Our colleague’s SVT (Supra Ventricular Tachycardia)!
Hemalatha R1,*, Nancy Almeda E2
1Non Critical Ward Supervisor, Kauvery Heartcity, Trichy, India
2Nurse Educator, Kauvery Heartcity, Trichy, India.
Correspondence:+91 85086 98000;nursing.heartcity@kauveryhospital.com
Case Presentation
A 23 years old young nurse working at a Kauvery Hospital got admitted in Kauvery Heartcity, as a known case of Supra Ventricular Tachycardia, for Electro Physiology Study and Radio frequency ablation procedure.
The history of this young nurse is as follows: she had one episode of palpitation in the month of November-2022 while she was at her home. But she was unaware of these symptoms and it was auto reverted within 5 minutes. Again, she experienced the same symptoms of palpitation in the month of February-2023 while she was at her duty. ECG was taken under the guidance of Emergency physician and report was Sinus Tachycardia and then she was shifted to casualty for observation. ECG was taken at the casualty a second time and they found it was SVT (Supra Ventricular Tachycardia) and treated with Inj. Adenosine 6 mg/IV immediately.
Supraventricular tachycardia (SVT) is an arrhythmia that affects the upper chambers of the heart and causes an unusually fast or chaotic heartbeat. Paroxysmal Supraventricular tachycardia is another name for SVT.
The average heart beats between 60 and 100 times/min. Tachycardia are the medical term for a heart rate of greater than 100 beats/min. The heart typically beats 150 to 220 times/min during an episode of SVT, but it can occasionally beat faster or slower.
Definition
A narrow complex (QRS 120 ms) with a pace of more than 100 beats per minute characterizes Supraventricular tachycardia (SVT), a dysrhythmia that originates at or above the Atrio Ventricular (AV) node (bpm).
Types of SVT
Sinus tachycardia
Sinus nodal reentrant tachycardia (SNRT)
Inappropriate sinus tachycardia (IST)
Multifocal atrial tachycardia (MAT)
Junctional ectopic tachycardia (JET)
Nonparoxysmal junctional tachycardia (NPJT)
Symptoms
Palpitation
Giddiness
Examination:
CVS: S1 S2+ SAO2 – 99 RA
RS: BAE(+) BP – 80/60 mmhg
P/A: Soft HR – 86/min
CNS: Within normal limits RR – 20/mt
T – Normal
GCS – 15/15
GRBS – 98 mg/dl
Procedure Details
Surface ECG details
PR interval – 112 msec QRS interval – 86 msec
RR interval – 800msec QT interval – 390 msec
Under local anesthesia, catheters were placed at the appropriate location. Using 3D ENSITE
NAVIX mapping, RA geometry was created
Baseline measurements are as below.
V. Pacing : Concentric & Decremental,
VAW – < 200 msec
VERP – 600 / 250 msec
A Pacing : No pre – Excitation
AV cross over at 320 msec
Easily inducible clinical Tachycardia at burst pacing at 310 msec after AV crossover
AVNERP – 500 / 220 msec
Tachycardia: (TCL – 240 msec
1:1 AV ratio, concentric VA
Septal VA 10 msec
VOP – VAV response
CPPI – 150 msec
Diagnosis: Typical slow- fast AVNRT
Ablation details: with medium curve therapy ablation catheter in sinus rhythm, slow pathway region was mapped with 3D mapping. Ablation at that spot revealed stable functional rhythm for 60 seconds
Energy settings : 30w, 50deg C
Post Radio Frequency Ablation:
Baseline : PR – 110/msec HV – 42 msec, AH – 60 msec
Easily inducible AVNRT was not inducilbe with burst and extra atrial Stimulus (Double Extras). AH jump was present. No AV nodal Echoes.
Final Diagnosis : SVT- Typical AVNRT (Drug refractory) using 3D ENSITE NAVX mapping
Successful slow pathway modification done
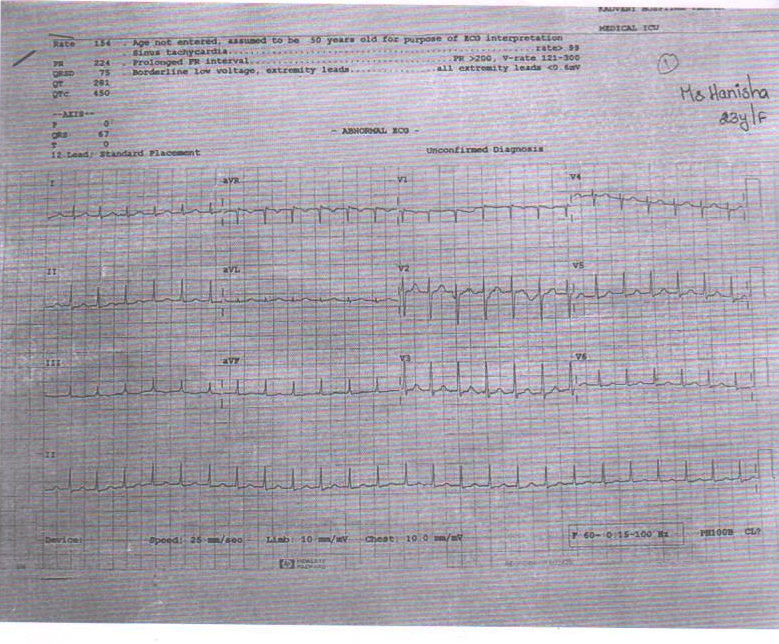
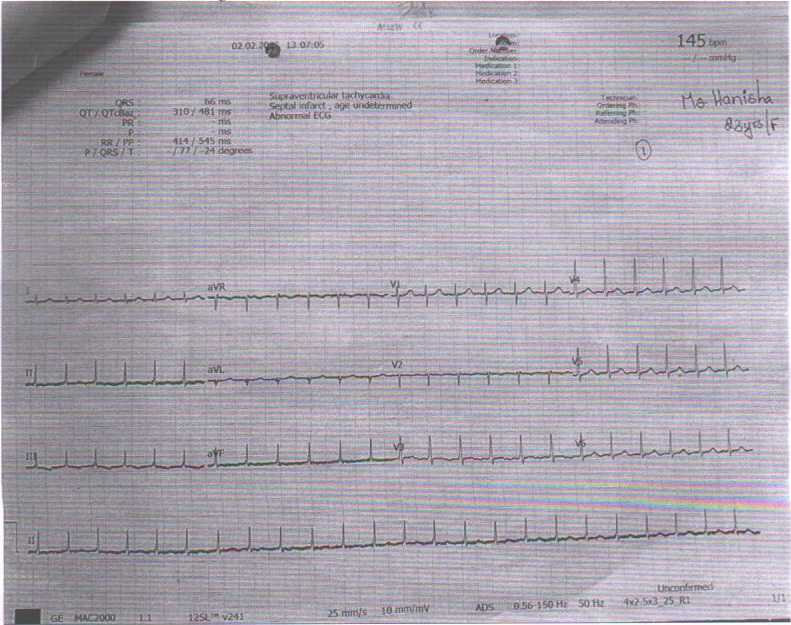
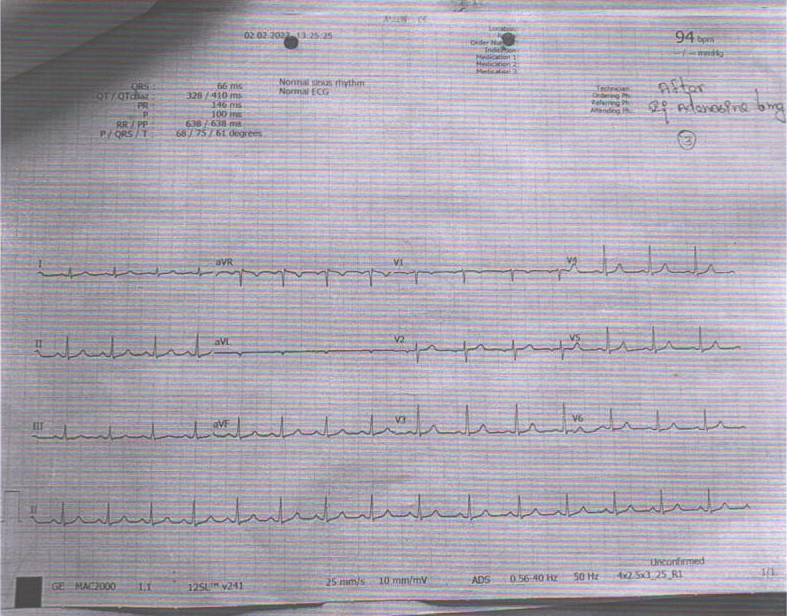
ECG:
1. At the time of palpitation in ICU
2. At the time of palpitation in Casualty
3. After treatment (Inj.Adenosine)
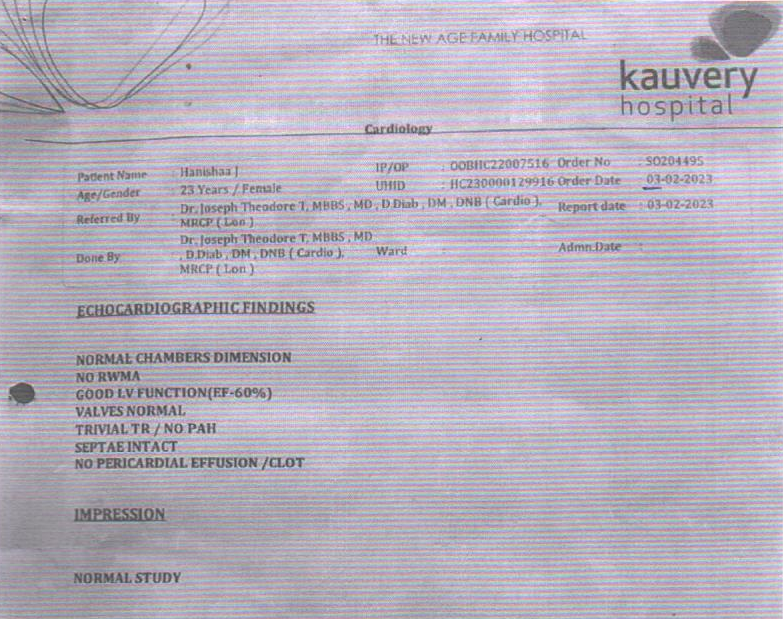
ECHO Report: 3.2.23
Nursing Management
Every four hours, blood pressure was monitored
Physicians gave attendees an explanation of the patient’s situation.
After thorough counselling, nurses were able to secure consent for the clinical procedures.
Whole body preparation done for the procedure.
Povidone bath given prior to the procedure.
When speaking with patients and visitors, nurses employed the AIDET strategy (Acknowledge, Introduce, Duration, Explanation and Thank you) to build trust and raise satisfaction levels.
The patient was moved to the Cath lab on 11/2/2023 for an electrophysiological investigation and radio frequency ablation.
The 3D ablation procedure was completed successfully.
Nurses kept an eye out for any hematomas or active bleeding at the femoral site
Vital indicators were closely checked both throughout the procedure and following it to avoid stasis and embolism formation.
Following the surgery, effective hydration and I/O chart maintenance optimised renal function.
Renal function was optimised following the procedure with effective hydration and I/O chart management.
Diversional therapy was supplied with newspapers, television and active listening to patient voice by nurses.
Discharge Medication
Tab. Rantac 150 mg BD
Tab. Ecosprin 75 mg OD
Outcome
On discharge: she was asymptomatic. Heart rate was 86/min. She went with full of happiness and she joined back to her duty within one week. Now she is leading a happy life without any problem.

Ms. T. Jasmine Rajareegam Princely
Non-Critical Ward Incharge, Kauvery Heartcity

Ms. R. Hemalatha
Non-Critical Ward Supervisor, Kauvery Heartcity

Ms. E. Nancy Almeda
Nurse Educator, Kauvery Heartcity
