C. Sugendhiran, A. Ramkumar, S. Kamalanayagi
Physiotherapists, Kauvery Hospital, Hosur
Role of physiotherapy in Bell’s Palsy at outpatient department
Abstract
Bell’s palsy is a form of facial paralysis resulting from a dysfunction of the 7th cranial nerve (facial nerve) that results in the inability to control facial muscles on the affected side
Background
Bell’s palsy is considered as a most common cause of one-side facial nerve paralysis (70%), it occurs 1 to 4 per 10,000 people per year. About 1.5% people are affected at same point in their lives. It most commonly occurs in people between the ages 15 to 60, and equally affects males and females. It is named after the Scottish scientist Charles Bell, who also described the connections of the Facial nerve.
The aetiology of Bell’s palsy may be idiopathic or attributable to infection, trauma etc.
Common symptoms and signs include wrinkles in forehead, drooping of eyelid, inability to close the mouth, lacrimation, loss of naso-labial fold, angle of mouth deviation and loss of sensation loss of anterior 2/3 of tongue
Most of the people that we receive in OPD will be prescribed medicines and Physiotherapy
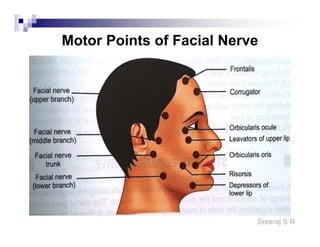
Anatomy of facial nerve
The facial nerve contains approx.10,000 fibres. 7000 are myelinated fibres that form facial expressions-motor functions. 3000 are fibres that form the nervus intermedius, a small branch of the facial nerve. The nervus intermedius is part of the facial nerve (cranial nerve VII) and is located between the motor component of the facial nerve and vestibulocochlear nerve (cranial nerve VIII).
It carries:
- Sensory fibres (anterior 2/3rd of tongue)
- Taste fibers from soft palate via palatine and greater petrosal nerve
- Parasympathetic to sub-mandibular, sublingual, lacrimal and parotid gland
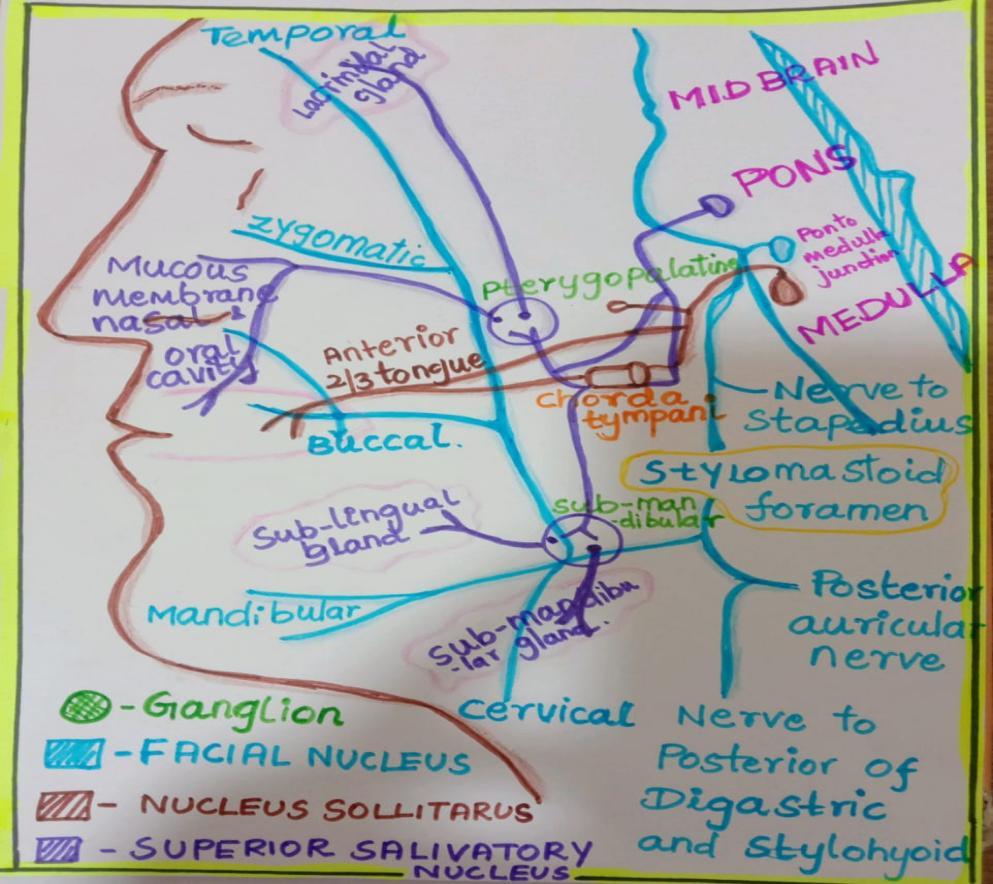
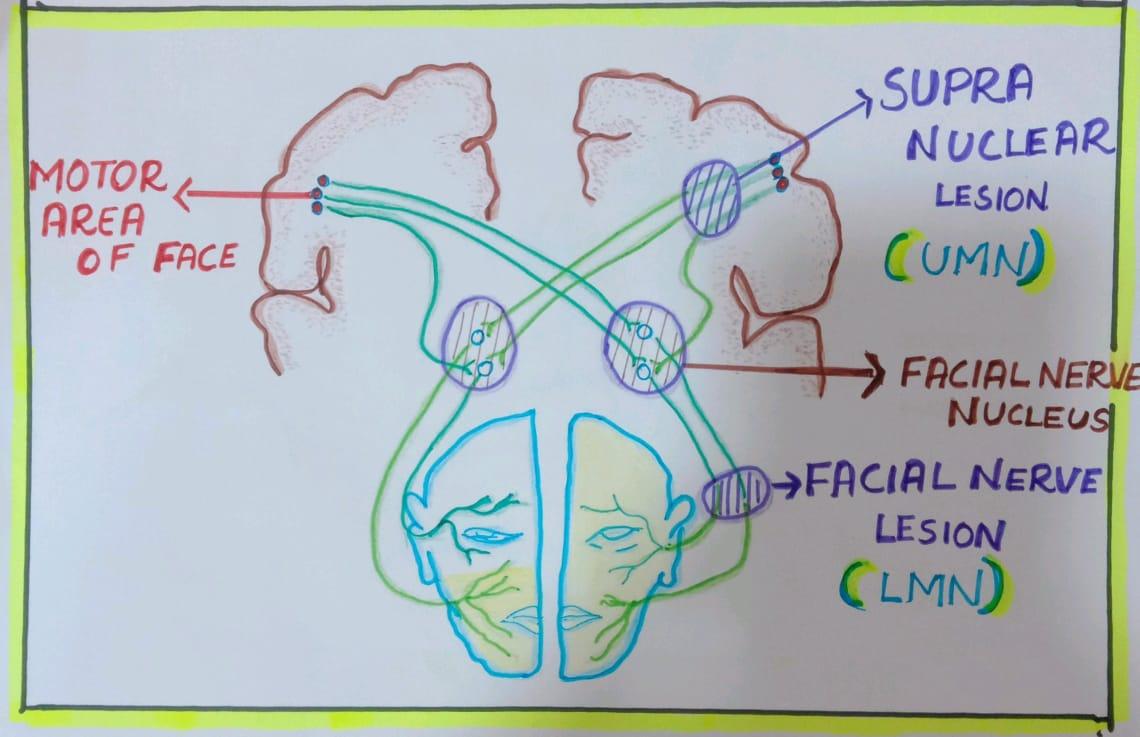
Clinical features of UMN and LMN facial Paralysis are attributable to loss of its function in:
- Upper face — crossed and uncrossed fibres
- Lower face — crossed fibres only
Case Presentation
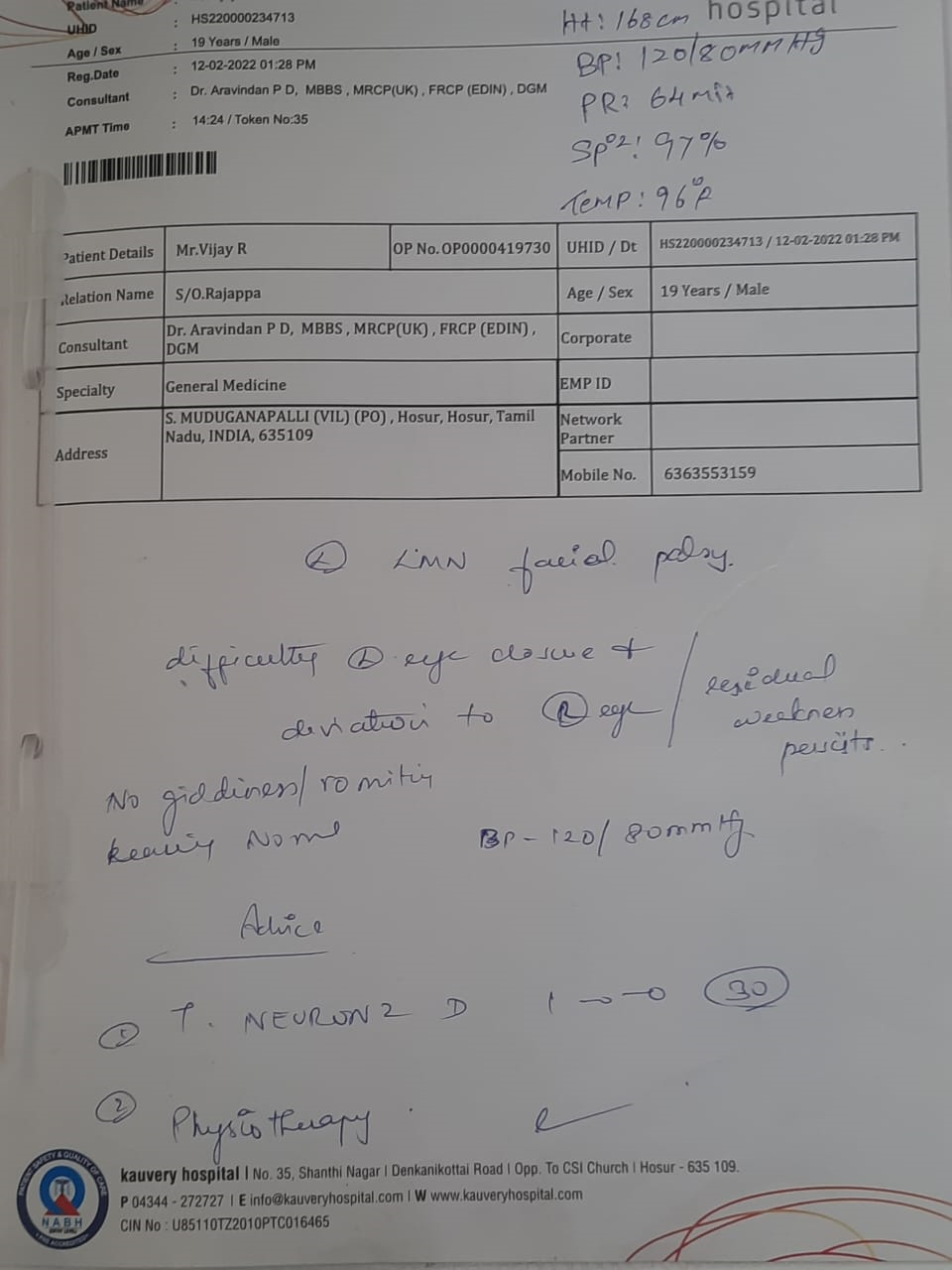
A 19 years old male patient came to hospital with complaints of weakness of the face on the left side. The patient was apparently normal till the previous evening, Next morning he developed weakness
H\o sudden deviation of mouth
H\o Inability to close an eye
He had taken a naturopathy treatment for two months. As there was no recovery he came to our hospital OPD for further management.
Vitals: BP:120/80 mm of Hg, SpO2: 97%
Course in the hospital
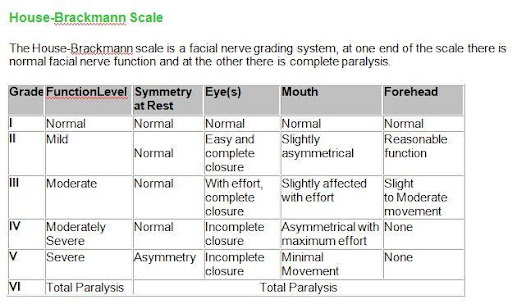
The patient came to OPD and was evaluated for his symptoms. Based on his symptoms the doctor diagnosed LMN palsy (grade IV), advised medicines and physiotherapy management.
Physiotherapy management for the patient
Assessment
- Muscle tone: Hypo tone
- Drooling: Present in left side
- Sensation: of superficial sensation in anterior 2/3rd of tongue
- Reflex: Corneal reflex absent
- Diagnosis: Left side Bells palsy (GRADE IV)
- Investigation: Strength duration curve (S D – graph that represent the response to stimulation of facial muscle- use of galvanic stimulation to identify the nerve lesion).
Management
List of complaints patient had:
- Weakness of facial muscles on left side
- Deviation of muscle movement (typically the angle of mouth) to right side
- Difficulty in chewing of food on the left side
- Difficulty in closing eye on the left side
- Redness in eye and lacrimation
Treatment
1. Electric stimulation — 30 contraction
Muscle of face — Galvanic stimulation
Nerve trunk — Faradic stimulation
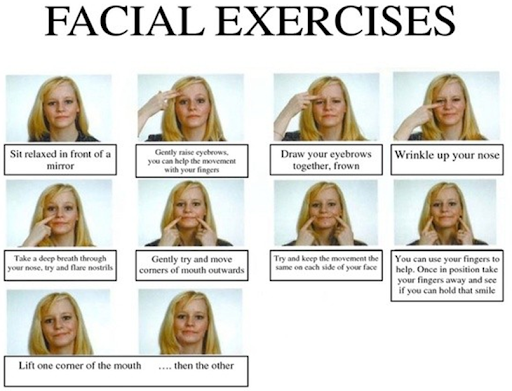
2. Facial Exercises – 10 count (3 times a day)
3. Facial Massage — Stroking, Effleurage, Picking up, Kneading, Rolling
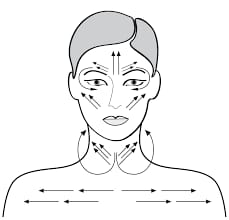


4. Facial Tapping — At night>


5. Resistance exercise to facial muscles



Advice for recovery
- Exercise the facial muscles regularly
- Apply moist heat to the paralyzed areas to help reduce pain.
- Massage affected area.
- Keep the face warm, wear a scarf because exposure to cold brings on paralysis.
- Eating healthy and balanced diet rich in leafy, green vegetables.
- Increase intake of Vitamin B12, B6 and zinc supplements to promote nerve growth.
- Manage stress levels by practicing relaxation exercises.
- Using a finger, regularly close the eye to keep it moist.
- Tape the eye closed for sleeping
- Cut food into small pieces and eat on the side of your mouth that feels most comfortable.
- Wear a pair of goggles when you shower to prevent soap and shampoo from affecting your weak eye
- Use protective glasses or clear eye patches to keep the eye moist and to prevent foreign materials from entering the eye.
Outcome of the patient
| HOUSEBRACHMANSCALE | GRADE | DESCRIPTION |
| PRE-TREATMENT
12/02/22 |
IV | MODERATELY SEVERE DYSFUNCTION |
| POSTTREATMENT
24/04/22 |
II | MILDDYFUNCTION |
Discussion
The patient came to OPD to start electrical stimulation, facial exercise, facial tapping and , resistance exercises which were given in detail, as mentioned above, during our management.
We advised him to come for regular treatment.
After 2 months we re-assessed the patient who had improved well, from to Grade IV – Grade II.
He was followed up weekly twice.
Then we advised to do exercise regularly for facial muscles, and following a month he recovered fully (grade 1)

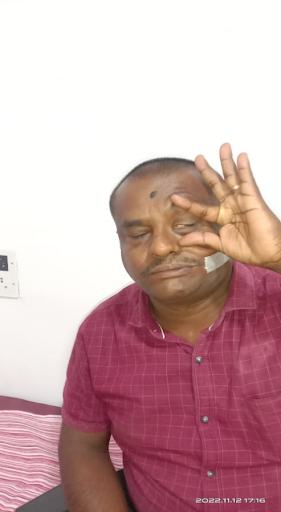
This is our patient Mr. Vixxx, 20y/m after treatment picture..
