
Vein Graft Procedures/for Dialysis
Dialysis, also called hemodialysis, is the most common treatment for kidney failure. A dialysis machine is an artificial kidney designed to remove impurities from your blood. During , blood is drawn from the patient through the dialysis access already created and is connected to the dialysis machine so it can remove impurities and regulate fluid and chemical balances. The purified blood is then returned to the patient again through the dialysis access.
Creating the access portal is a minor surgical procedure. There are two types of portals placed completely under the skin:
Arteriovenous Fistula
A surgeon creates an arteriovenous fistula by making a connection between an artery (which carries blood away from the heart) and a vein (which carries blood back to the heart). This artificial connection allows the vein to become larger and for the walls of the vein to thicken, a process termed maturation. A mature fistula makes it easier for the vein to be punctured repeatedly for dialysis. Maturation typically takes three to six weeks to occur, but in rare cases, can take longer. This makes advance planning for an arteriovenous fistula important. When a patient is felt to be approximately a year away from requiring dialysis, the patient should be referred for evaluation for possible creation of an arteriovenous fistula. Arteriovenous fistulas are usually created between radial artery and the vein at the wrist. It can also be done at the fore arm as well as the elbow. An arteriovenous fistula is the preferred type of vascular access due to lower rate of infection and clot formation, resulting in greater longevity than other types of vascular access. However, not everyone is a good candidate for an arteriovenous fistula, particularly older patients and patients with small veins or those who have blocked veins in the upper limb due to previous intravenous injections.
Arteriovenous Graft
If a patient is not a good candidate for an arteriovenous fistula, an arteriovenous graft is considered. An arteriovenous graft is a piece of artificial tubing, generally made out of teflon or fabric, that is attached on one end to an artery, and the other end to a vein. The tube is placed entirely under the skin and the tube itself is punctured during dialysis. An arteriovenous graft can in general be used two to three weeks after the operation. However, arteriovenous grafts are more prone to infection and clotting than fistulas. The lifespan of an arteriovenous graft is approximately two to three years.
Carotid Artery Surgery

Carotid artery surgery is a surgery to restore blood flow to the brain. It is a treatment for carotid artery disease and can help prevent a stroke. Carotid artery surgery involves removing plaque build-up from the carotid arteries.
Carotid artery disease, also called carotid artery stenosis, is a narrowing of the carotid arteries. There are two carotid arteries, one on each side of the neck. They are major arteries that carry blood from the heart to the brain. Carotid artery disease is caused by arteriosclerosis, also called hardening of the arteries. Also called Atherosclerosis, it is a build-up of plaque. Plaque is a sticky, waxy deposit of fats, cholesterol, calcium, and fibrous material. This causes reduction in the blood flow to the brain or can sometimes throw a clot into the brain. This leads to damage to the nerve cells of the brain resulting in stroke.
Symptoms of a stroke
- Slurring of speech
- Deviation of mouth
- Weakness of upper or lower limbs
- Sudden loss of vision
- Rarely giddiness.
Investigations
Presence of a block in the carotid artery can be easily detected by a Doppler study. This can indicate the degree of block and help to decide about need for surgery. Angiogram is done to get a road map of the artery and to plan treatment.
Treatment
In early stages carotid blocks can be managed with good medical treatment. Medical treatment includes blood thinners, anticholesterol medications, good control of diabetes and hypertension and strict abstinence from tobacco.
Types of carotid artery surgery
Carotid endarterectomy: involves opening the carotid arteries in the neck and removing the inner lining that is diseased or damaged by plaque. A patch graft may be placed to help widen the artery and improve the blood flow.
Carotid artery angioplasty and stenting: is an option for patients who have a high risk of complications for carotid endarterectomy.
Aortic Aneurysm
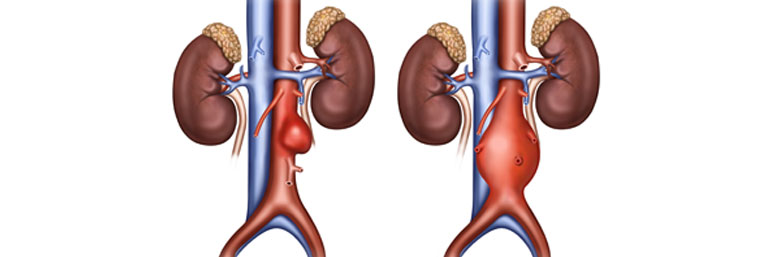
The word “aneurysm’ means out-pouching or bulging of a portion of a blood vessel that can occur anywhere in the body. When an aneurysm occurs in the aorta, the largest blood vessel in the body, it is either a thoracic aneurysm, located in the chest, or an abdominal aneurysm. The elastic fibre in the vessel wall can undergo damage and become weak. This causes the wall to bulge resulting in an aneurysm. The size continues to increase because of the blood pressure and when it reaches a critical size, it ruptures, just like a blow-out. This can be a life-threatening emergency. The goal of surgery is to intervene before that happens by removing the dilated portion of the vessel and replacing it with a graft-a tube of synthetic material, that won’t rupture or tear.
Causes
- Atherosclerosis (Cholesterol deposition in the wall of the arteries)
- Chronic or untreated high blood pressure
- Smoking
- Injury (for example, a car accident)
- Congenital abnormality (present from birth)
- Inherited conditions (for example, Marfan syndrome)
These are all the conditions that have the potential to weaken the wall of the vessel, allowing it to dilate or balloon out over time.
Symptoms
Aortic Aneurysms usually do not cause symptoms until they get quite large. They often are found during an examination for a different medical condition. When they are large enough to cause symptoms, people may notice a pulsating mass in the abdomen, chest or abdominal pain, back pain, palpitations, fatigue, dizziness or shortness of breath. Sudden, severe abdominal or back pain-that feels like the worst pain anyone has ever had-is usually a sign of a tear or rupture and is an extreme medical emergency.
Diagnosis
Large aneurysms can be seen on a chest or abdominal x-ray. They are also detected by studies such as routine ultra sound abdomen, CT scan, MRI, or echocardiography. These studies also help to determine the exact location and size of the aneurysm. When a small aneurysm is found, the study used to find it is repeated on a regular basis, usually every six to twelve months, to monitor any change in size. This helps determine the ideal time for surgical intervention.
Surgery is usually advised if the aneurysm is
- Larger than 5.5cm
- Growing by more than 1cm per year
- Causing pain
Treatment
Surgical repair involves removal of the diseased portion of the aorta. Clamps are placed above and below the aneurysm, which is then cut out and removed. A fabric tube, or graft , is sewn onto both cut ends, to replace the diseased portion that is removed.
Minimally invasive surgery for aortic aneurysms
There is another technique for repairing an aortic aneurysm that can be used for patients who are at a high risk to undergo major surgery. This involves placing a device called a “stent graft” inside the diseased portion of the aorta without opening the abdomen or chest. The stent is placed inside the aorta through a catheter, which is put through an artery leading to the aorta usually from the groin. This stent graft can relieve most of the pressure of the blood flowing through the aneurysm, preventing rupture.

