Vascular Access Management (VAM) training program for nurses
Improving the Knowledge, Confidence, and Skills of Kauvery Nurses in Peripheral Intravenous Catheter Insertion
D Kavitha*
Manager, Clinical Governance and Quality, Kauvery Hospitals, India
*Correspondence: +91 77088 69499; kavitha@kauveryhospital.com
Abstract
Introduction: Peripheral Intravenous Cannulation (PIVC) is a common invasive procedure for most patients coming to a healthcare setting. About 90% of hospitalized patients receive IV infusion therapy as part of their treatment. An expert is required to secure good venous access.
Need for the program: The need for an exclusive Vascular Access Management (VAM) training program is to exclude all variations starting from the selection of an appropriate iv access to the maintenance of the IV line. At any given point, in the hospital, up to 50% of peripheral IVs don’t meet their therapy goals largely due to complications like infections, phlebitis, occlusion and infiltration. 89% of central line-associated bloodstream infections occur after 4 days of insertion.
Objectives: The vascular access goals and objectives include: i. Patient safety and experience: Improve PIV dwell time and decrease the risk of Vascular Access Device (VAD) related complications and improve the patient experience ii. Clinical and economic outcomes – Standardization of vascular care and achieving cost efficiency iii. Clinical competency and efficiency – Continuous improvement in competency of vascular care delivery.
Participants: A total of 59 participants underwent the VAM programme in two batches, 30 in the first batch and 29 in the second batch.
Survey and Training program: A comprehensive study was conducted to obtain a baseline of the current vascular access processes in the facility. The training program was conducted for three days of time, post the initial assessment.
Results: It was found in the pre-test that 68% of nurses were rated poor knowledge, 23% with moderate knowledge and 9% of nurses with good knowledge. After the infusion update and training, it was found that 98% of nurses were rated with good knowledge and 2% of nurses with moderate knowledge in the post-test. The training also showed a significant difference of p < 0.05 in the phlebitis grade.
Conclusion: Infusion experts play a vital role in phlebotomy and maintenance of IV lines and the study paved to fulfil the nursing vision of safe and effective infusion nursing, by following the best practices in our hospital.
Keywords: Intravenous cannulation, knowledge, practice, infection control, training program, peripheral intravenous cannula.
Background
PIVC (Peripheral Intravenous Cannulation) is a common invasive procedure in all hospital settings. It is the method of an insertion of a flexible plastic devise with a stylet available, inserted into the vein for the therapeutic and diagnostic purposes, successfully Nurses have a vital role in performing PIVC. It is the most efficient and effective way to deliver medications directly to the circulation. Trainers impart nurses the necessary knowledge and practical skills to succeed in this procedure, with minimum complications and maximum benefits to the patient, with positive clinical outcomes.
Peripheral Intravenous cannulation (PIVC)-related infections are associated with increased morbidity, prolonged hospitalization and increased costs. Nurses should maintain meticulous care during and following the insertion of PIVC to reduce the risk of infection. If nurses are not competent enough in the insertion of intravenous cannula there may be chances of developing complications like fungal and bacterial infections, dis-lodgement, leakage, infiltration, extravasation, thrombophlebitis, and vascular wall damage all of which result in in delay in treatment. So the comfort and safety of the patient, and successful insertion of the cannula in a first attempt, are of utmost importance.
Need for the study
The need for a Vascular Access Management training program is that there are variations in the maintenance of the IV line which increases the risk of complications. The need to improve care and maintenance of IV lines are:
- Up to 50% of peripheral IVs don’t meet their therapy goals largely due to complications like infections, phlebitis, occlusion and infiltration
- 89% of central line-associated bloodstream infections occur after 4 days of insertion.
- It is reported that more than 250,000- 500,000 intravascular-related bloodstream infections (BSIs) result in a mortality rate of 12-25%.
- It is estimated that the annual cost of treating patients with catheter-related BSIs may be as high as $ 2.3- 28 billion.
Stringent compliance with evidence-based guidelines during insertion of PIVC and catheter care has proven significant benefits in reducing BSIs.
Objective
The objective of the program was to determine the level of knowledge and the standard of prevailing practices in IV cannulation and to instill best practices in infusion among the nurses in Kauvery Hospitals. The program was offered in collaboration with BD company in accordance with the guidelines of the Infusion Nurses Society (INS). It aimed to develop expertise in our Peripheral IV Cannulation teams (IV access team or VAM team) in all our units, which shall help to prevent peripheral line-associated bloodstream infections and complications like infiltration, hematoma, extravasation etc., due to lack of knowledge and skills in IV cannulation technique and management. The cannula site was monitored and maintained using the tool Visual Infusion Phlebitis scoring chart (VIP scoring chart). The program aimed to prevent bad experiences for patients from painful cannulation, multiple pricks and complications.
We ensured that all nurses in our organization were trained to be experts in safe injection and infusion practices.
Vascular access goals and objectives:
- Patient safety and experience – Improve PIV dwell time and decrease the risk of Vascular Access Device (VAD) complications, improving patient experience.
- Clinical and economic outcomes – Standardization of vascular care and achieving cost efficiency.
- Clinical competency and efficiency – Continuous improvement in competency of vascular care delivery.
Materials and Methods
Survey/Assessment: A third-party audit was conducted to get the baseline data. A total of four hundred IV cannulations were evaluated based on the IV therapy monitoring charts maintained by the nurses. The audit was conducted by three persons in two hospitals at four care settings over four days. The audit was done by four methods: interviews, site assessment, practice observations and PIV records and it was conducted as followed:
- 67 staff members were interviewed
- 27 central lines were assessed
- 12 peripheral line insertions were assessed
- 67 PIV records were reviewed
- 70 patients were interviewed
- 116 peripheral lines were assessed
- 13 medication administration procedures were observed
Major observations observed during the survey were:
- Lack of adherence to sterility during IV cannulation procedure
- Lack of using appropriate PPE
- Lack of IV flushing protocol, backflow of blood and fluids found in the three-way extension and the IV cannula.
- Lack of monitoring and maintaining IV cannulation site using VIP (Visual Infusion Phlebitis scoring chart.
- The report showed 65 % of adherence and 35% of non-adherence in practicing the prevention of peripheral line-associated bloodstream infections
- The facility’s average dwell time was 68.71 hours/ 2.86 days whereas the recommended dwell time was 144 hours/6 days. It was found that 18% of IVs were removed within 24 hours.
- The estimated current cost of vascular access complications at Kauvery Hospital is 12000 x 385 = Rs.4,620,000 per year. This cost was estimated based on the Catheter cost + Dressing + Disinfectant + Process + Nursing time.
Vascular Access Management Training Program: VAM program is a three-day training program organized for our Nurses of Trichy units, ten nurses from each unit, a total of thirty nurses for each batch. This program was organized by the BD trainers and was coordinated by nursing leaders.
Batch 1: The training program for the 1st batch was started on March 2022 with 30 participants and the Sessions were scheduled from 9 am to 5 pm.
Batch 2: The 2nd batch was organized in June 2022 for 29 nurse participants.
Batch 3: The 3rd batch was organized in August 2022 for 30 nurse participants

Fig 1. Participants attending the VAM training program.
The topics covered in the three days sessions are as follows:
Day 1: Introduction to IV cannulation, challenges in IV therapy, anatomy and physiology of veins, the significance of the selection of size and the site, physiochemical properties and IV flushing protocol.
Day 2: Patient consideration during the IV therapy, initiation of therapy, dressings and aftercare of catheter.
Day 3: Managing complications and fundamentals of infection prevention and practical skill training using dummy arm on IV cannulation & infusion therapy.
The vascular access process that was covered during the 3 days program were:
- Selecting the right device
- Preparing the skin
- Placing the catheter
- Protecting the catheter
- Connecting to the catheter
- Maintaining the catheter safely



Figs. 2 and 3. Glimpse of VAM Programme.
Pre-test and post-test were conducted for the participants.
Later ten IV cannulations from the delegates were evaluated to see the effectiveness of the training. The evaluation was based on the Visual Thrombophlebitis Score (VTS) and the rate of grades of phlebitis.
Results
The knowledge gained from the program by the nurses on safe infusion practices were evaluated at the end of the training program by Post-test and OSCE observation of nurses on the practical skill of performing IV Cannulation.
It was found in the pre-test that 68% of nurses were rated poor knowledge, 23% with moderate knowledge and 9% of nurses with good knowledge. After the infusion update and training, it was found that 98% of nurses were rated with good knowledge and 2% of nurses with moderate knowledge in the post-test. The training also showed a significant difference of p < 0.05 in the phlebitis grade whereas in pre-evaluation grade 3 phlebitis was found but after training grade 0 had increased, which indicated an improvement in the IV cannulation practices.
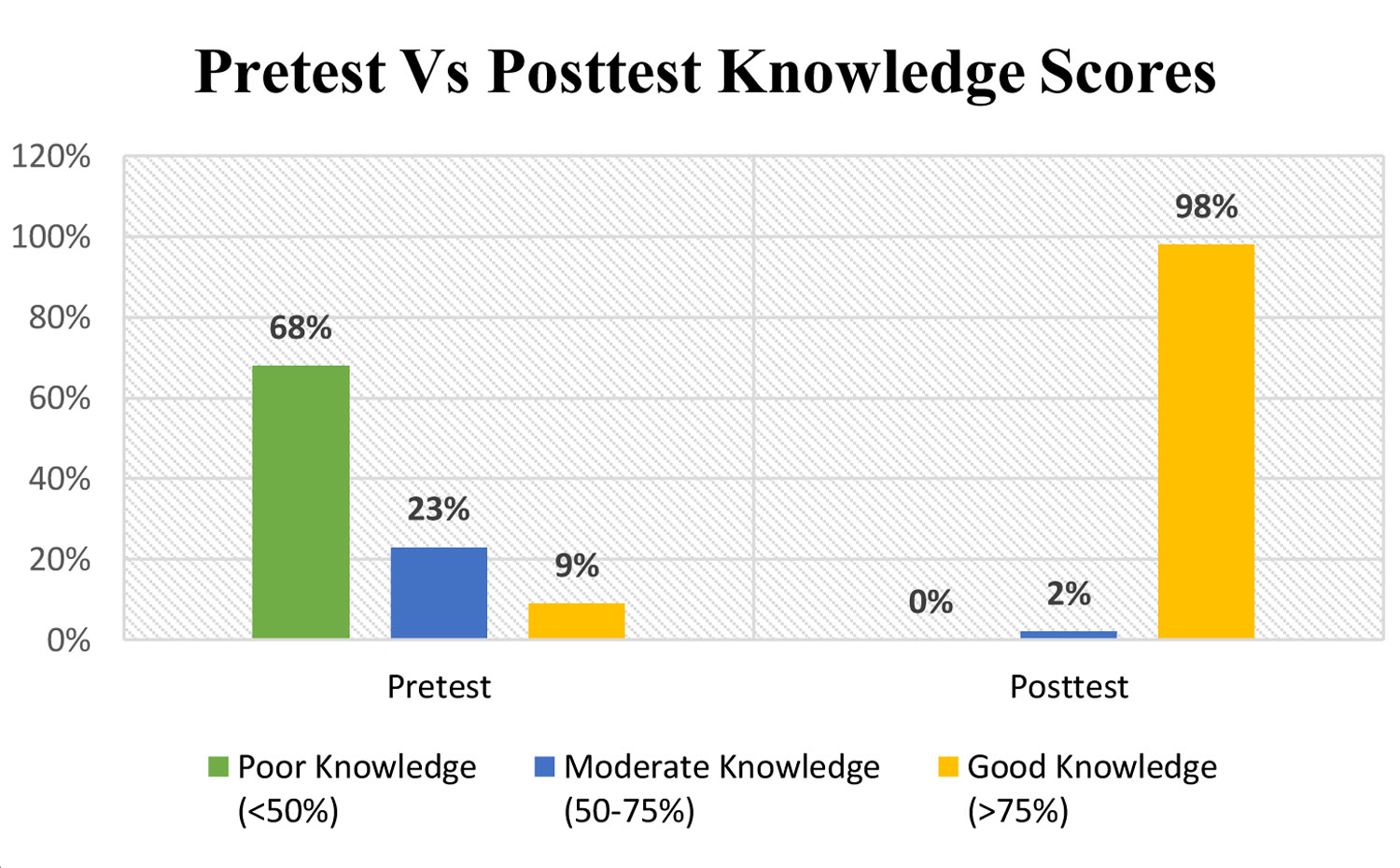
| Knowledge Assessment | Poor Knowledge (<50%) |
Moderate Knowledge (50-75%) |
Good Knowledge (>75%) |
| Pretest | 68% | 23% | 9% |
| Posttest | 0% | 2% | 98% |
Conclusion: Infusion Nursing is a nursing specialty that is the need of the hour to ensure patient safety and good clinical outcomes. Nurses skilled in safe infusion practices maintain high standards in phlebotomy and maintenance of IV lines. The study paved to fulfil our nursing vision of offering to our patients the best practices in IV infusions at our hospital
This study concluded that knowledge and practical skills in IVC should be continuously updated by such Continuing Nursing Education and Skill Development programs that promote standardized care.
Acknowledgement
We express our gratitude to our Managing Director, Group Medical Director, Medical Administrators, Nursing Heads, Infection control consultants, Learning & Development team and course coordinators for the successful implementation of this programme. A special thanks to the BD organization and the trainers for making this training a grand success. We take this opportunity to express our sincere gratitude to the entire nursing team.
References
- Asha Aniyan T, Sartaaj Perveen. A study to assess the knowledge and practice regarding intravenous cannulation among staff nurses in selected hospital New Delhi. Int J Nurs Midwif Res. 2016;3.
- George K, Muninarayanappa B. Effectiveness of structured teaching program on knowledge and practices of staff nurses on prevention of intravenous cannulae complications. Arch Med Health Sci. 2013;1:115-9.
- Gulcan Bahcecioglu Turan. Nursing students levels of knowledge on the prevention of intravascular catheter infections. Int J Caring Sci. 2018;11(1):443.
- Hossain AM, et al. Assessment of the level of knowledge and practice on intravenous cannulization among staff nurses of selected tertiary care hospital in Dhaka city. MOJ Public Health. 2016;4(5):156-9.
- Jyoti Kapoor. A descriptive study to assess the knowledge and knowledge on practice regarding peripheral intravenous infusion among GNM (Nursing) 3rd Year Students At AMT School, Bakshi Nagar, Jammu. Int J Adv Res Developm. 2017;2:269-71.
- Jaya Thanga Selvi G. A study to assess the knowledge and practice of nursing personnel regarding intravenous therapy and its selected complications. Int J Nurs Healthcare Res. 2017;1(1):19-22.
- Lalit Shree Sharma, et al. The knowledge and practice regarding intravenous cannulation and its complications: A narrative review. Int J Adv Sci Res. 2019;4:78-81.
- Pankaj Punjot, et al. A study to assess the effectiveness of infusion experts on the nursing interventions of peripheral intravascular devices among patients admitted to a tertiary care hospital of the city. Int J Nurs Res 2018;4(3):171-175.
- Moureau N. Preventing peripheral intravenous line infections. Recommendations for health care facilities. JAVA 2009;14(4):187-90.
- Abd El-Aziz A. Variations in aseptic technique and implications for infection control. Brit J Nurs 2009;18(1):26-31.

Ms. D. Kavitha
Manager, Clinical Governance and Quality
