Salicylate poisoning
Bini Susan Isaac*
Clinical Pharmacist, Kauvery Hospital, Salem, India
*Correspondence: +91 9497052726; clinicalpharma.khs@kauvery.in
Background
Salicylates are ubiquitous agents found in hundreds of over-the-counter (OTC) medications and in numerous prescription drugs, making salicylate toxicity an important cause of morbidity and mortality.
Salicylates are used as analgesic agents for the treatment of mild to moderate pain.
Aspirin, the most familiar Salicylate, is used as an antipyretic and as an anti-inflammatory agent for the treatment of soft tissue and joint inflammation and vasculitides such as acute rheumatic fever and Kawasaki disease [1].
Pathophysiology
The therapeutic range of salicylate concentration for anti-inflammatory effects is between 15 and 30 mg/dL. Concentrations higher than 30 mg/dL can be associated with signs and symptoms of toxicity.
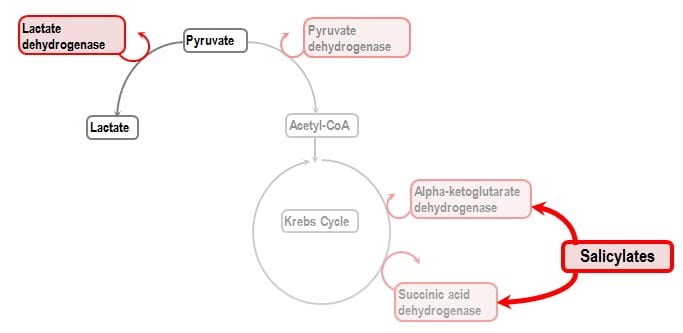
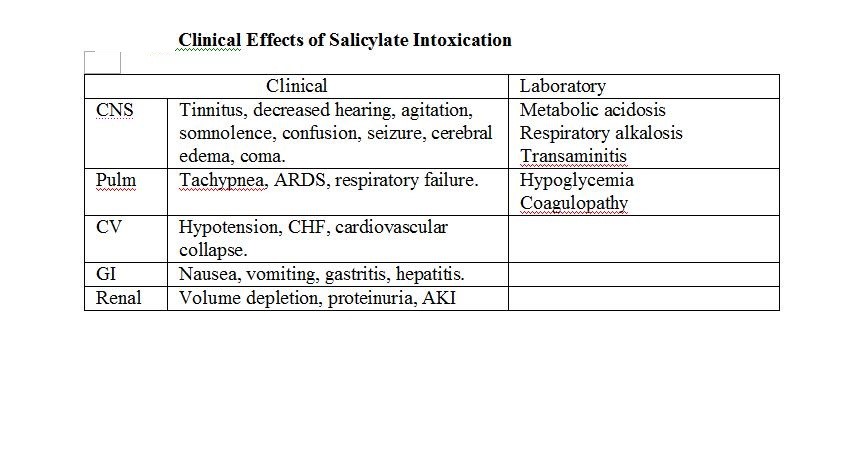
Salicylic acid acts to uncouple oxidative phosphorylation, leading to accumulation of lactic acid and pyruvic acid, causing a primary elevated anion gap metabolic acidosis.
Salicylic acid also directly stimulates the respiratory drive in the medulla, leading to a primary respiratory alkalosis.
Salicylic acid is a weak acid; it exists mostly in charged/ionized state at physiologic pH. As pH decreases, shifts more towards uncharged/ non-ionized state and can cross blood-brain barrier to worsen neurotoxicity.
Even at normal plasma glucose levels, salicylate toxicity causes decrease in brain glucose due to uncoupling of oxidative phosphorylation and compensatory stimulation of brain glycolysis. This can cause CNS effects of hypoglycemia at normal plasma glucose levels [2].
Diagnosis
- Serum Salicylate level
- Arterial blood gases (ABGs)
Salicylate poisoning is suspected in patients with any of the following:
- History of a single acute overdose
- Repeated ingestions of therapeutic doses
- Unexplained metabolic acidosis
- Unexplained confusion and fever (in older patients),
- Other findings compatible with sepsis (eg, fever, hypoxia, noncardiogenic pulmonary edema, dehydration, hypotension)
Patients Requiring Treatment:
- Acute ingestion ≥150 mg/kg
- All symptomatic patients
- Ingestion of unknown quantity
Resuscitation and supportive care
Standard procedures and supportive care
- Apnoea associated with intubation may worsen acidosis and lead to cardiac arrest. Consider pre-loading with sodium bicarbonate and obtain senior help.
- If ventilated, maintain alkalaemia (pH 7.45 – 7.5) to prevent redistribution of salicylate into the CNS. This may require setting the initial ventilator respiratory rate to the pre-intubation respiratory rate.
Decontamination
- Activated charcoal 1 g/kg. May be indicated in massive overdose, ideally within 1 hour of ingestion.
Correct fluids and electrolytes
- Rehydrate to euvolaemia
- Correct electrolyte imbalance
- Correct hypoglycaemia
Enhance elimination and treat acidosis
- Correction of metabolic acidosis is critical to limit CNS penetration
- Urinary alkalniization: IV bicarbonate infusion 1 mmol/kg/hr, after initial slow bolus of 2 mmol/kg, (keep urine pH >7.5). Urinary alkalinization requires a catheter, otherwise it is very difficult to monitor urinary pH in real time. This is to be considered in cases with symptoms of mild-moderate salicylism. Urinary alkalinization is not possible in the presence of hypokalaemia. Urinary alkalinization will also produce urinary potassium loss. Therefore, potassium must be replaced via intravenous administration to maintain a mid-range concentration.
- Haemodialysis should be considered early in moderate to severe salicylate poisoning as urinary alkalinization can be difficult to achieve and may not be effective Indications include but are not limited to:
- If urinary alkalinization is not feasible (eg renal failure, pulmonary oedema)
- Serum concentration >7.2 mmol/L (100 mg/dL) or rising to >4.4 mmol/l (60 mg/dL) despite alkalinization
- Severe toxicity: Altered mental state, refractory acidaemia or electrolyte imbalance, hyperthermia (temperature >39 oC despite active cooling measures) or renal failure [3].
Discharge criteria & follow up
Observe for 6 h and if remains asymptomatic, normal acid base status and concentration is within therapeutic range, discharge.
Take Home Points:
- Always consider salicylate toxicity
- In patients with tachypnea, hyperpnea, altered mental state and clear lungs
- In the presence of an anion gap metabolic acidosis with a respiratory alkalosis
- Treat salicylate toxicity by alkalinizing the blood and urine to increase excretion
- Avoid intubation until absolutely necessary. If you do have to intubate, minimize apneic time and consider awake intubation and make sure your ventilator settings match the patient’s necessary high minute ventilation
- Think about chronic salicylate toxicity in unexplained altered mental status, tachypnea or metabolic acidosis in elderly
- Know indications for hemodialysis in salicylate toxic patients
References
- Waseem M, et al. Salicylate toxicity treatment & management. 2022.
- Hoffman RS, et al. Goldfranks’s toxicologic emergencies (10th ed.) New York:McGraw-Hill Education. 516-527.
- Gerald F, et al. Aspirin and other salicylate poisoning. 2022.

Dr. Bini Susan Isaac
Clinical Pharmacist
