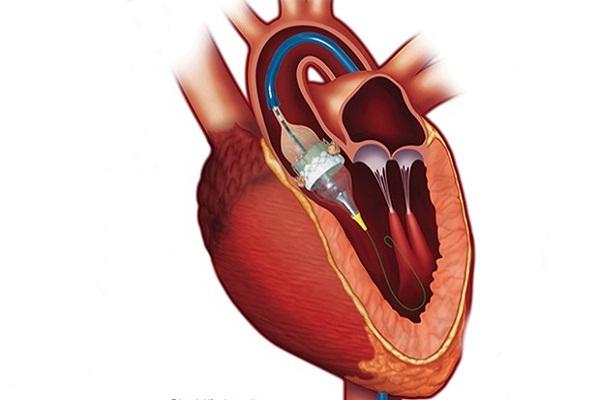
Transcatheter Aortic Valve Implantation (TAVI)
Shanthi R
Nursing Incharge, Kauvery Hospital, Tirunelveli, India
Abstract
TAVI stands for Transcatheter Aortic Valve Implantation. It’s a procedure that helps to improve a damaged aortic valve. TAVI is a common, mostly painless procedure. A narrow flexible tube (called a catheter) is put into a blood vessel in the upper leg or chest and is passed towards the aortic valve in the heart. The tube is used to fix a replacement valve over the top of the old one.
Background
A 77y /female patient, with h/o Hypertension but no diabetes, came for TAVI procedure.
H/o PTCA with stenting done to Distal LM to proximal LAD and proximal RCA on 02.08.23.
H/o Nephrectomy done on 2008.
H/o Hysterectomy done on 2018
Examination
- CVS: S1, S2 (+)
- RS: Bilateral air entry is present
- P|A: soft
- CNS: NFND
- Temp: 98.6 F
- SAo2: 90%
- BP: 140/90mmHg
- HR: 62 beats\min
- RR: 14breath\min
Pre-Op Investigations:
Blood Test
- HB: 11.5g/dl
- WBC Count: 6020 cell/cumm
- Platelet count: 234000cell/cumm
- PCV: 37.4%
- Test (PT): 14 sec
- Control: 30 sec
- INR: 1.09
- Urea: 27.7 mg /dL
- Creatinine: 0.89 mg /dL
- Potassium: 4.47 mEq/L
- Sodium: 138.2mEq/L
- RBC: 153mg/dL
- Bleeding time: 3 min 45 sec
- Clotting time: 5 min 00 sec
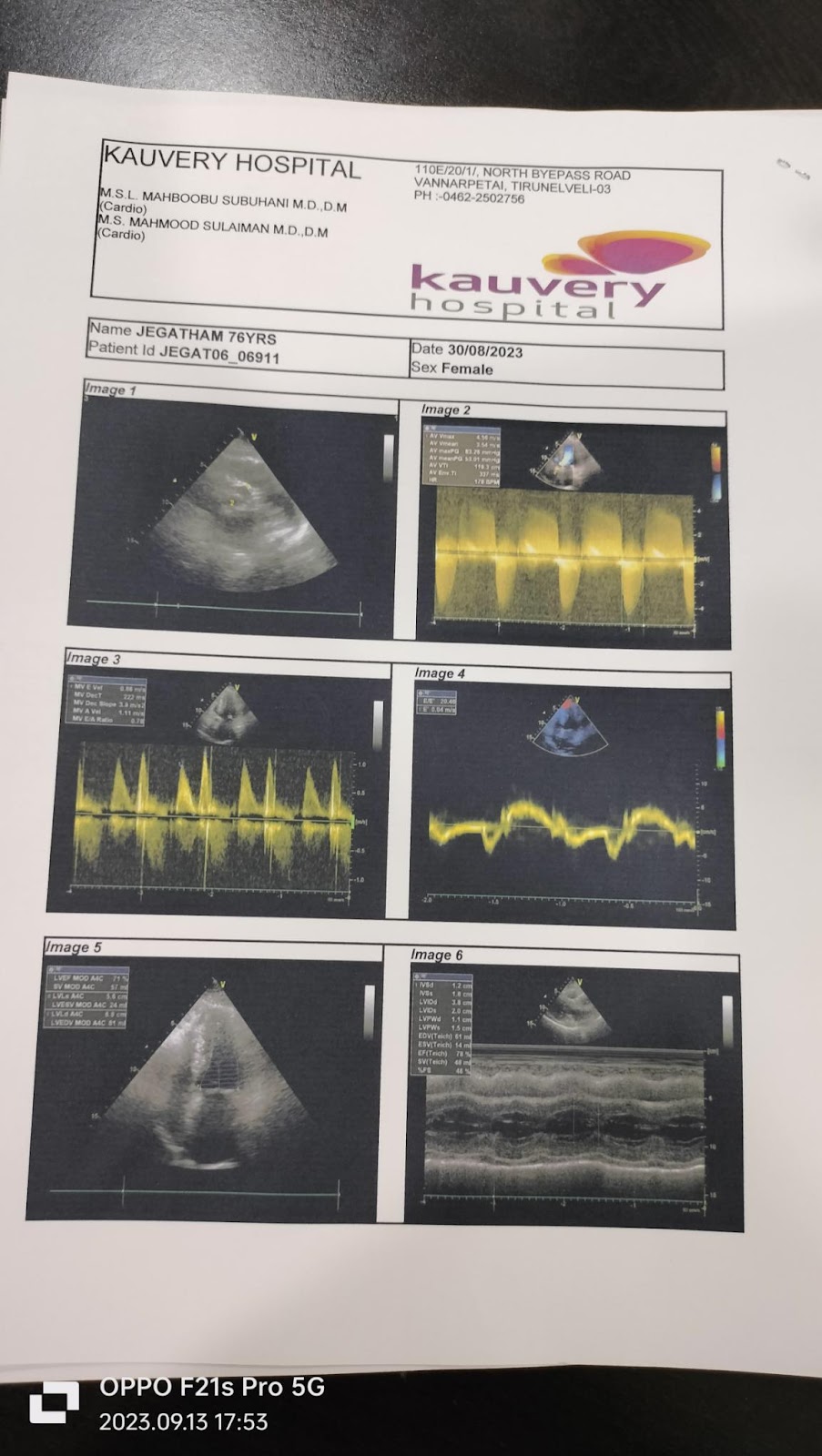
Echo
Bicuspid Aortic Valve Thickened, Calcified. AS (severe), AR (Moderate), Normal LV Systolic Function, Stage I Diastolic Dysfunction. LA dilated.
Blood test
- HB: 8.1g/dl
- Urea: 33.7 mg /dL
- Creatinine: 0.95 mg /dL
- Potassium: 4.43 mEq/L
- Sodium: 135.7mEq/L
- RBC: 129mg/dL
Procedure
RFA-6F Pigtail, RFV -TPI, LFA – Fluroguided (proglide XL)
6F-14F cover duplicate of superstiff wire. ALI Thermo Straight tip wire to cross AV- Exchange length J wire exchanged Pigtil -Hemodynamic access (AVG-60mmHg )
Predialated with 16/40 Z- med II balloon under rapid pacing 180 bpm in TPI.
23 mm Evolut R Implanted under fluro guidance in cusps overlap explainer view. LFV Access closed with Proglide XL, and angio seal 8f *1. TPI secured – RFV /RFA stenting secured.
Course in the hospital
Patient was planned for Trans catheter Aortic Valve Implantation on 31.08.23 under general anaesthesia. Post procedural vitals stable. Antiplatelets, Antithyroid, H2 receptor blocker, antibiotics antiemetics, diuretics, B-blocker, statin given. CBC was daily HB -8.1g Hematinic injection was started. Temporary pace maker removed on 02.09.23. Investigation taken Hemoglobin level improved. Patient general condition improved.
Post Procedure investigation:
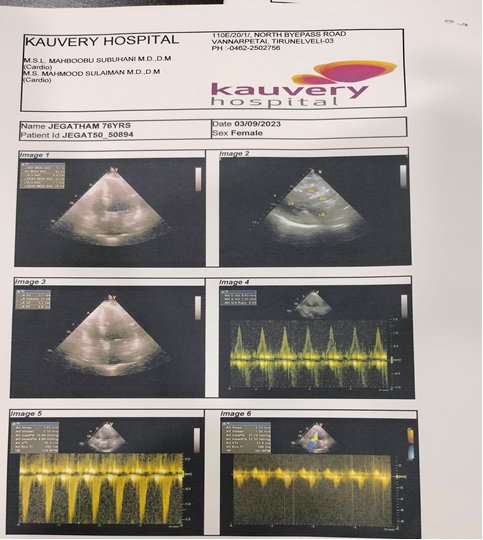
Echo
Aortic Prosthetic valve in situ Functioning normally. Normal LV Systolic Function stage I Diastolic Dysfunction.
Treatment
- Inj. Cefriaxone-750 mg TDS
- Inj. Rantac-50mg -TDS
- Inj. Emeset -4mg – BD
- Inj. Dytor-10mg -OD
- Tab. Revolol XL -25mg-OD
- Tab. Clavix As -75mg -BD
- Tab. Rozat -20 mg -HS
- Tab. Glycifer NR -TDS
- Tab. Thyroxine 25mcg-OD
Nebulization
Neb: Budecort -1Res-TDS
Neb: Duoline -1Res-TDS
Diet advice
During post-operative periods, initiate the liquid diet. After that, semi solid, solid diet and normal diet was given to the patient. Patient was tolerated well.
Eat heart-healthy foods

Nursing management
- Walking is a good exercise for the lungs and heart. Advised to take it slowly at first.
- Do not do any activity or exercise that causes pulling or pain across your chest, (such as using a rowing machine, twisting, or lifting)
- The patient and family were provided with information that will enable them to co-operate with the care and restrictions required to preparation them to return home.
- Educated the patient and family Wash your hands with soap and water
- Taught the use of assistive devices or modification of the home environment to help improve the health.
Follow up appointment
The patient and family are reminded of the Importance of Following recommendation and keeping with follow up appointments with health care providers for monitoring of risk factors.
Outcome
Patient was hemodynamically stable. On Discharge.
