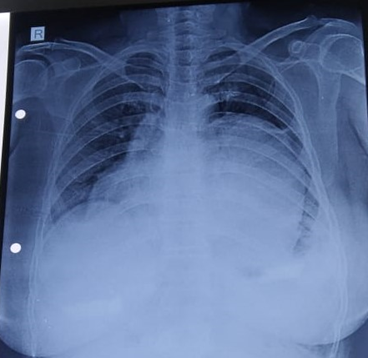
Pre- operative X- ray:
Post Ope rative X-ray

CT – Thorax Report

Impression
Well defined rounded mixed solid cystic calcified lesion was noted in the left half of superior and anterior mediastinum, partially extending into the medial mediastinum with following features:
- Superiorly: It is reaching upto the level of left lung apex.
- Supero-Laterally: It reaches upto the left anterior pleural surface without infiltration.
- Supero-Medially: Mass effect on the Mediastinal structures and pulmonary artery without infiltration, mass effect on the left main bronchus without obstruction, it measures 128 × 102 × 84 mm. Mass effect noted in trachea which is shifted on the right side.
ECHO Report
- Normal chambers dimension
- No RWMA
- Good LV function
- Valves normal
- No MR
- No TR/PAH
- Septae intact
- No pericardial effusion/Clot
Impression:
- Good LV function
- Poor ECHO window
- Anterior Mediastinal mass obscuring cardiac shadow
- Limited window shows normal cardiac chambers.
CT Scan guided biopsy
Indication: Anterior Mediastinal mass lesion.
CT Scan report
- Anterior Mediastinal mass lesion with both solid and cystic areas with peripheral wall calcification, to consider germ cell tumor.
CT Scan chest plain:
-
- Large well defined mass lesions in the posterior segment of right upper lobe.
Biopsy Procedure Notes
- Under strict aseptic precautions and using LACT guided biopsy done from the anterior mediastinum.
- Specimen obtained adequately.
- No procedural and post procedural complications.
- Patient stable after the procedure.
Operation Notes
- Large tumor 15 CM X 10 CM size occupied left thoracic cavity compressing left lung and Bronchus.
- Left phrenic nerve stretched and splayed out and buried with tumor mass.
- Left posteriolateral thoracotomy done through 5 th intercostals space.
- Lung tissue and adhesions released from tumor.
- Excision of tumor done.
- Chest drains placed.
- Chest closed in routine fashion.

Fig 1. Mediastinal mass

Fig. 2. Excision of Tumor
Post Operative Nursing Care
On “0” POD
- Patient conscious on the ventilator.
- Patient vitals were stable.
- She was managed with necessary supports Inj. Adrenaline – 0.1 ml
- Total ICD drain – 190 ml.
- Extubation was done and patient was in stable condition, after 2 h patient’s PCO2 level increased and she was again intubated and supports were added Inj. Noradrenaline – 1 ml.
- Patient’s condition was stable.
- Every 4 h patient was given back care and ET suctioning.
- Continuous close monitoring of the patient and the ICD drain was done.
On “1st” POD
- Patient vitals were stable.
- Supports Inj. Noradrenaline was weaned and stopped.
- Early in morning patient was given mouth care and combing done.
- Every 4 h once back care and ET suctioning were done.
On “2nd” POD
- Patient vitals were stable.
- Extubation was done.
- Early morning mouth care and nebulization were given.
- Intermittent CPAP was given.
- Every 2 h back care was given and position was changed.
- Chest physio and Spiro exercise were given.
On “3rd” POD
- Patient vitals were stable.
- Every 2 h back care was given and position was changed.
- Early morning mouth care and nebulization were given.
- Intermittent CPAP was given.
- Chest physio and Spiro exercise given.
On “4th” POD
- Patient vitals were stable.
- Every 2 hours back care was given and position was changed.
- Early morning mouth care and nebulization were given.
- Intermittent CPAP was given.
- Chest physio and Spiro exercise given.
- ICD, Arterial Line and CBD were removed.
- Patient was mobilized.
On “5th” POD
- Patient vitals were stable.
- Early morning mouth care and nebulization were given.
- Once in every 2 h back care was given and position was changed.
- CVC line was removed.
- Patient was shifted to ward.
Nursing Management
Cardiac monitoring
- Electrocardiography monitoring for 24 h minimum, 12 lead ECG post procedure and then daily.
Pain
- Patients pain was arrested using a pain assessment tool.
- The site was observed for abnormalities.
- Prescribed analgesia’s were given patient reassured and monitored.
- Patient was assisted into comfortable position.
- The medical team was notified of any abnormalities.
Assess site
- Direct site observation was done.
- Pulse checked (Dorsalis pedis, posterior tibia).
- The medical team was notified of any abnormalities.
- Clip removal as instructed by medical team was done.
Hemodynamic monitoring:
- Continuous blood pressure monitoring in the arterial catheter was done.
- Continuous monitoring of heart rate and rhythm was also done.
- The medical team was notified of any abnormalities.
- The blood gas analysis was monitored every 4th hourly (ABG).
Central venous catheter
- Catheter site was observed for any swelling or signs of infection.
- Temperature was recorded every 4 h.
- The dressing was constantly inspected for dryness.
- The site was observed for any bleeding/oozing.
- Normal mobility of arm was observed.
- Details were recorded in the hospital case file.
Respiratory
- Respiratory rate, depth and rhythm and chest wall expansion were monitored.
- Continuous pulse oximetry done.
- Skin was observed for cyanosis, warmth and perfusion.
- O2 was administrated as prescribed.
- The medical team was notified of any respiratory difficulty.
Urinary Catheter
- Catheter cleaning was done regularly as per hospital policy.
- It was ensured that the position of the drainage bag was above floor but below bladder level.
- Hourly urine output was monitored and recorded.
- On a Daily basis blood urea and creatinine were monitored.
Central Nervous System
- Monitored and recorded the neurological observations.
- Observed the patients conscious level and orientation to time and place.
- Observed for alteration in pupil size or reaction.
- Observed verbal and motor responses.
- The medical term was notified of any abnormalities.
Prevention of Infection
- Observed documented all invasive sites for signs of infection.
- Temperature was recorded every four hours.
- NM – Touch technique for all clinically indicated procedures.
- Hand washing was done as per protocol were administered.
- Intravenous antibiotics were administered as per standard protocol.
Conclusion
Patient received Left Mediastinal tumor excision. After surgical resection, she had excellent results.

Ms. A. Kanimozhi,
Assistant manager, Operation Theater

Ms. Cesilipriya
Nursing incharges

Ms. V. Yuvasri
Senior Scrub Nurse

Ms. Ramya,
Staff Nurse
